To the Editor:
The formation of professional identity is a central goal in medical education 1. It must encompass both professional competence and core principles of the medical profession, including the primacy of patient welfare, patient autonomy, and social justice 1. Curriculum should include courses designed to empower medical students, develop strong patient-doctor relationships, and teach them self-nurturing skills to protect against stress and burnout. 2
A recent systematic review of hospitalization care in Peru found it to be average, largely due to low empathy levels among healthcare workers in MINSA (Ministry of Health) and EsSalud (Social Security) hospitals and private clinics 3. Similarly, another review indicated that both professionals and patients perceived empathic care at a moderate level 4. Due to the crucial role of empathy in healthcare, it is imperative for future studies to prioritize developing and testing interventions to enhance empathy among healthcare providers. These initiatives should start in undergraduate studies and extend to continuing medical education.
The Healer’s Art (HA) is an elective course in the School of Medicine at Universidad Peruana Cayetano Heredia (UPCH) that emphasizes values, self-care, and humanity 5. It is based on the idea that a community built on shared values and mutual safety helps students connect with the core principles of scientific medicine and the profession. Developed by Rachel Naomi Remen, MD, at The Remen Institute for the Study of Health & Illness, the course is now widely used 6. However, there is scarce information about its application in developing countries such as Peru.
We conducted a study to assess the narrative responses of medical students from UPCH regarding the usefulness of the HA course and its impact on their future medical practice. All students who participated in the HA course during the 2023 academic year were invited to complete an evaluation, which consisted of 13 questions. The evaluation included a mix of open and closed-ended questions, allowing students to provide both structured responses and more detailed personal insights.
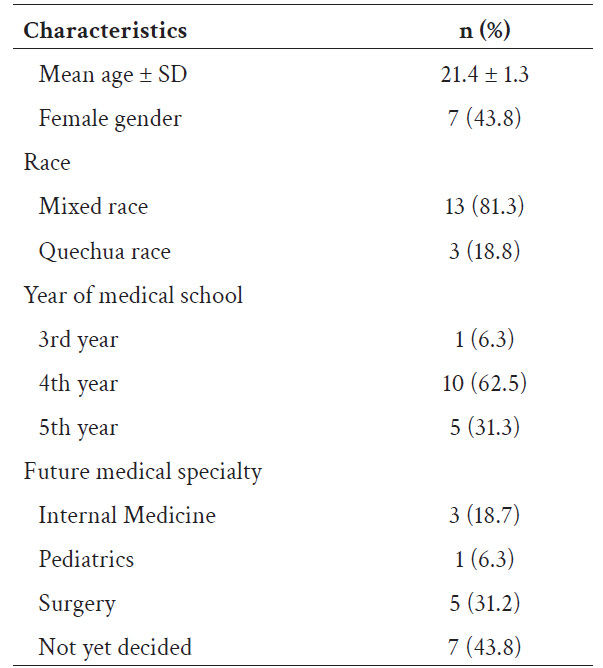
All 16 students enrolled in the course agreed to participate in the study. Participants enrolled for various reasons: the short duration of the course, the holistic approach in patient care, and the opportunity to improve doctor-patient interactions and soft skills. The appealing name of the course, its short duration, and recommendations from friends were key factors in their decision to enroll. Additionally, many participants viewed the course as a therapeutic opportunity, providing a space for personal reflection and emotional support.
94% of participants agreed that the HA course provides educational experiences that are not available anywhere else in the medical curriculum. Additionally, 69% of participants indicated that the experiences in the HA course were different from others in medical school, providing a personal and introspective environment and allowing participants to share emotions, build trust, and connect with peers and instructors. This contrasted with the more academically focused small groups in medical school.
As a result of this course, nearly all participants agreed that they feel more committed to medicine and patient-centered care, more confident in their ability to be good doctors, and more certain that they belong in the profession. They also have a better understanding of what it means to be a good doctor, a clearer idea of what they could offer to patients, and a stronger sense of connection with their peers.
Moreover, participants from the HA course were committed to improve patient care through empathetic listening and holistic treatment. They intend to integrate daily practices learned in the course, such as relaxation techniques and reflective journaling, to reinforce their learning and enhance interactions with patients and colleagues, fostering a compassionate medical environment.
Participants unanimously recommended the course for its transformative impact on personal growth, understanding of others, and exploration of overlooked aspects of medicine like grief. It offers valuable reflection and career support, enhancing overall development beyond the standard curriculum.
This is the first report on the benefits of incorporating the HA course into the medical curriculum of a Peruvian School of Medicine. The positive findings suggest that expanding this course in Spanish to more medical faculties could enhance medical education and foster compassionate healthcare providers in Peru.