Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Gastroenterología del Perú
versión impresa ISSN 1022-5129
Rev. gastroenterol. Perú v.32 n.1 Lima ene./mar. 2012
ARTÍCULOS ORIGINALES
A prospective randomized study comparing partially covered metal Stent versus plastic multistent in the endoscopic management of patients with postoperative benign bile duct strictures: a follow-up above 5 years
Un estudio prospectivo y randomizado comparando el uso de Stents de metal parcialmente cubiertos de plastico versus multistents en el manejo endoscópico de los pacientes con estenosis benignas postoperatorias del ducto biliar en un seguimiento de más de 5 años
Everson L.A. Artifon ; Flavio Coelho ; Mariana Frazao ; Sergio Marques ; Jose B. Paione ; Jonas Takada ; Paulo Boaventura ; Carolina Rebello ; José Pinhata Otoch
Departamento de Cirugia del Hospital Ana Costa, Santos, Brasil.
RESUMEN
FUNDAMENTO: Los Stent de metal autoexpandibles se utilizan a menudo para el drenaje biliar en obstrucción de origen neoplásico, con mejores resultados que los stents plásticos, pero son rara vez utilizados en el drenaje biliar en estenosis de etiología benigna.
OBJETIVO: El objetivo final primario: Es verificar la permeabilidad de la vía biliar después de la colocación de los stents auto-expandible de metal y (múltiples) prótesis plásticas en pacientes con estenosis benignas derivadas de la cirugía del conducto biliar con un seguimiento superior a cinco años. Punto final secundario: Evaluar a largo plazo la tasa de complicaciones en pacientes con stents metálicos autoexpandibles y plástico.
RESULTADOS: Los stents autoexpandibles de metal se colocaron en 15 pacientes y múltiples stents de plástico en 16. La edad media fue de 45 años, con prevalencia de pacientes de sexo femenino en ambos grupos y no hubo diferencia estadística entre los grupos se observó (Stent metálico: 66,7%; plástico multistent: 62,5%, p = 0,8). La tasa de complicaciones resultantes de los stents fueron más frecuentes en el grupo de stent de metal (40% versus 25%, p = 0,37). En el grupo de stent de metal, las complicaciones más frecuentes fueron hemorragia (n = 3; 20%), la migración del stent (n = 2; 13,3%) y perforación (n = 1; 6,7%). En el grupo multistent plástica, las complicaciones más frecuentes fueron la (n: 2, un 12,5%), hemorragia (n = 1; 6,2%) y la úlcera (n = 1; 6,2%). A largo plazo la tasa de permeabilidad tras el drenaje biliar fue mayor en el grupo de metal autoexpandible, SEMS: 81,67% ± 2,56, IC: 76,47-86,54; plástico multistent: 71,88% ± 2,93, IC: 66.08-77.27.
CONCLUSIÓN: El paso temporal de los stents metálicos cubiertos parcialmente auto-expandible es una opción viable para los pacientes con estenosis benignas del conducto biliar.
PALABRAS CLAVE: Prótesis, Stents, Estenosis vías biliares.
ABSTRACT
BACKGROUND: Self-expandable metal stents (SEMS) are often used for biliary drainage due to obstruction of neoplastic etiology, with better results than plastic stents, but seldom for biliary drainage of benign etiology.
OBJECTIVE: Primary end point: Verify bile duct patency after placement of self-expandable metal and (multiple) plastic stents in patients with benign strictures resulting from bile duct surgery with follow-up above five years. Secondary end point: Evaluate long-term complication rate in patients with metal selfexpandable and plastic stents.
RESULTS: Self-expandable stents were placed in 15 patients and multiple plastic stents in 16. Mean age was 45 years with prevalence of female patients in both groups and no statistical difference between groups was observed (SEMS: 66.7%; plastic multistent: 62.5%; p=0.8).
Complication rate resulting from stents occurred more often in the metal stent group (40% versus 25%; p=0.37). In the metal stent group, most frequent complications were hemorrhage (n=3; 20%), stent migration (n=2; 13.3%) and perforation (n=1; 6.7%). In plastic multistent group, most frequent complications were perforation (n:2; 12.5%), hemorrhage (n=1; 6.2%) and ulcer (n=1; 6.2%). Long-term patency rate after biliary drainage was higher in the selfexpandable metal stent group, SEMS: 81.67% ± 2.56; CI: 76.47-86.54; plastic multistent: 71.88% ± 2.93; CI: 66.08-77.27.
CONCLUSION: The temporary passage of partially covered self-expandable metal stents is a feasible option for patients with benign bile duct strictures.
KEY WORDS: Prothesis, Stents, Biliary duct stenosis.
INTRODUCTION
Benign biliary strictures are often derived from iatrogenic causes due to surgical procedures. After cholecystectomies, strictures occur in approximately 0.1-0.5% of open procedures and 0.25-1.0% of laparoscopic surgeries1. They may occur due to direct trauma or possible ischemic microvascular causes after surgical dissection, adjacent inflammation and use of monopolar electrocoagulation for hemostasis2.
Main symptoms of biliary strictures are jaundice, pruritus, and epigastric pain. The most common site for lesions is below the hilum. Surgical treatment is successful in 73% to 90% of cases and morbidity rate ranges from 7% to 26%, whereas mortality occurs from 0 to 13%1. Recurrence is observed in approximately 10% to 35% of cases and is associated with factors such as prior surgery, cirrhosis, portal hypertension, biliary fistula, and advanced age2.
Endoscopic treatment includes radial dilation with balloon dilators followed by the placement of post-stricture stents that must be maintained for at least three months. The control for evaluation of biliary duct patency may be performed through magnetic resonance cholangiography or endoscopic cholangiography. This treatment is less invasive than surgery with success rates ranging from 70% to 80%3. In general, 80-90% of biliary strictures can be treated through endoscopy3. The predictors for endoscopic treatment failure include lesions above the hilum, long stenoses, late postoperative presentation (more than 3 months), anatomic variations of the upper gastrointestinal tract or of the biliary ducts, and clinical conditions of patients that affect the safety of prolonged sedation or general anesthesia3.
METHOD
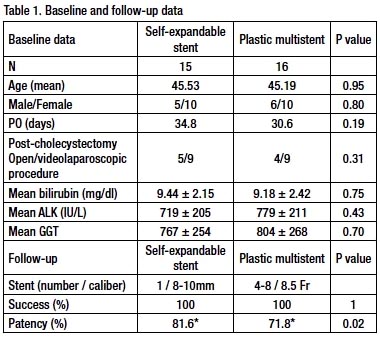
Patients with benign biliary obstruction resulting from benign lesions underwent endoscopic retrograde cholangiopancreatography (ERCP) from 2002 to 2006 in Hospital Ana Costa, Santos, Brazil, and that received indication for endoscopic treatment. After dilation with a 4-mm to 8-mm balloon, patients were randomized into two groups: biliary partially covered self-expandable metal stent (SEMS) or multiple plastic stent (plastic multistent, over three stents, 8.5 Fr in diameter). Table 1.
Inclusion Criteria
Patients aged 18 and older diagnosed with bile duct stricture of benign etiology that received indication for endoscopic treatment with balloon dilation and subsequent placement of biliary stents were included in the study. Prior diagnosis of biliary strictures was based on magnetic resonance imaging (16/31; 51.6%), intraoperative cholangiography (12/31; 38.7%), and ERCP (3/31; 9.7%).
Technique
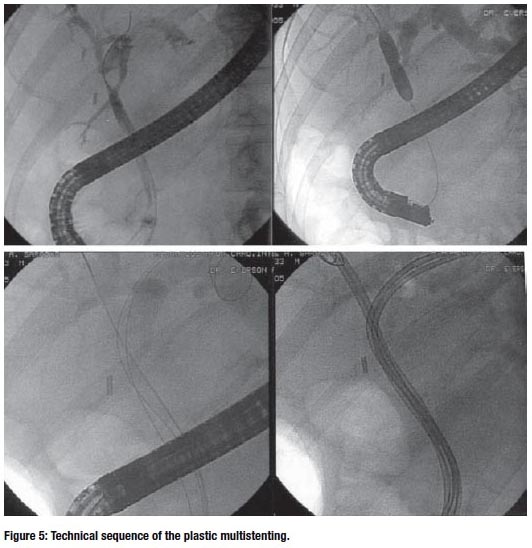
ERCP was performed by a single endoscopist (E.L.A.A.) using a therapeutic duodenoscope (TJF; Olympus Optical Co., Tokyo, Japan). Whenever a biliary stricture was confi rmed, a guidewire was passed through the stenosis followed by the dilation of a 4-mm to 6-mm balloon (Boston Medical Scientific, Natick, USA). Biliary partially covered metal selfexpandable stents (Boston Medical Scientific, Natick, USA, Bloomington, USA) were used. Multiple 8.5-Fr and/or 10-Fr plastic stents 7 cm and/or 9 cm long (Boston Medical Scientific, Natick, USA, Bloomington, USA) were used.
Follow-up and end points
Patients were clinically followed up through periodical visits and laboratory tests with hepatic enzyme dosage prior to the procedure and also afterwards at seven days, 30 days and every six months.
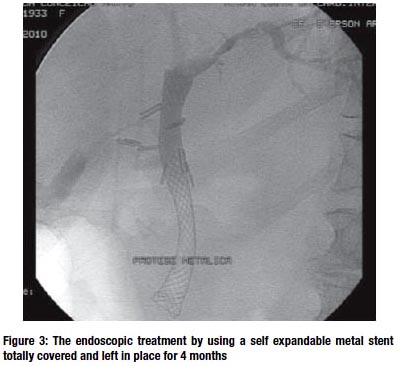
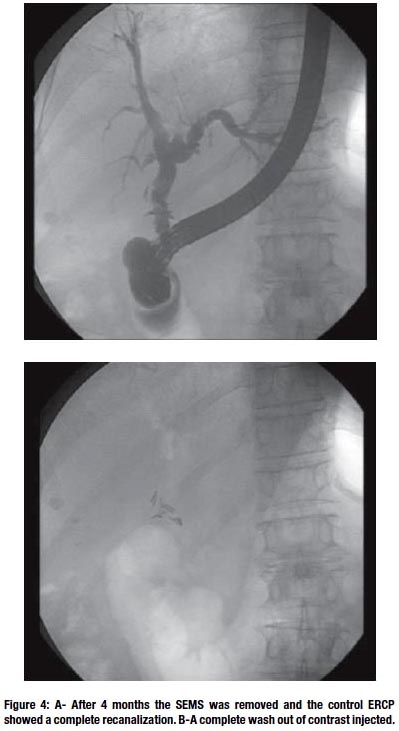
The removal of metal stents was performed after four to five post-procedure months with no passage of new stents subsequently. Plastic stents, nevertheless, were removed after three post-procedure months, when a new session with a 6-mm- to 8-mm-balloon dilation was performed. At the end of this procedure, new multiple plastic stents were placed. The replacement of stents was performed with the same frequency: every three months over a period from six months to one year.
Bile duct patency was evaluated through magnetic resonance imaging. The percentage value of bile duct patency was obtained from dividing the diameter measurement of the stenotic area by the diameter measurement of the bile duct outside the immediately proximal stenotic area. Treatment success was based on good stent placement, jaundice resolution and significant drop of serum bilirubin level, which is determined by a 60%- to 70%-reduction from initial values within six weeks.
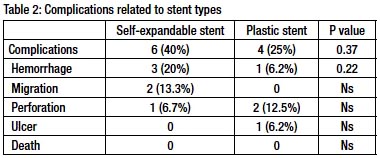
Complications resulting from the endoscopic procedure were evaluated at immediate, intermediate and late time points. Table 2.
Patients were followed up from stent placement up to five and six years.
Statistical Analysis
Qualitative variables were compared using chi-square test or Fishers exact test. Quantitative variables were evaluated through Students t test. Values at p<0.05 were considered significant.
RESULTS
A total of 31 patients was evaluated in this study, of which 15 received partially covered self-expandable metal stents and 16, multiple plastic stents. Success was obtained in stent passage at all cases and technical success was considered at 100%. Mean age was 45 years with prevalence of female patients in both groups and no statistical difference between groups was observed (SEMS: 66.7%; plastic multistent: 62.5%; p=0.8). All cases had benign etiology through postsurgical strictures most frequently due to cholecystectomies (SEMS: 93.3%; plastic multistent: 81.2%; p=0.31) performed as open procedure or laparoscopically (SEMS: n=5 and n=9, respectively; plastic multistent: n=4 and n=9, respectively). Other etiologies were partial hepatectomy (n=1), bariatric gastroplasty (n=1), total gastrectomy (n=1) and fundoplication (n=1). No statistical difference between the interval of stricture approach and the surgery that caused the stricture was observed between the groups (SEMS: 34.8 days; plastic multistent: 30.6 days; p=0.19).
In the plastic stent group, on average 4.8 8.5-Fr-stents were placed (range 4-7 stents per patient).
The complications resulting from stents in both groups occurred more often in the metal stent group (40% versus 25%; p:0.37) (Table 2). In the metal stent group, most frequent complications were hemorrhage (n=3; 20%), stent migration (n=2; 13.3%) and perforation ( n=1; 6.7%). In plastic multistent group, most frequent complications were perforation ( n:2; 12.5%), hemorrhage (n=1; 6.2%) and ulcer (n=1; 6.2%).
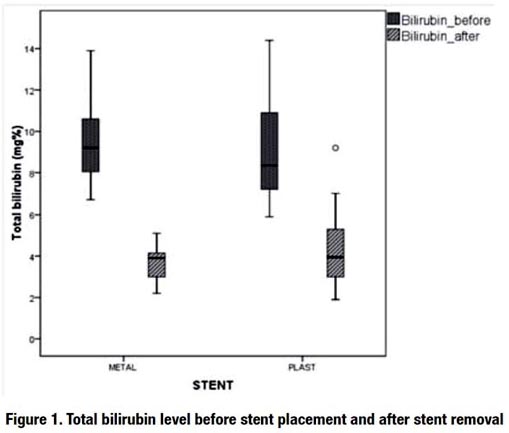
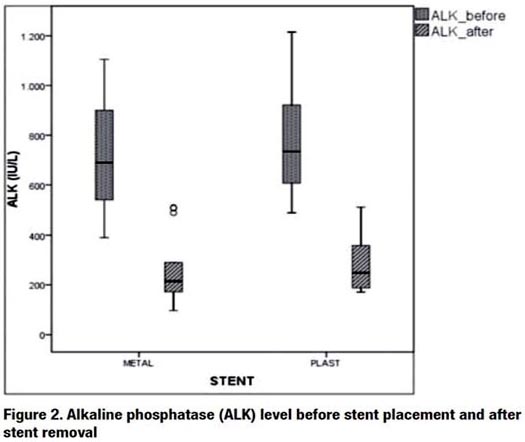
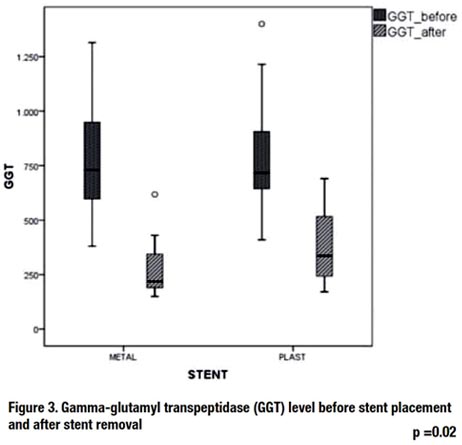
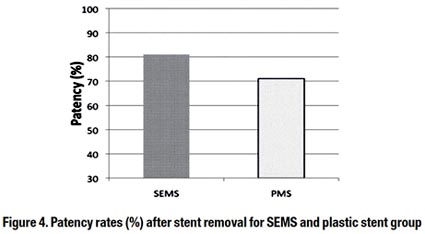
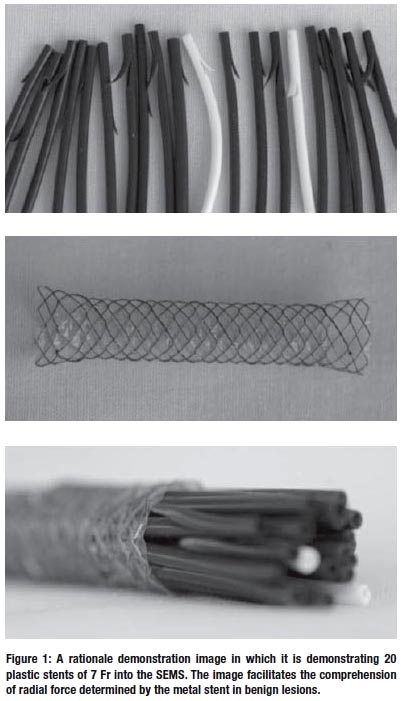
A significant reduction after biliary drainage was verified in the levels of bilirubin, alkaline phosphatase (ALK), and gamma-glutamyl transpeptidase (GGT) in the groups with both types of stents, but no significant difference was verifi ed between them after stent passage (Figure 1, 2 and 3)
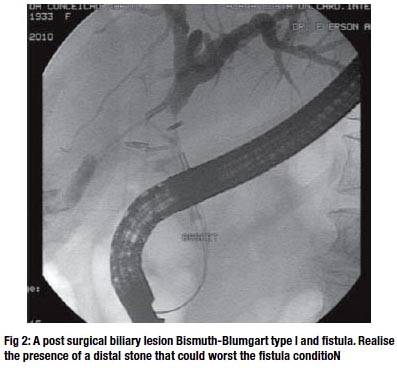
Long-term patency rate after biliary drainage was statistically higher in the metal stent group (SEMS: 81.67% ± 2.56; CI: 76.47-86.54; plastic multistent: 71.88% ± 2.93; CI: 66.08-77.27) (Figure 4).
DISCUSSION
The endoscopic treatment of postoperative biliary strictures experienced great development after the introduction of multistent technique and use of self-expandable stents and made it a feasible, efficacious, less invasive therapy option than surgical treatment. The basic principle of endoscopic therapy consists in the dilation of the stenotic area followed by the placement of a plastic stent to maintain patent the stenotic area with the successive replacement of stents every three months in order to prevent clogging.
Further studies demonstrated that multiple plastic stents passed side by side and maintained on the long term (more than one year) yields better results compared to single shortterm plastic stents. For this reason, the placement of the greatest possible number of stents periodically replaced (approximately 3-4 months) became a practice along a prolonged period of time (above one year)4.
Biliary self-expandable stents to treat benign lesions began to be used more recently with a small number of cases. A study conducted by Kahaleh and collaborators comprising 79 patients with benign strictures demonstrated that selfexpandable metal stents are a feasible treatment option with resolution of 90% of cases after a 12-month follow-up from stent removal5. In this study, the most frequent complication was stent migration observed in 14% of cases with hemorrhage in only 1%. Furthermore, the most frequent etiology was chronic pancreatitis (40%), biliary lithiasis complication (30%), and liver transplant (20%).
Insertion of uncovered self-expandable metal stents to treat benign biliary strictures was evaluated through systematic review and technical success was obtained in 98.9% of cases with clinical improvement in 79.5%, but with a great number of complications (39.5%). Most frequent complications were cholangitis, pancreatitis, stent migration, and hemorrhage. Death occurred in 1.1% of the cases. Self-expandable metal stents are technically easy to insert, with greater inner diameter, but hold the disadvantage of hyperplastic tissue ingrowth through stent mesh causing biliary obstruction and leading to technical difficulty or even the impossibility of their endoscopic removal.
A systematic review comparing single and multiple plastic or metal stents demonstrated technical success in 94.8%, 94% and 98.8% of the cases, respectively, whereas clinical improvement was 59.6%, 94.3% and 79.5%, respectively. Complication rate was 36% for single plastic stent, 20.3% for multiple plastic stent, and 39.5% for metal stent6. Mortality rate at 0.9% was observed in the single plastic stent group mainly due to cholangitis.
In this study comparing two types of stents in benign bile duct diseases, a significant statistical difference was observed in bile duct patency with superior rate for self-expandable stents (81% versus 71%; p=0.02). Conversely, a higher complication rate in this group of patients that received self-expandable stents was observed (40% versus 25%), but not statistically significant (p=0.37). The most frequent complication in the self-expandable stent group was hemorrhage (20% versus 6.2%) and migration (13.3%). In those patients with plastic stents, the most frequent complication was perforation (12.5% versus 6.7%). No death related to the procedure was observed in any of the groups.
CONCLUSION
Covered or partially covered self-expandable metal stents may be a feasible option because they offer good inner diameter similar to that obtained by multiple plastic stents with the benefit of enabling their removal without the problem of hyperplastic tissue ingrowth through stent mesh. Nonetheless, their clinical experience is still limited and presents high complication rates (39.6%).
REFERENCES
1. ARTIFON EL, COUTO JÚNIOR DS, SAKAI P. Tratamento endoscópico das lesões biliares. Rev Col Bras Cir. 2010;37(2):143-152.
2. HALL JG, PAPPAS TN. Current management of biliary strictures. Gastrointest Surg. 2004; 8:1098-1110.
3. VITALE GC, TRAN TC, DAVIS BR, VITALE M, VITALE D, Larson G. Endoscopic management of postcholecystectomy bile duct strictures. J Am Coll Surg. 2008; 206:918-925.
4. COSTAMAGNA G, PANDOLFI M, MUTIGNANI M, SPADA C, PERRI V. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc. 2001; 54: 162-168.
5. KAHALEH M, BEHM B, CLARKE BW, BROCK A, SHAMI VM, DE LA RUE SA, SUNDARAM V, TOKAR J, ADAMS RB, YEATON P. Temporary placement of covered self-expandable metal stents in benign biliary strictures: a new paradigm? Gastrointest Endosc. 2008;67(3):446-54.
6. VAN BOECKEL PG, VLEGGAAR FP, SIERSEMA PD. Plastic or metal stents for benign extrahepatic biliary strictures: a systematic review. BMC Gastroenterol. 2009; 9:96.
7. KUZELA L, OLTMAN M, SUTKA J, HRCKA R, NOVOTNA T, VAVRECKA A. Prospective follow-up of patients with bile duct strictures secondary to laparoscopic cholecystectomy, treated endoscopically with multiple stents. Hepatogastroenterology. 2005 SepOct;52(65):1357-61.
8. DEVIERE J, CREMER M, BAIZE M, LOVE J, SUGAI B, VANDERMEEREN A. Management of common bile duct stricture caused by chronic pancreatitis with metal mesh self expandable stents. Gut. 1994 Jan;35(1):122-6.
9. MACCIONI F, ROSSI M, SALVATORI FM, RICCI P, BEZZI M, ROSSI P. Metallic stents in benign biliary strictures: three-year follow-up. Cardiovasc Intervent Radiol. 1992 Nov-Dec;15(6):360-6.
10. HOLT AP, THORBURN D, MIRZA D, GUNSON B, WONG T, HAYDON G. A prospective study of standardized nonsurgical therapy in the management of biliary anastomotic strictures complicating liver transplantation. Transplantation. 2007 Oct 15;84(7):857-63.













