INTRODUCTION
Melanoma is a deadly skin cancer originating from malignant melanocytes, predominantly present as primary cutaneous melanomas, constituting the most common subtype 1. The majority of cutaneous melanomas (CM) are sporadic and, to a lesser extent have dominant autosomal hereditary patterns 2. Exposure to chronic ultraviolet light (UV) is the principal risk factor to CM 3.
According to the 2020 GLOBOCAN report, CM ranks as the 13th most common type in Peru, with an incidence of 1.8 per 100 000, and a mortality rate of 1% per 100 000 4. Notably, there is a lack of published epidemiological data on CM prevalence in Iquitos, a tropical city in northeastern Peru with warm and rainy weather, where the average temperature is 26 °C. At in 2016, one case of CM was reported at Hospital Regional de Loreto 5. Historically, numerous cases of CM were attended at the Instituto Nacional de Enfermedades Neoplásicas (INEN) located in Lima (Peru) 6. In Peruvian population, acral melanoma is the most prevalent subtype, a form typically associated with a poor prognosis 7. A 2024 study from INEN identified nodular subtype representing the 12.8% of cases. Besides, the lower extremities were the most common primary site for melanoma 8.
This case report enhances the existing knowledge by presenting a rare case of multiple nodular melanomas in a male patient from this amazon and tropical region of Peru. Institutional Research Ethics Committee of Hospital Regional de Loreto (N° 048/24) approved this study. The authors obtained informed consent from the patient.
CASE REPORT
An 82-year-old male patient, originally from a rural community in Maynas, Iquitos (Peru) was admitted to the Hospital Regional de Loreto and hospitalized by the Infectious Diseases Department. He presented with a three-month history of painful skin lesions on his right lower limb. The patient’s medical history was not contributory. The patient reported that initial skin lesions originated as a small nodule on his leg, and over subsequent weeks, three additional similar lesions emerged, all of which progressively increased in size. During this period, the patient noted swelling in his right leg and foot; however, he did not seek medical advice.
On admission, the patient exhibited normal vital signs, and his overall nutritional and hydration status appeared satisfactory. Dermatological examination revealed four skin tumors displaying an exophytic growth pattern, measuring approximately 4x5x4 cm each. These lesions were situated on the external anterolateral aspect of the right shin, and characterized by a verrucose-like appearance, sessile morphology, brown-to-black discoloration, and some with pink spots (Figure 1). Besides, two notable subcutaneous nodules, measuring 1.5 cm and 1.4 cm respectively, exhibited an infiltrative appearance (Figure 2). On sole examination of the affected lower limb, the patient exhibited a brown-to-black macule near his heel suggesting acral melanoma, unfortunately it was not biopsied (Figure 3). There was enlarged lymphadenopathy in the right inguinal area which was not painful. No other clinically relevant physical findings were observed.
The hematologic and biochemical laboratory investigations were within normal limits except for mild anemia, hypereosinophilia, and hypoalbuminemia. All serology tests were negative. Due to the tropical epidemiological context of our institution, subcutaneous fungus infection and cutaneous tuberculosis were suspected. However, melanoma prevailed as a relevant differential diagnosis, therefore a skin biopsy was requested.
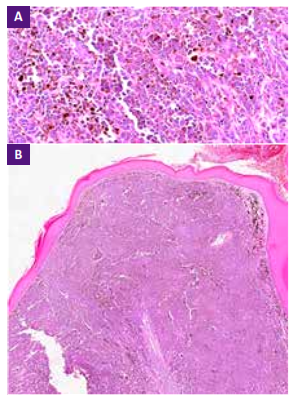
On histopathological examination of the skin biopsy, it showed epithelial melanocytes proliferation with a nodular pattern, the presence of melanin pigment nests, associated with a superficial ulcerated bed (Grade IV), and an infiltrated profound border. No specific melanoma or other oncological biomarkers were assessed due to limited laboratory resources. The biopsy confirmed the diagnosis of ulcerated nodular melanoma, Breslow index of 5mm (Figure 4A and 4B). The patient was transferred to the Oncology Department for further medical evaluation.
DISCUSSION
Cutaneous melanoma is a malignant tumor arising from the uncontrolled activity of melanocytes. Extracutaneous manifestations are less frequent. Traditionally, CM is subdivided into 4 categories: lentiginous, acral, superficial spreading, and nodular 1. A Peruvian cohort study found that 72.1% of melanomas occurred on the lower extremities, with many lesions being pigmented and ulcerated 8, similar to our patient. In our setting, CM may be underdiagnosed due to factors like limited healthcare access. For our patient, the vertical growth pattern of nodular melanoma was key to the clinical presentation
Our patient skin lesions resembled a patient in the clinical presentation of vascular-like lesions, displayed in a multiple nodular pattern, and an onset presentation. Furthermore, the cutaneous compromise showed a unilateral distribution as seen in our patient 9. Notably, nodular CM may present as a giant mass in the back with lung and brain metastases as seen in an elderly patient 10. Another more aggressive presentation of multiple nodular melanoma may encompass dermal and subcutaneous tissue along the entire right side of the body 11.
However, the clinical presentation can vary based on factors such as geographic origin, as seen in the Indian Subcontinent, where a patient presented with multiple nodules with a bosselated surface on the lower limb 12. Remarkably, nodular melanoma has been documented as a congenital mass in a newborn 13. To our knowledge, this clinical presentation of nodular melanoma has not been previously reported in the Peruvian tropics. Reports from Lima provide valuable insights into melanoma cases. One study described an exophytic lesion on the right sole, revealing a giant acral melanoma, along with multiple nodular lesions on the right lower limb, closely resembling our patient’s presentation 14. Additionally, another study reported an acral nodular type affecting the first toe 15.
In tropical regions, diagnosing skin lesions like those in our patient can be challenging, as infections may mimic neoplasia or vice versa. For instance, a case of multiple nodular-ulcerative lesions initially misdiagnosed as sporotrichosis, leading to ineffective antifungal treatment, was later revealed to be melanoma 16. Subcutaneous fungus infections, including distinct forms of localized lobomycosis 17, confluent nodular lesions of chromoblastomycosis 18, and verrucose plaque or nodules of phaeohyphomycosis 19 should be considered for differential diagnosis. We must also consider protozoan parasite infections, especially the verrucous presentation of leishmaniasis 20, due to their high prevalence in our region.
Various infectious diseases present with verrucose or nodular lesions and distinguishing them from the neoplastic condition is crucial for appropriate treatment. The physicians should be able to differentiate the basic morphology of lesions and use proper diagnostic tests such as histopathology examination, imaging studies, and tumor markers.
In Iquitos, Loreto, heightened awareness of melanoma risk factors is crucial due to the region’s proximity to the equator and high UV exposure. Residents should prioritize sun protection by consistently applying sunscreen, wearing protective clothing, and undergoing regular dermatological checkups. Tailoring educational efforts to the local context emphasizes the importance of effective preventive measures, promoting a community-wide commitment to skin health
In conclusion, the CM poses challenges in the tropics due to diagnostic complexities. In our patient, nodular melanoma exhibited a unique presentation crucial for diagnosis. Comparisons with other cases reveal varied clinical presentations worldwide. In tropical regions, distinguishing between neoplasia and infections poses a challenge, requiring proper diagnostic. In Iquitos, awareness of melanoma risk factors highlights the need for prevention strategies. Residents should prioritize sun protection and regular dermatological checkups due to the high UV exposure. We recommend continued, high-quality data collection on cancer diagnoses, especially melanoma, to inform public health decisions effectively.