INTRODUCTION
The SARS-Cov-2 health emergency and the high death rate have caused enormous inequalities in health, leading to the oversaturation of hospital services during epidemic waves 1. Peru has produced more than 3 million cases with more than 212,000 deaths with a fatality rate of 5.98% 2; SARS-CoV-2 infection has affected more in Amazonian areas than coastal areas of Peru, with seroprevalences of 70% 3 and 29% 4, respectively.
The clinical characteristics of COVID-19 are very diverse but can be arranged into four categories: systemic, respiratory, gastrointestinal, and cardiovascular 5. There are a wide number of symptoms in patients with COVID-19, only six symptoms occurred in 50% of people such as cough, sore throat, fever, myalgia or arthralgia, fatigue, and headache 6,7. Of these, fever, myalgia or arthralgia, fatigue, and headache could be considered red flags 5. Loss of smell taste is a highly specific symptom of COVID-19 8. Knowing the specific symptoms of COVID-19 does not help to have a quick diagnosis, better follow-up, and prognosis of infected patients.
The main cause of death is respiratory failure due to acute respiratory distress syndrome 9. The overall combined mortality rate from respiratory failure in COVID-19 patients is discharged; however, this varies significantly between countries 10. People younger than 65 have a very small risk of death even in the epicenters of a pandemic, and deaths in people younger than 65 without any underlying conditions are rare. 11. The prognosis of patients with COVID-19 can be affected by comorbidities such as diabetes, 12 hypertension, stroke, cancer, kidney disease, and high cholesterol 13. Risk factors should be considered to avoid rapid progression and poor prognosis of COVID-19 disease. More attention should be paid to these patients, in case of rapid deterioration.
Laboratory medicine is of great help for the early detection of SARS-CoV-2 and allows us to discriminate between patients with severe and non-severe COVID-19 14. Findings in COVID-19 patients will help better understand key disease traits and could be used for future disease research, control, and prevention 15. COVID-19 has a significant impact on the hematopoietic system and hemostasis 16. Leukocytosis, lymphopenia, and thrombocytopenia are associated with increased severity and even death in COVID-19 cases 17. Lymphopenia can be considered a key laboratory finding, with prognostic potential 16. A significant decrease in peripheral CD4 + and CD8 + T lymphocytes was observed 18. These findings are important to knowing the prognosis of patients with COVID-19.
There are still questions to be resolved about COVID-19, it is with us a short time, which is a short time to give accurate details about it, that is why it is necessary to increase research in all fields of science, to help us fight the pandemic and get back to the new normal. This study examined the laboratory results of COVID-19 patients from a hospital in the Peruvian Amazon and their clinical prognosis.
MATERIALS AND METHODS
Study design
A retrospective longitudinal study was carried out, the purpose of which was to identify the laboratory tests of patients with COVID-19 and mortality in a hospital in Ucayali (located in the Central Jungle, in eastern Peru). Ucayali has a population of approximately 500,000 inhabitants.
Population and sample
The population consisted of hospitalized patients with a confirmed diagnosis of COVID-19 in a hospital in Ucayali, Peru during the period from March 13 to May 9, 2020, selected a total of 127 people consecutively. Only patients with a history of hematological disorders were excluded (leukemias, thrombocytopenias, anemias, etc.).
Procedures
The diagnosis of COVID-19 was made based on the provisional guidelines of the World Health Organization (WHO) 19. A confirmed case of Covid-19 was defined as a positive result in the polymerase chain reaction-transcriptase (RT-PCR) assay of nasopharyngeal swab samples and rapid immunochromatographic test. The only laboratory-confirmed cases were included in the analysis. Follow-up was carried out until discharge or death.
The laboratory tests were performed within the hospital headquarters at the time of admission, these were corroborated by a pathologist. All the laboratory tests were carried out following the clinical care needs of the patient following the technical standard of the Ministry of Health of Peru. Laboratory evaluations consisted of leukocytes, neutrophils, platelets, red cell distribution width-standard deviation (RDW-SD), Relation neutrophils/lymphocyte (RN/L), fibrinogen, c-reactive protein (CRP), D-dimer, lactate dehydrogenase (LDH), hematocrit, monocytes, eosinophils.
Statistical analysis
Statistical analysis was performed in the STATA v.16.1 software (StataCorp LP, College Station, TX, USA). Mean and the standard deviation was described for age, leukocytes, neutrophils, platelets, RDW-SD; median and interquartile range for the variables lymphocyte, RN / L, fibrinogen, CRP, D-dimer, DHL, hematocrit, monocytes, eosinophils; the variables sex, ICU, and death were reported as frequencies and percentages.
In the bivariate analysis of categorical variables, the chi-square test was used to explore the association between laboratory factors and COVID-19 mortality, after evaluating the assumption of expected frequencies. For the numerical variables, the student's t-test was used for independent samples, or the Mann Whitney U test according to the normality distribution. In the simple regression analysis, prevalence ratios (PR) and 95% confidence intervals(IC 95%) were estimated, using the Poisson distribution family, log link function, and robust variance. For the multiple models, a parsimonious model was built by performing a nesting process between the variables that were found to contribute significantly to the model, using the Likelihood-ratio test.
The area under the curve (AUC) values with their 95% confidence intervals of the hematological variables were calculated for the prediction of mortality.
Ethical aspects
The present research was approved by the ethics committee of the “Universidad Nacional de Ucayali” (IE005-FMH-UNU) and the informed consent obtained from the participants who participated was requested.
Codes were used to maintain the confidentiality of data for COVID-19 patients eligible for this study. The ethical principles of the Declaration of Helsinki were respected.
RESULTS
Information was collected from 127 people from Hospital II Essalud Pucallpa. It is a population with an average age of 59.6 years, where the female sex predominated (67.72%). Of this population, it was found that 21 (83.46 %) patients were in the ICU, also the entire population had a mortality of 75 people (59.06 %).
Regarding the laboratory tests, it is observed that, on average, the general population had high levels of biochemical and hematological values. However, when stratifying according to mortality, the parameters such as leukocytes and neutrophils were statistically much higher in patients who died (p <0.001 in both cases), also, those who died had lymphocytopenia compared to normal values in survivors (720 vs 1360 respectively, p <0.001), something similar happened with monocytes and eosinophils.
It can be seen that in other parameters such as RN / L, and fibrinogen among others, they were higher in the population that died compared to the one that survived. Platelet, RDW-SD, and D-dimer values were statistically similar in both groups. Table 1.
Table 1 Clinical, laboratory, and hematological characteristics of the population hospitalized with COVID-19, Ucayali.
| Total | Died | Survived | |||||
| Numeric variables * | Mean | SD | Mean | SD | Mean | DS | p-value |
| Age | 59.6 | 14.21 | 66.1 | 10.8 | 50.2 | 13.3 | <0.001 |
| Leukocytes | 13 778.12 | 6 973.44 | 15 503.9 | 7 438 | 11 289.1 | 5 400 | <0.001 |
| Neutrophils | 12 037.04 | 7 183.8 | 14 034.5 | 7 413 | 9 099.6 | 5 735 | <0.001 |
| Platelets | 286 119 | 130 685 | 290 202 | 14 156 | 280 307 | 19 890 | 0.677 |
| RDW-SD | 45.42 | 3.9 | 45.3 | 3.6 | 45.6 | 4.5 | 0.642 |
| Numeric variables ± | Median | IQR | Median | IQR | Median | IQR | p-value |
| Lymphocyte | 900 | 690 | 720 | 520 | 1360 | 1770 | <0.001 |
| Fibrinogen | 672 | 490 | 774.3 | 264 | 373.5 | 182 | <0.001 |
| PCR | 2.45 | 13.5 | 1.8 | 2.8 | 3.85 | 15.4 | 0.012 |
| D-dimer | 1.48 | 2.7 | 4.7 | 6.2 | 1.35 | 1.6 | 0.091 |
| DHL | 715 | 390 | 817 | 261 | 495.5 | 298 | <0.001 |
| Hematocrit | 39.5 | 8.2 | 42.2 | 6.4 | 37.65 | 7.4 | <0.001 |
| Monocytes | 390 | 300 | 300 | 300 | 480 | 390 | <0.001 |
| Eosinophils | 20 | 80 | 10 | 45 | 125 | 290 | <0.001 |
| Categorical variables¥ | N | % | N | % | N | % | p-value |
| Sex | |||||||
| Female | 86 | 32.28 | 20 | 48.78 | 31 | 36.05 | 0.104 |
| Male | 41 | 67.72 | 55 | 63.95 | 31 | 36.05 | |
| RN/L Categorized | |||||||
| RN/L>= 30 | 101 | 80.16 | 71 | 70.3 | 30 | 29.7 | <0.001 |
| RNL/L <30 | 25 | 19.84 | 4 | 16 | 21 | 84 | |
| Condition | |||||||
| UCI | 21 | 83.46 | 5 | 23.8 | 16 | 76.2 | <0.001 |
| No-UCI | 106 | 16.54 | 70 | 66.1 | 36 | 33.9 |
SD: Standard deviation. IQR: Interquartile range. * Values are presented in mean and SD, p-value calculated with the t-student test. ± Median and IQR values are presented, p-value calculated with the Mann-Whitney test. ¥ Absolute and relative frequencies are presented, p-value calculated with the chi-square test. RNL: Relation neutrophils/lymphocyte. CRP: c-reactive protein. LDH: lactate dehydrogenase. RDW-SD: Red cell distribution width-standard deviation.
No differences were observed in this population regarding death and sex (OR: 1.31; 95% CI 0.92 to 1.87), however, it was observed that, for each one-year increase, the probability of death increased by 4% (PR: 1.04, 95% CI 1.03 to 1.05). The IRR (Incidence Risk Ratio) analysis for the numerical variables showed results strongly associated with hematological values such as Leukocytes (scaled by 2500 units) (IRR: 1.08, 95% CI 1.03 to 1.13), neutrophils (scaled by 2500 units) (IRR: 1.08; 95% CI 1.03 to 1.13), on the contrary, it is observed that the increase of 1000 units in lymphocytes, the probability of dying decreased by 48% (IRR: 0.52; 95% CI 0.38 to 071). It is worth mentioning that the one with the greatest strength of association was the D-dimer since for each 1 mg / L increase in D-dimer, the risk of dying increased by 25% (IRR: 1.25, 95% CI 1.10 to 1.43). The other results are shown in Table 2.
Table 2 Comparison of hematological and clinical values in the hospitalized population with COVID-19, Ucayali.
| Crude Analysis | Parsimonic model | |||||
| RPc | CI 95% | p* | RPa | CI 95% | p± | |
| Sex | ||||||
| Male | Ref | - | ||||
| Female | 1.31 | 0.92 - 1.87 | 0.133 | |||
| IRRc | IC 95% | valor-p | IRRa | IC 95% | valor-p | |
| Age | 1.04 | 1.03 - 1.05 | <0.001 | - | ||
| Neutrophils (Staggered 2500) | 1.09 | 1.05 - 1.14 | <0.001 | 1.08 | 0.99 - 1.17 | 0.089 |
| Lymphocyte (Staggered 1000) | 0.52 | 0.38 - 0.71 | <0.001 | 0.22 | 0.08 - 0.57 | 0.002 |
| D-dimer | 1.25 | 1.10 - 1.43 | 0.001 | 1.14 | 1.01 - 1.29 | 0.039 |
| Hematocrit | 1.04 | 1.01 - 1.07 | 0.008 | - | ||
| RDW-SD | 0.99 | 0.95 - 1.03 | 0.652 | - | ||
| Platelets (Staggered 1000000) | 1.27 | 0.41 - 3.97 | 0.682 | - | ||
| Leukocytes (Step 2500) | 1.08 | 1.04 - 1.13 | <0.001 | - | ||
| RN/L Categorized | ||||||
| RN/L< 30 | Ref | |||||
| RNL/L>=30 | 4.39 | 1.77 - 10.92 | 0.001 | - | ||
| Fibrinogen (Tier 100) | 1.03 | 1.01 - 1.06 | 0.013 | - | ||
| PCR | 0.98 | 0.085 - 1.01 | 0.085 | - | ||
| DHL | 1.00 | 1.00 - 1.00 | 0.340 | - | ||
| Monocytes | 0.99 | 0.99 - 1.00 | 0.226 | - | ||
| Eosinophils | 0.99 | 0.99 - 1.00 | 0.053 | - |
*P-value obtained from the generalized linear model, using the Poisson family and the robust Log and variance link function. ± p-value obtained from the generalized linear model for a parsimonious model with backward elimination, Poisson family, and robust Log link function and variance were used. 95% CI: 95% confidence interval. RP: Prevalence ratio. IRR: Incidence Risk Ratio. c: Crude. a: Adjusted. RNL: Relation neutrophils/lymphocyte. Ref: Reference. RNL: Relation neutrophils/lymphocyte. CRP: c-reactive protein. LDH: lactate dehydrogenase. RDW-SD: Red cell distribution width-standard deviation.
In the explanatory variables model, it was observed that D-dimer and lymphocytes (scaled by 1000 units) had a strong association with mortality (IRR: 1.18 and 0.22 respectively), neutrophils (scaled by 2500 units) had a marginal association (IRR: 1.08, 95% CI: 0.99 to 1.17).Table 2.
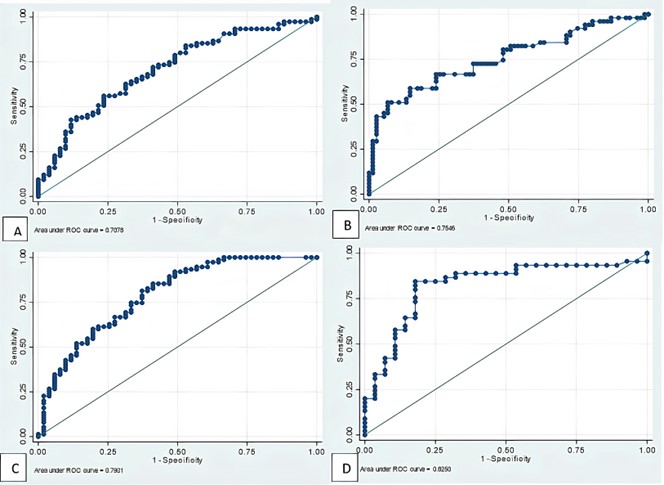
These results were complemented with the search for the area under the curve (AUC), where it was found that fibrinogen had the best AUC (AUC: 82.5%, 95% CI 72.17 to 92.83), followed by RN / L with AUC: 79.01 %. These and other variables can be seen in Table 3 and Figure 1.
Table 3 Areas under the curve (AUC) of hematological variables and mortality prediction in patients with COVID-19 in Ucayali.
| Hematological variables | AUC (%) | CI 95% |
| Leukocytes | 67.35 | 57.94 to 76.76 |
| Neutrophils | 70.78 | 61.61 to 79.97 |
| Platelets | 53.47 | 43.03 to 63.91 |
| RDW-SD | 50.51 | 39.73 to 61.30 |
| Lymphocyte | 75.46 | 66.44 to 84.49 |
| RN / L | 79.01 | 70.87 to 87.15 |
| Fibrinogen | 82.50 | 72.17 to 92.83 |
| CRP | 64.39 | 53.65 to 75.14 |
| D-dimer | 65.14 | 44.44 to 85.83 |
| LDH | 73.42 | 61.33 to 85.51 |
| Hematocrit | 71.36 | 61.99 to 80.72 |
| Monocytes | 66.17 | 56.56 to 75.78 |
| Eosinophils | 76.59 | 64.86 to 88.33 |
RNL: Neutrophil Lymphocyte Ratio. * AUC: Area under the curve. RNL: Relation neutrophils/lymphocyte. CRP: c-reactive protein. LDH: lactate dehydrogenase. RDW-SD: Red cell distribution width-standard deviation.
DISCUSSION
We look at the clinical symptoms of 127 COVID-19 patients, here, we mainly analyze and summarize the laboratory tests of COVID-19 patients, especially the biochemical and hematological parameters. In our study, the laboratory tests of the general population studied that was infected by SARS-CoV-2 had high levels of biochemical and hematological values, these findings have also been found in other systematic reviews of patients with COVID-19 and SARS 17,20,21. These findings can be explained why the blood presents a state of hypercoagulation, which becomes more acute in critically ill patients. 22. Our results show important biochemical and hematological changes in patients with COVID-19.
It was found that the parameters such as leukocytes and neutrophils were statistically much higher in patients who died (p <0.001 in both cases), these risk factors related to immunity can predict the mortality of patients with COVID-19 23. Patients who died presented lymphocytopenia compared to normal values in survivors (720 vs 1360 respectively, p <0.001), something similar happened with monocytes and eosinophils. Lymphocytopenia is an independent risk factor for hospital mortality for COVID-19 patients, especially men 24. Risk factors related to the mortality of patients with COVID-19 were found such as increased leukocytes and neutrophils along with lymphocytopenia, the evaluation of these parameters can help to identify people at high risk with COVID-19.
It can be seen that in other parameters such as the neutrophil-lymphocyte ratio (RN / L), and fibrinogen among others, they were higher in the population that died compared to the one that survived. Elevated fibrinogen level has been considered an epiphenomenon of pulmonary edema rather than activation of coagulation in affected patients 25. Platelet values, red cell distribution width with standard deviation (RDW-SD), and D-dimer were statistically similar in both groups. There are findings in which an increase in D-dimer levels is found and this increases according to the severity in patients with COVID-19 25,26. RDW-SD was a predictor in the group of severe patients in which its values were significantly higher than those of the group of patients with moderate COVID-19 27.
In this study, it was observed that, for each one-year increase, the probability of dying increased by 4%, these results have been reported in other studies 28. It is worth mentioning that the one who presented the greatest strength of association was D-dimer, since for every 1 mg / L increase in D-dimer, the risk of dying increased by 25%, these high values are associated with those with severe disease 29.
Laboratory parameters in patients with COVID-19 such as leukocytes, neutrophils and D-dimer were statistically higher and adequate association in patients who died