Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Medicina Experimental y Salud Publica
Print version ISSN 1726-4634
Rev. perú. med. exp. salud publica vol.38 no.3 Lima July/Sep 2021 Epub Aug 26, 2021
http://dx.doi.org/10.17843/rpmesp.2021.383.7446
Original articles
Prevalence and factors associated with the intention to be vaccinated against COVID-19 in Peru
1 Universidad Privada San Juan Bautista. Lima, Perú.
2 Red Internacional en Salud Colectiva y Salud Intercultural. Ciudad de México, México.
3 Instituto de Evaluación de Tecnologías en Salud e Investigación, EsSalud. Lima, Perú.
4 Médicos Sin Fronteras. Política Sanitaria. Bruselas, Bélgica.
5 Universidad Científica del Sur. Lima, Perú.
6 Centro de Investigación Epidemiológica en Salud Global, Universidad Privada Norbert Wiener. Lima, Perú.
7 Facultad de Medicina Humana, Universidad de San Martín de Porres. Chiclayo, Perú.
8 Unidad de Investigación Multidisciplinaria, Clínica Avendaño. Lima, Perú.
9 Grupo de Investigación Biomedicina, Facultad de Medicina, Fundación Universitaria Autónoma de las Américas. Pereira, Colombia.
10 Asociación Colombiana de Infectología. Bogotá, Colombia.
11 University of Connecticut. Storrs, Connecticut, Estados Unidos.
12 Unidad de Revisiones Sistemáticas y Meta-análisis, Guías de Práctica Clínica y Evaluaciones Tecnológicas Sanitarias. Universidad San Ignacio de Loyola, Lima, Perú.
13 Unidad para la Generación y Síntesis de Evidencias en Salud, Universidad San Ignacio de Loyola. Lima, Perú.
Objectives:
To estimate the prevalence and factors associated with the intention to be vaccinated (ITV) against COVID-19 in Peru.
Materials and methods:
Analytical cross-sectional study using the survey conducted by the University of Maryland, USA, on Facebook. The dependent variable is the ITV. Crude and adjusted prevalence ratios (PR) were calculated, with their 95% confidence intervals (95% CI) using generalized linear models of the Poisson family, in order to evaluate the association of sociodemographic variables, compliance with community mitigation strategies, symptoms of COVID-19, mental health and acceptance of vaccination before the recommendation (AVR) by various actors and health authorities, with the ITV.
Results:
Data from 17,162 adults were analyzed. The overall prevalence of the ITV was 74.9%. A lower prevalence of the ITV was associated with the female sex (PR=0.95; 95% CI: 0.94-0.97), living in a town (PR=0.95; 95% CI: 0.91-0.99) or village or other rural area (PR=0.90; 95% CI: 0.86-0.93) and the AVR of politicians (PR=0.89; 95% CI: 0.87-0.92). Conversely, having COVID-19 symptoms (PR=1.06; 95% CI: 1.03-1.09), economic insecurity (PR=1.04; 95% CI: 1.01-1.06), fears of becoming seriously ill or that a family member becomes seriously ill from COVID-19 (PR=1.49; 95% CI: 1.36-1.64) and the AVR of family and friends (PR=1.10; 95% CI: 1.08-1.12), healthcare workers (PR=1.29; 95% CI: 1.26-1.32), World Health Organization (PR=1.34; 95% CI: 1.29-1.40) and government officials (PR=1.18; 95% CI: 1.15-1.22) was associated with a higher prevalence of the ITV.
Conclusions:
Three-quarters of the respondents had the ITV. There are potentially modifiable factors that could improve vaccine acceptance.
Keywords: COVID-19; SARS-Co-V2; COVID-19 Vaccines; Vaccination; Vaccination Refusal; Peru
INTRODUCTION
On June 7, 2021, the World Health Organization (WHO) reported 173,005,553 confirmed cases of COVID-19, including 3,727,605 deaths 1. With no effective treatment and few therapies to modify the course of the disease, the global hope of controlling the disease rests on the effective and universal distribution of available vaccines 2.
Vaccination is key for succeeding in controlling the disease 3. Despite the growing number of safe and effective vaccines on the market, reluctance to vaccinate is a growing problem with global implications 4. This has become an important phenomenon due to outbreaks of preventable diseases that were previously controlled with vaccines 5. In the context of the COVID-19 pandemic, vaccination acceptance is a relevant discussion due to misinformation, mistrust and conspiracy theories that have hindered the adoption of community mitigation measures against the disease, such as vaccines 6.
There are several studies related to the acceptance of vaccination against COVID-19. Some countries such as China, United States, Ecuador, Malaysia, Indonesia, South Korea, Brazil, South Africa, Denmark and United Kingdom have a high acceptance rate, between 65% and 97% 7 - 10. In contrast, other countries have low acceptance rates, between 55% and 62%, such as Russia and France 11 , 12. Vaccine acceptance varies according to sociodemographic factors such as gender, belonging to ethnic minorities, rural population, economic income or sociological factors such as political tendencies, among others 6 , 10 , 13 - 16. We recently reported that countries from Latin America and the Caribbean intended to vaccinate 80% of their population by February 2020; and that fears of becoming seriously ill, having a family member fall ill from COVID-19 and having depressive symptoms were associated with a higher probability of having the intention to be vaccinated 17. In contrast, being female and non-binary was associated with a lower vaccination intention 17.
Peru has been one of the countries most affected by the COVID-19 pandemic. According to the situation room of the Peruvian Ministry of Health (MINSA), more than 1.9 million cases and more than 186,500 deaths due to COVID-19 were reported by June 7, 2021 ( 18. On February 7, 2021, the first batch of vaccines arrived in Peru, initiating the vaccination process against COVID-19. Although more than four million doses have been administered to date 18, the vaccine is not fully accepted in Peru, as in other parts of the world. According to a survey published by Ipsos in February 2021, if a free vaccine against COVID-19 were available, 35% of the country’s population would not get vaccinated, the first reason being fear of adverse effects 19. A previous study conducted by the authors on the vaccination intention in Latin America and the Caribbean did not include variations at the departmental level, in order to identify aspects that could individualize vaccination strategies in each of the departments of Peru 17. Therefore, the aim of this research was to determine the prevalence and factors associated with the intention to be vaccinated (ITV) against COVID-19 in Peru.
KEY MESSAGES
Motivation for the study: Despite the fact that Peru is one of the countries most affected worldwide by the COVID-19 pandemic, the prevalence of the intention to be vaccinated against this disease is uncertain.
Main findings: Three out of four respondents on Facebook intended to be vaccinated. There are modifiable and non-modifiable factors associated with the intention to be vaccinated against COVID-19 in Peru.
Implications: Communication strategies targeting population groups that influence vaccination intention may favor vaccination against COVID-19 in Peru.
MATERIALS AND METHODS
Study design and database
We conducted a secondary analysis of a database collected by the University of Maryland, USA, and the social network Facebook (Facebook, Inc.) by means of a survey aimed at assessing different characteristics of respondents in the context of the COVID-19 pandemic. The survey includes demographic information, self-report of COVID-19 symptomatology, assessment of food and economic security, mental health, and a module on attitudes toward vaccination. The survey was first conducted on April 23, 2020, and has since been administered daily in more than 200 countries or territories, translated into the primary language of each country 20. The selection of the participants was random, within the sampling frame of the total number of Facebook users according to geographic region and country. Likewise, each selected participant was weighted according to the region and country in which they responded to the survey. In case people declined the invitation or omitted to participate in the survey, Facebook invited another person within the same geographic area who had not responded to the survey within the last eight weeks.
Population and sample
The survey population included Facebook users aged 18 years and older. For this analysis, we included participants from Peru who had responded to the survey between January 15 and February 1 (n = 29,140 adults). We excluded participants who did not have data on the variables of interest for this study. Thus, we analyzed data from 17,162 adults in Peru.
Variables
The outcome of the study was the ITV. ITV was assessed by the following question, "If you were offered a vaccine today to prevent COVID-19, would you choose to be vaccinated?". This question had four possible answers: “Yes, definitely”, “probably yes”, “probably no”, “definitely no”. The variable was dichotomized by considering the last two alternatives as non-ITV against COVID-19 and the first two alternatives as ITV.
Independent variables
Sociodemographic characteristics
Gender (male, female, non-binary), age (18-24, 25-34, 35-44, 45-54, 55-64, 65-74, 75 and older) and the participant’s area of residence (city, town, village or other rural area) were included.
Compliance with community mitigation strategies and COVID-19 symptoms at the time of the survey.
The presence of suspected COVID-19 symptomatology at the time of the survey was defined as three or more of the following symptoms in the last 24 hours 21: fever, cough, respiratory distress, fatigue, coryza, muscle pain, sore throat, chest pain, nausea, loss of smell, eye pain, and headache.
Compliance and adherence to the three main community mitigation strategies to reduce coronavirus transmission were included: hand washing, use of masks, and physical distancing. Compliance with physical distancing was considered when the participant reported not having been in direct physical contact (including touching, shaking hands, hugging, kissing) for no more than one minute in the past 24 hours and not having been within two meters of any person with whom he or she does not currently live. Handwashing compliance was considered when participants reported having washed their hands at least once in the last 24 hours. In addition, compliance with facemask use was considered when participants reported having worn a facemask in public (at least sometime) during the last seven days. A variable was created considering compliance with the three community mitigation strategies previously mentioned.
Mental Health
Fear that the participant or a member of his or her family might become seriously ill with COVID-19 was assessed by the following question, “How worried are you that you or someone in your immediate family might become seriously ill with coronavirus (COVID-19)?”. The question had the following possible responses: “Very worried”, “somewhat worried”, “not very worried”, “not worried at all”. A dichotomous variable was created considering the last alternative as the absence of fear that the participant or a family member would become seriously ill with COVID-19 and the remaining three as the presence of fear.
Food and economic insecurity
Food security was assessed using the following question, “Are you worried about having enough food for the next week?”. This question had four possible answers: “Very worried”, “somewhat worried”, “not very worried”, “not at all worried”. The variable was dichotomized by considering the first three alternatives as food insecurity.
Economic security was assessed by the following question: “Are you worried about your household’s economy for the next month?”. This question had four alternatives: “very worried”, “somewhat worried”, “not very worried”, “not at all worried”. The variable was dichotomized by considering the first three responses as economic insecurity.
Likelihood of vaccination acceptance on the recommendation of different actors
We assessed the influence that friends and family, physicians and other health professionals providing medical care, the World Health Organization (WHO), government health authorities, and politicians might have on the participant’s ITV. This was assessed by the following question, “Would you be more or less likely to be vaccinated against COVID-19 if it was recommended by each of the following...?”. This question had three responses: "More likely", "about the same", "less likely". The last two alternatives were considered as the lack of influence on the acceptance of vaccination, and the first alternative as the presence of influence on the acceptance of vaccination.
Statistical analysis
We downloaded the database in Microsoft Excel® 2010 format and imported it into the statistical package STATA® v14.0 (StataCorp, TX, USA). We carried out the statistical analyses considering the complex sampling of the survey, using the svy command.
We described the qualitative variables using absolute frequencies and weighted proportions according to the complex sampling of the survey with their respective 95% confidence intervals (95% CI). We also carried out bivariate analysis between covariates of interest and outcome variables using Pearson’s Chi-square test with Rao-Scott correction, and generalized linear Poisson family models with log link function to assess factors associated with ITV. We calculated crude (CPR) and adjusted (APR) prevalence ratios with their respective 95% CIs. We employed a statistical criterion to choose the variables that we would include in the adjusted model (those with a p < 0.05 in the crude model) and to evaluate the possible collinearity between the covariates included in the final model. Statistical significance was set at p < 0.05.
Ethical Aspects
To carry out this study we used a database provided by the University of Maryland without personal identifiers; for that reason, the study did not require approval from an institutional ethics committee. Participants gave their consent before starting the survey; therefore, their privacy was not compromised.
RESULTS
Characteristics of the study sample
We analyzed a sample of 17,162 adults, from which 49.8% (n = 8512) were male, 47.1% (n = 9124) were younger than 35 years, and 81.2% (n = 14 229) lived in a city. From the total, 29.9% (n = 5264) had suspected COVID-19 symptomatology at the time of the survey, 82.0% (n = 14,026) reported having food insecurity while 90.2% (n = 15,502) reported economic insecurity. In addition, 44.6% (n = 7740) reported that they would have greater acceptance of vaccination if it were recommended by government health authorities, while only 8.8% (n = 1443) would have greater acceptance if the recommendation was made by politicians. 74.9% (n = 13,175) had ITV (Table 1).
Table 1 Descriptive analysis of the characteristics of the study sample (n = 17,162).
| Characteristics | Total | ||
|---|---|---|---|
| Absolute frequency of the included participants | Weighted proportion of each category | ||
| n | % | 95% CI | |
| Gender | |||
| Male | 8512 | 49.8 | 47.3-2.4 |
| Female | 8505 | 49.2 | 46.7-1.8 |
| Non-binary | 145 | 1.0 | 0.8-1.1 |
| Age (years) | |||
| 18-24 | 4260 | 20.1 | 18.5-1.8 |
| 25-34 | 4864 | 27.0 | 26.0-8.0 |
| 35-44 | 3625 | 20.9 | 19.7-2.1 |
| 45-54 | 2494 | 17.1 | 16.4-7.8 |
| 55-64 | 1374 | 9.0 | 8.2-9.8 |
| 65-74 | 468 | 5.2 | 4.2-6.4 |
| 75 or more | 77 | 0.8 | 0.4-1.4 |
| Area of residence | |||
| City | 14,229 | 81.2 | 72.0-7.9 |
| Town | 1756 | 10.8 | 64.8-7.4 |
| Village or other rural area | 1177 | 8.0 | 5.7-11.1 |
| Suspicious symptomatology of COVID-19 | |||
| No | 11,898 | 70.1 | 66.0-3.9 |
| Yes | 5264 | 29.9 | 26.1-4.0 |
| Compliance with community mitigation strategies | |||
| No | 9120 | 54.1 | 51.2-6.9 |
| Yes | 8042 | 45.9 | 43.1-48.8 |
| Food insecurity | |||
| No | 3136 | 18.0 | 15.9-0.4 |
| Yes | 14,026 | 82.0 | 80.0-4.1 |
| Economic insecurity | |||
| No | 1660 | 9.8 | 9.0-10.6 |
| Yes | 15,502 | 90.2 | 89.4-1.0 |
| Fear of a family member getting ill with COVID-19 | |||
| No | 705 | 4.8 | 3.9-6.0 |
| Yes | 16,457 | 95.2 | 94.0-6.1 |
| Probability of vaccination acceptance on the recommendation of family and friends. | |||
| Lower acceptance/Indifferent | 10,238 | 60.0 | 58.3-1.7 |
| Greater acceptance | 6924 | 40.0 | 38.3-1.7 |
| Likelihood of vaccination acceptance on the recommendation of physicians and other health care professionals who provide medical care | |||
| Lower acceptance/Indifferent | 8461 | 50.1 | 48.2-2.0 |
| Greater acceptance | 8701 | 49.9 | 48.0-1.8 |
| Probability of vaccination acceptance based on WHO recommendation. | |||
| Lower acceptance/Indifferent | 7834 | 46.3 | 44.7-7.9 |
| Greater acceptance | 9328 | 53.7 | 52.1-5.3 |
| Probability of vaccination acceptance upon the recommendation of government health authorities. | |||
| Lower acceptance/Indifferent | 9422 | 55.4 | 53.2-7.5 |
| Greater acceptance | 7740 | 44.6 | 42.5-6.8 |
| Likelihood of vaccination acceptance upon recommendation by politicians. | |||
| Lower acceptance/Indifferent | 15,719 | 91.2 | 90.6-1.7 |
| Greater acceptance | 1443 | 8.8 | 8.3-9.4 |
| Intention to be vaccinated | |||
| No | 3987 | 25.1 | 23.0-7.3 |
| Yes | 13,175 | 74.9 | 72.7-7.0 |
| Fear of adverse effects of the vaccine | |||
| No | 1542 | 9.5 | 8.8-10.2 |
| Yes | 15,620 | 90.5 | 89.8-1.2 |
95% CI: 95% confidence intervals.
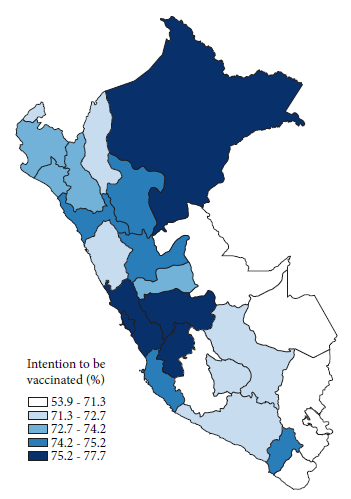
Prevalence of the intention to be vaccinated by departments
The departments with the highest ITV prevalence were provincial Lima (81.4%), metropolitan Lima (77.7%), Junín (76.7%), Callao (75.7%), Huancavelica (75.7%) and Loreto (75.7%). On the other hand, those with the lowest ITV were Madre de Dios (53.9%), Ayacucho (66.1%), Puno (69.5%), Ucayali (69.9%) and Tacna (70.2%) (Figure 1).
Bivariate analysis according to the intention to be vaccinated.
Significant differences were found between ITV and the included covariates, with the exception of age groups (p = 0.213) and compliance with community mitigation strategies (p = 0.062) (Table 2).
Table 2 Descriptive and bivariate analysis of study characteristics according to the intention to be vaccinated in the study sample (n = 17,162).
| Characteristics | Intention to be vaccinated | ||||||
|---|---|---|---|---|---|---|---|
| No | Yes | ||||||
| Absolute frequency of included participants | Proportion weighted according to each category | Absolute frequency of included participants | Proportion weighted according to each category | p-value | |||
| n | % | 95% CI | n | % | 95% CI | ||
| Gender | |||||||
| Male | 1845 | 23.6 | 23.2-26.3 | 6667 | 76.4 | 73.7-78.8 | 0.010 |
| Female | 2091 | 26.3 | 24.5-28.3 | 6414 | 73.7 | 71.7-75.5 | |
| Non-binary | 51 | 37.3 | 23.0-54.1 | 94 | 62.7 | 45.9-77.0 | |
| Age (years) | |||||||
| 18-24 | 971 | 24.4 | 22.1-26.8 | 3289 | 75.6 | 73.2-77.9 | 0.213 |
| 25-34 | 1110 | 25.4 | 22.6-28.5 | 3754 | 74.5 | 71.5-77.4 | |
| 35-44 | 869 | 25.6 | 23.3-28.1 | 2756 | 74.4 | 71.9-76.7 | |
| 45-54 | 589 | 25.1 | 22.3-28.1 | 1905 | 74.9 | 71.9-77.7 | |
| 55-64 | 323 | 25.1 | 22.1-28.3 | 1051 | 74.9 | 71.7-77.9 | |
| 65-74 | 99 | 22.4 | 18.4-27.1 | 369 | 77.6 | 72.9-81.6 | |
| 75 or more | 26 | 35.6 | 25.6-46.9 | 51 | 64.4 | 53.1-74.4 | |
| Area of residence | |||||||
| City | 3146 | 23.7 | 22.0-25.6 | 11,083 | 76.3 | 74.4-78.0 | <0.001 |
| Town | 451 | 28.3 | 25.1-31.7 | 1305 | 71.7 | 68.3-74.9 | |
| Village or other rural area | 390 | 34.6 | 31.2-38.2 | 787 | 65.4 | 61.8-68.8 | |
| Suspicious symptomatology of COVID-19 | |||||||
| No | 2861 | 26.6 | 23.4-29.9 | 9037 | 73.4 | 70.1-76.6 | 0.007 |
| Yes | 1126 | 21.6 | 20.2-23.1 | 4138 | 78.4 | 76.9-79.8 | |
| Compliance with community mitigation strategies | |||||||
| No | 2034 | 24.4 | 22.3-26.7 | 7086 | 75.6 | 73.3-77.7 | 0.062 |
| Yes | 1953 | 25.9 | 23.7-28.2 | 6089 | 74.1 | 71.8-76.3 | |
| Food insecurity | |||||||
| No | 800 | 28.9 | 25.3-32.7 | 2336 | 71.1 | 67.3-74.7 | 0.001 |
| Yes | 3187 | 24.3 | 22.2-26.4 | 10,839 | 75.7 | 73.6-77.8 | |
| Economic insecurity | |||||||
| No | 463 | 31.0 | 27.3-35.1 | 1197 | 69.0 | 64.9-72.7 | <0.001 |
| Yes | 3524 | 24.4 | 22.4-26.6 | 11,978 | 75.6 | 73.4-77.6 | |
| Fear of a family member getting ill with COVID-19 | |||||||
| No | 383 | 56.6 | 61.7-61.4 | 322 | 43.4 | 38.6-48.3 | <0.001 |
| Yes | 3604 | 23.5 | 21.6-25.5 | 12,853 | 76.5 | 74.5-78.4 | |
| Probability of vaccination acceptance on the recommendation of family and friends. | |||||||
| Lower acceptance/Indifferent | 3160 | 33.3 | 30.9-35.8 | 7078 | 66.7 | 64.2-69.1 | <0.001 |
| Greater acceptance | 827 | 12.8 | 11.3-14.4 | 6097 | 87.2 | 85.6-88.7 | |
| Likelihood of vaccination acceptance on the recommendation of physicians and other health care professionals who provide medical care | |||||||
| Lower acceptance/Indifferent | 3431 | 43.3 | 41.0-45.6 | 5030 | 56.7 | 54.4-59.0 | <0.001 |
| Greater acceptance | 556 | 6.9 | 5.8-8.1 | 8145 | 93.1 | 91.9-94.2 | |
| Probability of vaccination acceptance based on WHO recommendation. | |||||||
| Lower acceptance/Indifferent | 3249 | 44.4 | 41.7-47.2 | 4585 | 55.6 | 52.8-58.3 | <0.001 |
| Greater acceptance | 738 | 8.4 | 7.3-9.7 | 8590 | 91.6 | 90.3-92.7 | |
| Probability of vaccination acceptance upon the recommendation of government health authorities. | |||||||
| Lower acceptance/Indifferent | 3585 | 40.7 | 39.1-42.3 | 5837 | 59.3 | 57.7-60.9 | <0.001 |
| Greater acceptance | 402 | 5.8 | 4.4-7.6 | 7338 | 94.2 | 92.4-95.6 | |
| Likelihood of vaccination acceptance upon recommendation by policymakers | |||||||
| Lower acceptance/Indifferent | 3855 | 26.5 | 24.4-28.7 | 11,864 | 73.5 | 71.3-75.6 | <0.001 |
| Greater acceptance | 132 | 10.5 | 8.0-13.6 | 1311 | 89.5 | 86.4-92.0 | |
95% CI: 95% confidence intervals.
Factors associated with the intention to be vaccinated.
In the adjusted regression model, female gender (APR = 0.95; 95%CI: 0.95-0.97; p < 0.001), compared to male gender, was associated with a lower prevalence of having the ITV. Likewise, living in a town (APR = 0.95; 95%CI: 0.91-0.99; p = 0.034), village or other rural area (APR = 0.90; 95%CI: 0.86-0.93; p < 0.001), compared to a city, was associated with a lower likelihood of having the ITV. In addition, having COVID-19 symptomatology (APR = 1.06; 95%CI: 1.03- 1.09; p < 0.001), economic insecurity (APR = 1.04; 95%CI: 1.01-1.06; p = 0.006) and fear of getting sick or having a family member get sick with COVID-19 (APR = 1.49; 95%CI: 1.36- 1.64; p < 0.001) were associated with a higher prevalence of having the ITV. On the other hand, recommendations from WHO (APR = 1.34; 95%CI: 1.29-1.40; p < 0.001), physicians and other health professionals providing medical care (APR = 1.29; 95%CI: 1.26-1.32; p < 0.001), government health authorities (APR = 1.18; 95%CI: 1.15-1.22; p < 0.001), and family and friends (APR = 1.10; 95%CI: 1.08-1.12; p < 0.001), were associated with a higher prevalence of having the ITV. In contrast, recommendations by politicians (APR = 0.89; 95%CI: 0.87-0.92; p < 0.001) were associated with a lower probability of having the ITV (Table 3).
Table 3 Crude and adjusted regression models to assess the association between study characteristics and vaccination intention in the study sample.
| Characteristics | Intention to be vaccinated | |||||
|---|---|---|---|---|---|---|
| Crude | Adjusted | |||||
| CPR | 95% CI | p-value | APR | 95% CI | p-value | |
| Gender | ||||||
| Male | Reference | - | - | Reference | - | - |
| Female | 0.96 | 0.95-0.98 | 0.001 | 0.95 | 0.94-0.97 | <0.001 |
| Non-binary | 0.82 | 0.65-1.04 | 0.104 | 0.86 | 0.73-1.02 | 0.089 |
| Age (years) | ||||||
| 18-24 | Reference | - | - | |||
| 25-34 | 0.99 | 0.95-1.02 | 0.377 | |||
| 35-44 | 0.98 | 0.95-1.02 | 0.345 | |||
| 45-54 | 0.99 | 0.96-1.03 | 0.578 | Not included* | ||
| 55-64 | 0.99 | 0.95-1.03 | 0.624 | |||
| 65-74 | 1.03 | 0.96-1.10 | 0.445 | |||
| 75 or more | 0.85 | 0.73-0.99 | 0.039 | |||
| Area of residence | ||||||
| City | Reference | - | - | Reference | - | - |
| Town | 0.94 | 0.89-,0.99 | 0.021 | 0.95 | 0.91-0.99 | 0.034 |
| Village or other rural area | 0.86 | 0.82-0.90 | <0.001 | 0.90 | 0.86-0.93 | <0.001 |
| Suspicious symptomatology of COVID-19 | ||||||
| No | Reference | - | - | Reference | - | - |
| Yes | 1.07 | 1.02-1.12 | 0.011 | 1.06 | 1.03-1.09 | <0.001 |
| Compliance with community mitigation strategies | ||||||
| No | Reference | - | - | Not included* | ||
| Yes | 0.98 | 0.96-1.00 | 0.062 | |||
| Food insecurity | ||||||
| No | Reference | - | - | Not included** | ||
| Yes | 1.06 | 1.02-1.11 | 0.002 | |||
| Economic insecurity | ||||||
| No | Reference | - | - | Reference | - | - |
| Yes | 1.10 | 1.05-1.14 | <0.001 | 1.04 | 1.01-1.06 | 0.006 |
| Fear of a family member getting ill with COVID-19 | ||||||
| No | Reference | - | - | Reference | - | - |
| Yes | 1.76 | 1.56-1.99 | <0.001 | 1.49 | 1.36-1.64 | <0.001 |
| Probability of vaccination acceptance on the recommendation of family and friends. | ||||||
| Lower acceptance/Indifferent | Reference | - | - | Reference | - | - |
| Greater acceptance | 1.31 | 1.27-1.35 | <0.001 | 1.10 | 1.08-1.12 | <0.001 |
| Likelihood of vaccination acceptance on the recommendation of physicians and other health care professionals who provide medical care. | ||||||
| Lower acceptance/Indifferent | Reference | - | - | Reference | - | - |
| Greater acceptance | 1.64 | 1.59-1.70 | <0.001 | 1.29 | 1.26-1.32 | <0.001 |
| Probability of vaccination acceptance based on WHO recommendation. | ||||||
| Lower acceptance/Indifferent | Reference | - | - | Reference | - | - |
| Greater acceptance | 1.65 | 1.58-1.72 | <0.001 | 1.34 | 1.29-1.40 | <0.001 |
| Probability of vaccination acceptance upon the recommendation of government health authorities | ||||||
| Lower acceptance/Indifferent | Reference | - | - | Reference | - | - |
| Greater acceptance | 1.59 | 1.56-1.62 | <0.001 | 1.18 | 1.15-1.22 | <0.001 |
| Likelihood of vaccination acceptance upon recommendation by politicians. | ||||||
| Lower acceptance/Indifferent | Reference | - | - | Reference | - | - |
| Greater acceptance | 1.22 | 1.19-1.25 | <0.001 | 0.89 | 0.87-0.92 | <0.001 |
95% CI: 95% confidence intervals; CPR: crude prevalence ratio; APR: adjusted prevalence ratio; *Not included because there was no statistically significant association in the crude model. **Not included because of collinearity with economic insecurity.
DISCUSSION
Our results show a high ITV against COVID-19. This is similar to what was found in a multinational study that included Brazil and found that 71.5% of its participants reported a very high or some likelihood of accepting the COVID-19 vaccine 11. In this study, acceptability varied by country, ranging from as high as 90% in China to as low as 55% in Russia 11. Other studies in different countries have also shown different acceptance rates 7 , 14 , 22. The variability among these results may depend on how the research question is posed, which limits comparability 14. For example, a multinational study conducted by the Imperial College of London in November 2020 asked whether there was a “definite intention” to get the COVID-19 vaccine, with responses ranging from 18 to 65% 22. Our study does not pose the answer in terms of a “definite intention”, which would explain the lower percentages.
The variability in the results may also be due to the timing of the study 14. In the United States, the acceptance rate ranged from 72% in April to 48% in October 2020 14. In Italy, vaccine acceptance increased after confinement 23. In Peru, the Ipsos survey showed that the percentage of Peruvians accepting vaccination decreased from 75% in August 2020 to 59% in February 2021 19. The differences found between that survey and our study could be because confidence increased over time due to the advent of vaccines and more information available about vaccines 24. A previous study in countries in the Latin American and Caribbean region, which used the same source of information as this study, reported that the country with the highest ITV was Mexico (88.4%) and the lowest ITV was Haiti (43.2%) 17.
Likewise, it is possible that as the risk perception increased in the country, so did the ITV 14 , 23. In the weeks prior to the survey, due to the increase of the number of cases and deaths 18, the news of the lack of oxygen and available hospital beds may have increased the sense of vulnerability and, with it, the acceptance of the vaccine. A study in Turkey showed that 40% of those who initially had doubts about the vaccine considered it necessary as the pandemic progressed 25. Similarly, in France, more nurses shifted from rejection to hesitancy or acceptance of the vaccine 26.
Similar to our study, other countries show lower ITV in women 14 , 27. Although the reasons for these gender differences are not entirely clear, a European multinational study suggested that it might be due to women showing more concern regarding adverse effects and vaccine safety than men 27.
Although few studies have included rural populations 14, some aspects may explain our finding: living in a village or other rural area was associated with lower ITV. Rural residents are often reluctant to seek medical care or engage in preventive health behaviors compared to urban populations 28. Similarly, difficult access to the Internet limits telemedicine 29 and access to disease- and vaccine-related information, leading to centralization of information and its dissemination by less rigorous means that promote ineffective therapies to the detriment of the vaccine 30.
As with our study, other authors have suggested that the perceived risk of becoming infected, fear of the severity of the disease, a history of having been infected, or knowing an infected friend or relative were predictors of ITV 14. These findings are not limited to the COVID-19 vaccine, as similar results have been found for the acceptability of other vaccines 31. On the other hand, the prospect of not being able to work and the consequent economic insecurity and mental health problems could explain why people with depressive symptomatology and food insecurity are more likely to accept vaccination.
Most studies suggest that the influence of medical advice is the most important factor in accepting vaccination 14. In our study, although the advice of health workers was significant, WHO recommendations were more so. Despite the fact that the WHO disseminated discrepant information during the course of the pandemic 32, its status as the governing body on public health issues gives it credibility, so that reinforcing the importance of its messages would increase the ITV in our population. Similarly, as health workers are an important factor, the dissemination of standardized evidence-based messages should be considered, for example, during teleconsultation or with representative medical figures in regions with lower vaccine acceptance. In China, confidence in physicians as disseminators of vaccine-related information is 80% and in the United States it is 62%. On the other hand, in the United States, only 54% of the population trust the vaccine if it is approved by the Food and Drug Administration (FDA) 14. The fact that politicians’ recommendations are associated with a lower probability of ITV is worrisome, since they are frequently present in the media; however, it is understandable due to the lack of trust in them 33. In the United States, political factors and the influence of former President Donald Trump affected vaccine acceptance, which should also be considered in our country 14.
Our study has some limitations. First, it is based on the responses of users of a social network to which not everyone has access. Nevertheless, it is a social network used by 94% of Peruvians, according to a survey conducted by Ipsos in 2020 34. Secondly, the variables included and their definition are subject to the pre-established definition of the matrix survey. Third, the data were obtained by self-reporting, so there may be an underreporting of information. Fourth, causality cannot be established between the variables evaluated due to the study design. Fifth, the measurements used to assess food and economic security have not been validated, but they provide relevant information for the study. Sixth, the findings could be biased due to the rejection rate of users in a Facebook survey, as well as due to the possibility of occurrence of voluntary response bias. Seventh, some of the associated factors found had a low measure of association, so their interpretation should be done cautiously, despite the statistical significance that the result may have. In spite of this, this is a study with a large sample size with national representativeness that can help to understand the research topic.
In conclusion, three out of four respondents reported having the ITV. Adequate communication strategies based on potentially modifiable factors could increase the possibility of acceptance of the COVID-19 vaccine in our country. Considering that the vaccination campaign will be a long-term task, continuous monitoring of vaccine acceptance is necessary to steer strategies in order to achieve the results proposed by the government.
Acknowledgments:
The authors thank the University of Maryland for conducting the survey with which this study was carried out.
REFERENCES
1. WHO. WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. 2021 [citado el 12 de febrero de 2021]. Disponible en: https://covid19.who.int/. [ Links ]
2. Izda V, Jeffries MA, Sawalha AH. COVID-19: A review of therapeutic strategies and vaccine candidates. Clin Immunol. 2020:108634. doi: 10.1016/j.clim.2020.108634. [ Links ]
3. Bach AT, Kang AY, Lewis J, Xavioer S, Portillo I, Goad JA. Addressing common barriers in adult immunizations: a review of interventions. Expert Rev Vaccines. 2019;18(11):1167-85. doi: 10.1080/14760584.2019.1698955. [ Links ]
4. de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396(10255):898-908. doi: 10.1016/S0140-6736(20)31558-0. [ Links ]
5. Kubin L. Is there a resurgence of vaccine preventable diseases in the US?. J Pediatr Nurs. 2019;44:115-8. doi: 10.1016/j.pedn.2018.11.011. [ Links ]
6. World Health Organization [Internet]. Behavioural considerations for acceptance and uptake of COVID-19 vaccines: WHO technical advisory group on behavioural insights and sciences for health, meeting report, 15 October 2020. 2020 [citado el 12 de febrero de 2021]. Disponible en: https://www.who.int/publications/i/item/9789240016927. [ Links ]
7. Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, et al. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines. 2020;8(3):482. doi: 10.3390/vaccines8030482. [ Links ]
8. Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2):160. doi: 10.3390/vaccines9020160. [ Links ]
9. Sonawane K, Troisi CL, Deshmukh AA. COVID-19 vaccination in the UK: Addressing vaccine hesitancy. Lancet Reg Health Eur. 2021;1. doi: 10.1016/j.lanepe.2020.100016. [ Links ]
10. Pogue K, Jensen JL, Stancil CK, Ferguson DG, Hughes SJ, Mello EJ, et al. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines. 2020;8(4):582. doi: 10.3390/vaccines8040582. [ Links ]
11. Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225-8. doi: 0.1038/s41591-020-1124-9. [ Links ]
12. Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210-e21. doi: 10.1016/S2468-2667(21)00012-8. [ Links ]
13. Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [ Links ]
14. Lin C, Tu P, Beitsch LM. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines. 2021;9(1):16. doi: 10.3390/vaccines9010016. [ Links ]
15. Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg Health Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [ Links ]
16. Ward JK, Alleaume C, Peretti-Watel P, Seror V, Cortaredona S, Launay O, et al. The French public's attitudes to a future COVID-19 vaccine: The politicization of a public health issue. Soc Sci Med. 2020;265:113414. doi: 10.1016/j.socscimed.2020.113414. [ Links ]
17. Urrunaga-Pastor D, Bendezu-Quispe G, Herrera-Añazco P, Uyen-Cateriano A, Toro-Huamanchumo CJ, Rodriguez-Morales AJ, et al. Cross-sectional analysis of COVID-19 vaccine intention, perceptions and hesitancy across Latin America and the Caribbean. Travel Med Infect Dis. 2021;41:102059. doi: 10.1016/j.tmaid.2021.102059. [ Links ]
18. Ministerio de Salud del Perú [Internet]. Sala Situacional COVID-19 Perú: MINSA Lima; 2020 [citado el 12 de febrero 2021]. Disponible en: https://covid19.minsa.gob.pe/sala_situacional.asp. [ Links ]
19. IPSOS [Internet]. COVID-19 y vacunas- Febrero 2021- Encuesta Nacional Urbano Rural. 2021 [citado el 12 de febrero 2021]. Disponible en: https://www.ipsos.com/sites/default/files/ct/news/documents/2021-02/encuesta_nacional_urbano_rural_febrero_2021_-_covid_19.pdf. [ Links ]
20. Barkay N, Cobb C, Eilat R, Galili T, Haimovich D, LaRocca S, et al. Weights and Methodology Brief for the COVID-19 Symptom Survey by University of Maryland and Carnegie Mellon University, in Partnership with Facebook. arXiv preprint arXiv:200914675. 2020. [ Links ]
21. World Health Organization [Internet]. WHO COVID-19: Case definition. 2020 [citado el 12 de febrero 2021]. Disponible en: https://www.who.int/publications/i/item/WHO-2019-nCoV-Surveillance_Case_Definition-2020.2. [ Links ]
22. Imperial College London [Internet]. Covid-19: Global attitudes towards a COVID-19 vaccine. 2021 [citado el 12 de febrero 2021]. Disponible en: https://www.imperial.ac.uk/media/imperial-college/institute-of-global-health-innovation/GlobalVaccineInsights_ICL-YouGov-Covid-19-Behaviour-Tracker_20210520_v2.pdf. [ Links ]
23. Caserotti M, Girardi P, Rubaltelli E, Tasso A, Lotto L, Gavaruzzi T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc Sci Med. 2021:113688. doi: 10.1016/j.socscimed.2021.113688. [ Links ]
24. SAGE [Internet]. WHO Strategic Advisory Group of Experts (SAGE) on Immunization Working Group on COVID-19 Vaccines: Prioritized Infectious Disease and Economic Modelling Questions. 2020 [citado el 12 de febrero 2021]. Disponible en: https://www.who.int/immunization/policy/sage/SAGE_WG_COVID19_Vaccines_Modelling_Questions_31July2020.pdf. [ Links ]
25. Yilmazbas P, Terzi O, Ozceker D. Did. Covid-19 Pandemic Changed Parents' Approach To Vaccination?. Soc Behav. 2021;43(2):130-134. doi: 10.14744/etd.2020.85451. [ Links ]
26. Wang K, Wong ELY, Ho KF, Cheung AWL, Chan EYY, Yeoh EK, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross-sectional survey. Vaccine. 2020;38(45):7049-56. doi: 10.1016/j.vaccine.2020.09.021. [ Links ]
27. Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020. doi: 10.1007/s10198-020-01208-6. [ Links ]
28. Peters DJ. Community susceptibility and resiliency to COVID-19 across the rural-urban continuum in the United States. J Rural Health. 2020;36(3):446-56. doi: 10.1111/jrh.12477. [ Links ]
29. Instituto Nacional de Estadística e Informática [Internet]. Estadística de las tecnologías de información y comunicación de los hogares. 2020 [citado el 12 de febrero 2021]. Disponible en: https://www.inei.gob.pe/media/MenuRecursivo/boletines/boletin_tics.pdf. [ Links ]
30. Espacio y análisis [Internet]. El 90% de muertes asociadas a Covid-19 se encuentran en zonas urbanas. 2021 [citado el 12 de febrero 2021]. Disponible en: https://ojo-publico.com/2003/covid-19-en-regiones-90-de-muertes-esta-en-zonas-urbanas. [ Links ]
31. Schmid P, Rauber D, Betsch C, Lidolt G, Denker M-L. Barriers of influenza vaccination intention and behavior-a systematic review of influenza vaccine hesitancy, 2005-2016. PloS One. 2017;12(1):e0170550. doi: 10.1371/journal.pone.0170550. [ Links ]
32. Soave I [Internet]. Alertas, retrasos, cambios, modelos... Los errores de la OMS en la crisis del coronavirus 2020 [citado el 12 de febrero 2021]. Disponible en: https://www.elmundo.es/ciencia-y-salud/salud/2020/05/02/5ead266e21efa01b6b8b464f.html. [ Links ]
33. IPSOS [Internet]. Opinión Data - Enero 2021. 2021 [citado el 12 de febrero 2021]. Disponible en: https://www.ipsos.com/es-pe/opinion-data-enero-2021. [ Links ]
34. IPSOS [Internet]. Uso de Redes Sociales entre peruanos conectados. 2020 [citado el 12 de febrero 2021]. Disponible en: https://www.ipsos.com/es-pe/uso-de-redes-sociales-entre-peruanos-conectados-2020. [ Links ]
Cite as: Herrera-Añazco P, Uyen-Cateriano A, Urrunaga-Pastor D, Bendezú-Quispe G, Toro-Huamanchumo CJ, Rodríguez-Morales AJ, et al. [Prevalence and factors associated with the intention to be vaccinated against COVID-19 in Peru ]. Rev Peru Med Exp Salud Publica. 2020;38(3):381-90. doi: https://doi.org/10.17843/rpmesp.2021.383.7446
Received: February 23, 2021; Accepted: July 14, 2021











 text in
text in