INTRODUCTION
Neuroendocrine tumors (NET) of thyroid commonly originate from cells derived from the neural crest in the thyroid parafollicular cells or derived from C cells neuroendocrine tissue rise medullary thyroid carcinoma (MTC). This neoplasm is characterized by the elevated calcitonin production, and the concentration levels of this hormone is correlated with the diagnosis 1. Calcitonin is also used as immunohistochemically marker for cytological diagnosis and histopathological MTC 2. However, there are few reports of neuroendocrine thyroid tumors morphologically identical to medullary carcinoma but without calcitonin production 1,3,4. These tumors are rare, so their etiology and clinical presentation remain unknown 1,5. In this context, we report the case of a 49-year old man with the diagnosis of calcitonin negative neuroendocrine thyroid carcinoma.
CASE REPORT
A 49-years old man, referred a 1-year disease time characterized by progressive dysphonia, intolerance liquids and mild dyspnea, he had diagnostic work at another institution with right vocal cord biopsy which reported poorly differentiated neuroendocrine carcinoma. At the physical examination of the head and neck, an enlarged right thyroid lobe of hard consistency was palpated, no cervical adenopathy was found. The nasal fibroscopy showed right vocal cord paralysis and a tumor that partially infiltrates the mucosa of the right subglottic region.
The neck CT scan showed a heterogeneous solid tumor measuring 3.6 x 3 x 3.8 cm dependent on the right thyroid lobe; it infiltrated the larynx at the level of the subglottic region and enveloped the first tracheal ring. It was associated with multiple adenopathy in the right cervical region. The thorax CT scan showed multiple metastatic nodules in both pulmonary fields.
The reviewed pathology slides reported neuroendocrine differentiation of a thyroid carcinoma with the following immunohistochemistry markers: TTF1 (+), Synaptophysin (+), Panqueratin (+), Calcitonin (-), Chromogranin (-), CD20 (-), CD3 (-), CD5 (-), CD23 (-), CD10 (-), Cyclin D1 (-), S-100 (-), Ki 67 (90%) (Figure 1 and figure 2).
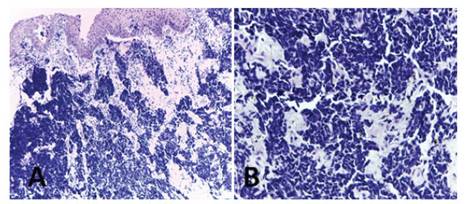
Figure 1 Histopathological study. Hematoxylin eosin stain (A) and (B). Proliferation of small round cells that infiltrate the epithelium.
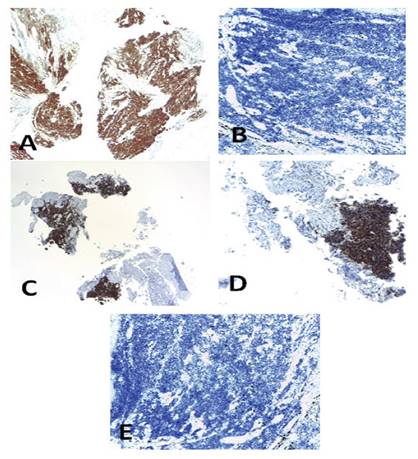
Figure 2 Immunohistochemistry. (A) Ki 67 (90%), (B) ACL, CD 20, CD 3, CD 5, CD 23, CD 10, Cyclin D1, Protein S100 negative; (C) TTF 1 positive, (D) Synaptophysin positive, (E) Chromogranin and calcitonin negative.
In addition, fine needle aspiration cytology of the right thyroid lobe reported a thyroid carcinoma, Bethesda VI, TTF1 (+), Calcitonin (-). Laboratory tests reported CEA: 38.8 ng/ml (Range: 0 to 2.5 µg/l) and serum calcitonin: 6.05 pg/ml (Range < 10 pg/ ml). The patient was diagnosed with locally advanced disease with regional and distant metastasis, therefore a tracheostomy was performed and the patient received systemic therapy. Currently the patient is in his sixth course of Cisplatin and Etoposide, uneventful.
DISCUSSION
Medullary thyroid cancer (MTC) represents 3% to 5% of malignant neoplasms of the thyroid. Calcitonin is a 32-amino acid glycoprotein; high levels of it are found in patients with MTC so its measurement remains the most accurate tool to diagnose and follow up this disease with a global sensitivity of 100%. However, during the last decades several cases of calcitonin negative thyroid medullary carcinoma were reported 6.
In 1998, Schmid et al., used the term “Atypical thyroid medullary cancer” in thyroid tumors with negative calcitonin but showing positive neuroendocrine markers 7; being the negativity of calcitonin the atypical form of an MTC. In 2008, Wang et al., published another case of MTC with negative calcitonin 5; using this term, since the tumor cells were positive for CEA although minimally positive for calcitonin and negative for amyloid. In 2011, Chernyavsky et al., reported another case with calcitonin negative but showing neuron- specific enolase (NSE), synaptophysin and positive thyroglobulin 3; they used the term “Neuroendocrine Thyroid Negative Calcitonin Tumor (CNNET)”. In 2014, Nakazawa et al., used the term “Neuroendocrine carcinoma of thyroid derived from calcitonin-free C cells” in which the tumor cells were negative for calcitonin and positive for neuroendocrine markers, also to rule the diagnosis the peptide immunoreactivity related to the calcitonin gene (CGRP) was used 4,8.
Some theories tried to explain the physiopathology of calcitonin negative in MTC. For example, the dedifferentiation of tumor cells, genetic mutations in calcitonin gene-related peptide (CGRP), defects in the cellular machinery that synthesizes calcitonin, among others 6. Some authors suggest that the loss of the ability to produce calcitonin is due to the dedifferentiation of the tumor, so it could be an indicator of poor prognosis. This mechanism could explain the low serum levels of calcitonin despite the fact that the disease is in advanced stages 9. In support of this theory, Saad et al., described that weak calcitonin staining in immunohistochemistry (IHC) was associated with a worse prognosis 10. Guidelines of the American Thyroid Association on MTC mentioned that a poor calcitonin production could be related to the loss of differentiation, which poor prognosis 2,8. Also, low serum levels of calcitonin have been related to a more aggressive variant of MTC and the presence of early metastasis 5,11. Despite this, Frank-Raue et al, reported that the stage and clinical course of calcitonin negative MTC was not necessarily associated with a poor prognosis 12.
Some tumors showed less aggressive characteristics, such as low Ki-67 staining and RET mutations, but these patients had rapid progression and death. In addition, Saad et al, the weak IHC staining of calcitonin did not correlate with the aggressive histological grade of the tumor or with a worse prognosis 1,12,13.
Another theory that may explain calcitonin negative MTC is the production of precursor peptides and aberrant forms of calcitonin by some tumors, which consequently results in the inability to produce mature calcitonin 14. In the process of calcitonin production, different peptides are created, such as procalcitonin, immature calcitonin, and the byproducts of aminoprocalcitonin and CCP-1 15. The calcitonin antibodies used by various laboratories for immunohistochemistry staining are polyclonal and can detect these peptides. In contrast, immunoradiometric assays use monoclonal antibodies to detect mature calcitonin. Therefore, differences in the specificity of the antibody may account for the discordance between serum levels and immunohistochemistry that is observed in some cases 16. A defect in the cellular secretory apparatus is another hypothesis that could explain the calcitonin negative MTC. This theory may also explain the low levels of other peptides such as chromogranin A and CEA 11.
Because MTC are neuroendocrine tumors, not only is calcitonin, but other immunohistochemistry markers such as neuron-specific enolase (NSE), synaptophysin, and chromogranin A could be used in the diagnosis. In this cases, pathologies such as paragangliomas, metastatic neuroendocrine tumors, hyalinizing trabecular tumors, primary carcinoma of small thyroid cells, among others must be included in the diagnostic workout 7,8.
The main treatment for patients with calcitonin negative MTC is surgery when the disease is localized. When the disease is metastatic disease, the treatment of choice is systemic therapy 3,4,7,8. The lack of marked elevation of calcitonin and other tumor markers, including CEA and chromogranin A, poses a difficulty with respect to surveillance of the disease 5,15.
There are several imaging techniques for the localization of disease recurrence such as computed tomography, magnetic resonance, selective venous catheterization and FDG-PET. Redding et al., followed their patient with serial CT scans of the thorax, pelvis and abdomen 17. Bockhorn et al., recommended cervical ultrasonography every 3 months during the first year as well as chest x-ray and abdominopelvic CT scan 18; in the case of doubtful findings in cervical ultrasonography should be verified with magnetic resonance, if the doubt persists, FDG-PET is recommended 5,13,17,18. Recent publications have compared the role of gallium-68-labelled somatostatin analogues (DOTATATE PET CT), it is an efficient imaging modality in MTC patients for localizing recurrent or metastatic disease. It can be used in patients with any level of increased calcitonin and CEA 19.
In conclusion, negative calcitonin medullary thyroid carcinoma is a rare disease, its etiology still debatable. Immunohistochemistry study is a very important tool, being indispensable specific markers to arrive at its diagnosis. The treatment and prognosis were heterogeneous among the reported cases.














