INTRODUCTION
Colonoscopy is the procedure of choice for diagnosis and therapeutic of the colonic disorders. This method has become the standard criterion for screening of colorectal cancer (CCR) because of its high accuracy for the diagnosis of early-staged cancer and its precancerous lesions (conventional adenomas and serrated colorectal lesions) 1.
Despite the recent progress in the field of colonoscopy (high-definition endoscopes, virtual chromoendoscopy, wide-angle colonoscopies, retrograde viewing devices and devices to attach to colonoscope) 2, adequate bowel preparation is still one of the most important factors related to the yield of colonoscopy 3. Low-quality bowel preparation has been associated with lower adenoma detection rate and cecal intubation rate; and greater need for earlier repeat colonoscopy than recommended intervals 4,5. Moreover, improper cleaning significantly increases hospital stays and healthcare expenses 6,7. Bowel preparation is perceived as an unpleasant experience by most patients, which represents a major barrier to undergo colonoscopy 8. Thus, better tolerance profiles of laxative agents are necessary to increase the adherence of patients to this procedure.
Currently, there are different available cleansing formulations used for bowel preparation. Nevertheless, none of them meet all the criteria of an ideal agent (high quality of bowel cleansing, safety, convenience, tolerability and affordability) 9,10. Polyethylene glycol (PEG) regimens are widely recommended as laxative agents for routine colonoscopy by most of the endoscopy societies 3,10. Those regimens provide a high quality of bowel preparation and are considered safe in most cases. However, small groups of patients have poor compliance and tolerability to PEG-based regimens due to its side effects and/or high volume necessary to complete the preparation (11,12.
Although mannitol solution is avoided in several countries due to anecdotal cases of colonic explosion, it is routinely used as a laxative agent in most of the healthcare centers in Brazil and in some centers in Venezuela and Colombia because of its low costs, high quality bowel cleansing and low complication rates 13-16.
This study was aimed to assess tolerance and acceptability of the bowel preparation using either PEG or mannitol solution.
MATERIALS AND METHODS
Study design
This was a prospective, transversal, randomized study of patients underwent colonoscopies that received either PEG or mannitol solution as bowel preparation. This study followed the Declaration of Helsinki and was approved by the ethics committee of the Department of Medical Education and Research, Escuela de Ciencias de la Salud “Francisco Battistini Casalta”, Universidad de Oriente.
Patients
We enrolled prospectively 140 patients who met the selection criteria from the gastroenterology consultation of three healthcare centers in Venezuela: Centro Clínico Andrés Bello, Ciudad Bolívar (n=50); Hospital Militar “Dr. Carlos Arvelo”, Caracas (n=40) and Hospital de Clínicas Caracas, Caracas (n=50), between August and October, 2018. All patients were fully informed about the procedure and provided written informed consent.
Selection criteria included: Adult patients with indications of screening for CRC or with suspected large bowel diseases. Exclusion criteria were as follows: bowel obstruction, pregnant women, hemodynamic instability, hypersensitivity to PEG or mannitol solution, illiterate patients or unable to complete the questionnaires.
Patients were allocated to receive either PEG or mannitol solution by simple random sampling.
Diet
Patients received a dietary plan with a low-fiber diet, which had to be started in the morning of the day preceding colonoscopy.
PEG preparation
A PEG-electrolyte powder was used (Colayte®, Renova Industria Farmacéutica, Venezuela). Each package of Colayte® contains: PEG 3350 60 g, sodium chloride 1.460 g; potassium chloride 0.745 g; sodium bicarbonate 1.680 g and anhydrous sodium sulfate
5.680 g. Each package was diluted in one liter of water. Preparation was standardized as follows: the day before the examination, the patient received 2 l of PEG solution, beginning at 8 p.m. (1 glass of 250 ml every 10 minutes). On the day of colonoscopy, the patient drank other 2 l of PEG solution, beginning at 4 a.m.
Mannitol preparation
A 10% mannitol solution (Laboratorio Behrens, Venezuela) was used. Each 500-ml-bottle of mannitol was further diluted in 500 ml of water. The preparation was divided into two phases. On the day preceding colonoscopy, the patient was given one liter of mannitol (500 ml of mannitol + 500 ml of water), beginning at 8 p.m. (1 glass every 10 minutes). On the day of colonoscopy, the patient took another liter of the mannitol solution, beginning at 4 a.m.
Colonoscopic procedure
The procedure was performed in a digestive endoscopy unit in the morning with conscious sedation. The colonoscope was introduced into the rectum and under direct visualization advanced to the cecum. Bowel preparation was scored by using the Boston Bowel Preparation Scale (BBPS) (17. During the withdrawal of the scope, the colonic mucosa was inspected, findings were recorded, biopsies were taken and therapeutic procedures were performed when necessary. After the procedure, the patients were taken to a recovery room.
Questionnaires
A questionnaire about the bowel preparation experience was given to the patients after they had left the recovery room. The questionnaire had three parts. The first part assessed the tolerance by nine 4-point scale questions (1=none, 2 =mild, 3=moderate and 4=severe). The items evaluated were nausea, abdominal pain, bloating, anal irritation, and overall experience during the preparation and post-procedure discomfort, disagreeable flavor, burden of the volume ingested and cost of the preparation. The second part was a question about the most unpleasant burden of the preparation. The last one evaluated the acceptability by asking the willingness to use the same bowel preparation in future colonoscopies.
RESULTS
One hundred forty patients were randomized in groups (PEG group: n=70; mannitol group: n=70). The mean age was 58.94 years with a standard deviation of
14.38 years. Screening for colorectal cancer (55.7%) was the most frequent indication for colonoscopy. Thirty percent of the patients had no pathological findings during the colonoscopy. Baseline patient and clinical characteristics are summarized in Table 1.
Table 1 Baseline and clinical characteristics.
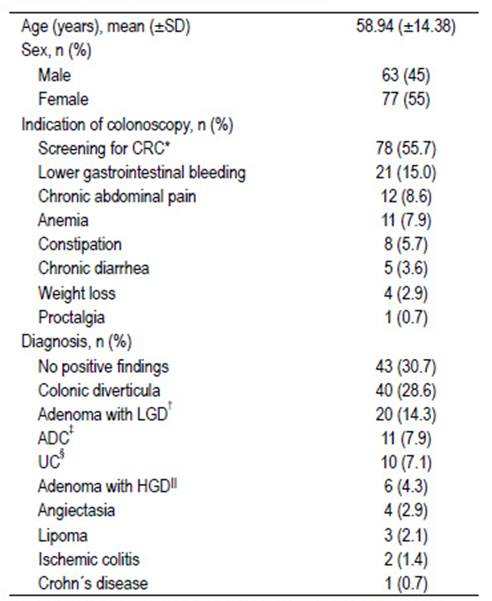
*Colorectal cancer; †Low-grade dysplasia; ‡Adenocarcinoma; §Ulcerative colitis; IIHigh-grade dysplasia.
High quality of bowel preparation was achieved in both groups. The mean of the BBPS score was 8.06 ± 0.96 and 8.10 ± 0.96 in the mannitol group and in the PEG group, respectively (p=0.75). Cecal intubation was possible in all cases.
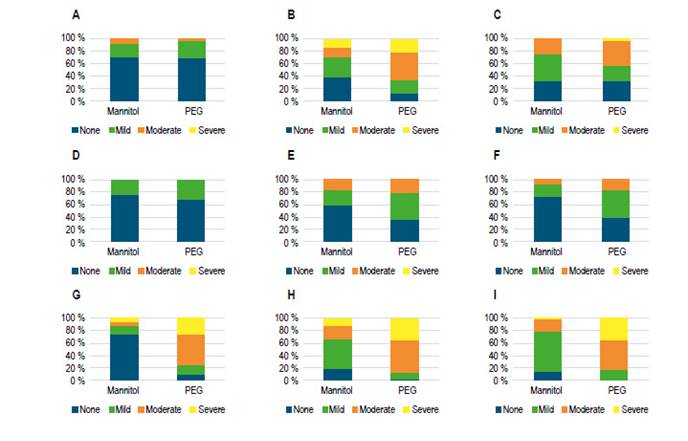
Figure 1 shows the differences of burden according to the answers from the questionnaires between the mannitol group and the PEG group. Patients perceived more burdensome the bowel preparation with PEG than mannitol solution for the variables nausea, overall experience, post-procedure discomfort, disagreeable flavor, volume ingested and cost (p<0.05). A similar tolerance was reported for abdominal pain, bloating and anal irritation (p>0.05) (Table 2).
Table 2 Differences of tolerability of the bowel preparation according to a 4-point scale* questions.
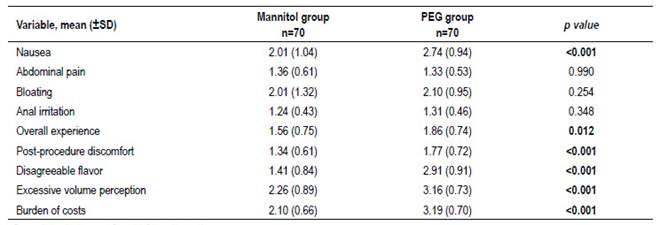
*Four-point scale: 1=none; 2 =mild; 3=moderate; 4=severe
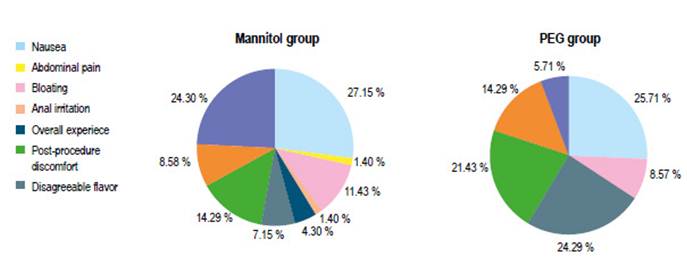
The most unpleasant burden in the mannitol group was nausea (27.1%), followed by volume ingested (14.2%), whereas in the PEG group, nausea (25.7%) and disagreeable flavor (24.2%) were the worst burdens. It should be noted that in the mannitol group, 24.3% of the patients reported none major burden (Figure 2).
The same type of bowel preparation would be used again in future colonoscopies in the 82.9% of the patients from the mannitol group versus 71.4% of the patients from the PEG group (p=0.10).
DISCUSSION
A High-quality bowel preparation is a key element for the success of colonoscopy because is related to higher adenoma detection rate and lower healthcare costs and complication rates during the procedure. Therefore, the factors that influence on the bowel preparation can also impact the yield of colonoscopy. Bowel preparation remains one of the main impediments to undergo colonoscopy since it is usually perceived as an unpleasant experience by most patients (8,18. Moreover, greater technical difficulty and lower accuracy of colonoscopy have been associated with a patient-perceived negative experience of bowel preparation 19.
PEG is an isotonic agent, which passes through the bowel with neither absorption nor secretion. The use of PEG-electrolyte solutions is considered the standard regimen of bowel preparation 10. This formulation achieves high quality of bowel cleansing compared with other agents. However, many patients report low tolerance due to its disagreeable flavor and burden associated with the larger volumes intake, routinely 2-4l 20,21. Moreover, in some developing countries, PEG-based regimens are expensive and unavailable 22.
Mannitol is an osmotic diuretic agent, which is insignificantly absorbed by the gastrointestinal tract when is administered orally, leading to an osmotic diarrhea 23,24. This formulation has been used as bowel preparation for colorectal surgery and colonoscopy in several countries because of its low cost, easy administration, pleasant flavor, good tolerability and high quality of bowel cleansing (16,22,25,26. Despite this fact, this formulation has been avoided in the United States and Europe due to a few cases of colonic explosion during therapeutic colonoscopy27-31.To trigger a colonic explosion, the presence of combustible gases like hydrogen and methane, presence of oxygen (concentration above 5%) and application of a heat source are necessary. As a non-absorbable carbohydrate, mannitol is fermented by bacteria in the colonic lumen, which produces hydrogen and methane. Concentration of hydrogen and methane must be above 4% and 5%, respectively to be considered potentially explosive 32. Nonetheless, in a study by Paulo et al.9, in which the methane concentration was measured both during colonoscopy and after gas exchange (air insufflation and aspiration) in patients who had received either mannitol or sodium phosphate, none of the patients in the mannitol group had detectable levels of methane after gas exchange. Therefore, those results showed the mannitol use was as safe as sodium phosphate considering methane measurements.
In the current study, the difference in the cleansing quality was not statistically significant between the mannitol group and the PEG group, achieving BBPS scores ≥6. This fact has been reported in several trials, which have shown high levels of cleanliness of the colon in both types of formulations 14-16. In a study by Vieira et al. 14, patients who received mannitol achieved a mean BBPS score 8.50 versus 8.54 in the group that took the PEG regimen, which is similar to the findings in our study (mannitol group: 8.06 versus PEG group: 8.10).
There were differences of tolerability between both sorts of cleansing agents in the present study. In the mannitol group, nausea, overall experience, post procedure discomfort, disagreeable flavor and volume ingested were less burdensome than in the PEG group. On the other hand, abdominal pain, bloating and anal irritation were well tolerated in both groups without significant differences. We included in the questionnaire the item burden of the preparation cost, which has been not included in previous researches. The cost of the preparation was more burdensome in the PEG group than in the mannitol group. Our results contrast with those obtained in the study by Vieira et al. 14 in which the patients reported more burden in the mannitol group than in the PEG group. This fact could be explained by the additional dilution of 500 ml of 10% mannitol in 500 ml of water that we performed, as well as, it was given a split-dose of mannitol solution (1 l of the preparation the night before and then 1 l the at the same day of the colonoscopy) instead of a single dose at the same day of the colonoscopy.
In both groups nausea was the main burden of the bowel preparation, which is consistent with the results of previous researches 15,16. Even though split dose bowel preparation was used in both groups, patients still perceived nausea as a major complaint. Nevertheless, nausea was less burdensome in the mannitol group. None of the patients were unable to complete the preparation because of this burden. We usually advise patients with nausea to space the intake of the preparation every 30 minutes, which manages to mitigate this complaint in most cases.
No significant differences were found with regard to acceptance between the Mannitol and PEG groups. Both groups showed high levels of acceptability (mannitol group: 82.9% versus PEG group 71.4%, p=0.10). However, the mannitol solution was perceived more tolerable.
This study has some limitations that should be discussed. First of all, it was not a blinded study, which could have led to observer bias. Secondly, the sample size was relatively small because most of the patients who attend to the gastroenterology consultation in our country cannot afford the costs related to colonoscopy, which makes it difficult to generalize our findings. Due to those limitations, we suggest carrying out multicenter, double-blind studies with larger sample size in order to corroborate the results of the present study.
In summary, acceptance of the bowel preparation between mannitol solution and PEG was comparable. Nevertheless, mannitol solution was better tolerated by patients in regard to overall experience, nausea, post-procedure discomfort, disagreeable flavor, volume ingested and cost. Thus, mannitol solution seems to be a safe alternative to bowel cleansing before colonoscopy.