Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Estomatológica Herediana
versão impressa ISSN 1019-4355
Rev. Estomatol. Herediana vol.28 no.3 Lima jul. 2018
http://dx.doi.org/https://doi.org/10.20453/reh.v28i3.3394
Artículo Original
Impact of oral conditions on quality of life in schoolchildren in urban area of Cuenca-Ecuador
Impacto de las condiciones orales sobre calidad de vida en escolares del área urbana de Cuenca-Ecuador.
Neli Gomescuello 1,2,a, Carmen Rosa García-Rupaya 2,b, César del Castillo-López 2,c
1 Universidad Técnica Particular de Loja. Loja, Ecuador.
2 Facultad de Estomatología Roberto Beltrán, Universidad Peruana Cayetano Heredia. Lima, Perú.
a Doctor en Odontología. Maestría en Gerencia en Salud. Maestría en Estomatología.; b Especialista en Carielogía y Endodoncia, Magister en Estomatologia, Docente del Departamento Académico de Medicina, Cirugía y Patología Oral. ; c Especialista en Salud Pública. Magíster en Estomatología. Magíster en Salud Pública. Docente del Departamento Académico de Odontología Social.
RESUMEN
Objetivos: Determinar Impacto de las Condiciones Orales sobre la Calidad de Vida Relacionada a Salud Bucal (CVRSB) en escolares de dos escuelas urbanas, Cuenca – Ecuador el año 2015. Material y métodos: Estudio transversal, que valoró a 208 escolares de 11 y 12 años, de las escuelas Ezequiel Crespo y Ulises Chacón, de Cuenca, Ecuador. Se determinó un promedio de edad de 11,48 ± 0,501, donde 159 (76,44%) fueron varones y 49 (23,56%) fueron mujeres, se aplicó el instrumento Child Oral Impacts on Daily Performance Index (Child OIDP Index) en español, versión validada en Perú que permite evaluar los impactos de 17 condiciones orales sobre 8 desempeños diarios. Resultados: Las prevalencias de las condiciones orales autopercibidas como problema fueron: posición de dientes (54%) y diente cariado (52%), los impactos en desempeños diarios más afectados fueron: sonreír (38%) y comer (36%). Conclusiones: El Índice Child-OIDP Index promedio global fue de 9,79 ± 7,02, considerado alto.
PALABRAS CLAVE: Calidad de vida, salud bucal, escolares, urbano, Child OIDP.
SUMMARY
Objectives: To determine the Impact of the Oral Conditions on the Quality of Life Related to Oral Health (QLROH) in schoolchildren of two urban schools, Cuenca Ecuador in 2015. Materials and methods: Cross-sectional study that evaluated 208 schoolchildren aged 11 and 12 from the Ezequiel Crespo and Ulises Chacón schools in Cuenca, Ecuador. An average age of 11.48 ± 0.501 was determined, where 159 (76.44%) were male and 49 (23.56%) were female. The Child Oral Impacts on Daily Performance Index instrument (Child OIDP Index) was applied in Spanish, version validated in Peru that allows to evaluate the impacts of 17 oral conditions on 8 daily performances. Results: The prevalences of+ self-perceived oral conditions as a problem were: position of teeth (54%) and decayed tooth (52%), the impacts on daily performance most affected were: smiling (38%) and eating (36%). Conclusions: The global average Child-OIDP Index was 9.79 ± 7.02, considered high.
KEYWORDS: Quality of life, oral health, schoolchildren, urban, Child OIDP.
INTRODUCTION
In Ecuador one of the goals established by the World Health Organization (WHO) and the International Dental Federation (FDI) for the year 2000 was that 50% of the population at the age of 6 years should be free of cavities. However, the National Epidemiological Study of Oral Health in Children under 15 years of Ecuador 2009 2010 reveals that only 20.1% of schoolchildren in Ecuador at that age are healthy, so there is still a high Caries prevalence in Ecuadorian children (79.9% at 6 years and 88.2% in the school group from 6 to 15 years old) (1). Consequently, the Ecuadorian health system is focused on controlling the disease (2). In 2009, the Ministry of Public Health of Ecuador (MSP) approved the Standardization of the National Health System, Oral Health Area (3), and in 2013 the “National Plan for Good Living” (4).
In recent years, oral health and its deterioration have been related to emotional and social perceptions. In this sense, Quality of Life is defined as: “the perception of the individual about his position in life within the cultural context and the value system in which he lives and with respect to his goals, expectations, norms and concerns” (5), being the best way to measure and evaluate this relationship through a multidisciplinary approach (5), using instruments that integrate clinical and psychometric aspects through analog scales designed to measure HRQOL in children such as the Child OIDP index, instrument developed by Gherunpong et al., (6,7); validated in several countries and languages (8-11) is an instrument that relates the impact of 17 oral conditions, on 8 habitual performances that characterize well-being and HRQOL in adolescents (6,7).
In the present study, the instrument validated in Peru was used in the same way that they used: Sánchez et al., (12); which evaluated the impact of oral conditions on quality of life in four public schools in Puente Piedra, Lima; finding that the prevalence of impacts of oral conditions on daily performances was 82.0% and the Index reached an average score of 7.77. On the other hand, Del Castillo (13) in the rural area of Piura, could determine that 88.7% of schoolchildren reported one or more of an impacted performance (Child-OIDP> 0) and the average of self-perceived oral conditions as a problem was 1.14 ± 0.66 conditions. Also, Paredes in a school in San Juan de Miraflores, Lima; in 2013, in 169 schoolchildren, it was determined that the prevalence of the impact of oral conditions on the quality of life of 11and 12-years-old school children was 100%, with at least one daily performance impacted, being the most affected: eating and smiling (14).
On the other hand, Ingunza in Callao, Lima, using the Child OIDP Index in 132 schoolchildren found that 100% of the schoolchildren interviewed reported at least one affected daily performance and the average of self-perceived oral conditions as a problem was 4.52 ± 1.96; finally the global Child-OIDP Index was 9.71 ± 7.63, where eating performance was the highest, mainly due to tooth pain (15). All these studies show self-perceived oral conditions that affect the quality of life related in oral health.
The objective of this study was to determine the impact of oral conditions on the quality of life of 11and 12-year-old schoolchildren in public elementary schools Ulises Chacón and Ezequiel Crespo Ambrosi, located in the urban area of the city of Cuenca. Ecuador, the year 2015.
MATERIALS AND METHODS
Descriptive and cross-sectional study, the population consisted of 284 schoolchildren from two public, urban schools in the city of Cuenca, Ecuador. Simple random sampling was used and 106 schoolchildren were sampled, however the sample was finally made up of 208 schoolchildren of 11 and 12 years old, of both sexes. An average age of 11.48 ± 0.501 was determined, where 159 (76.44%) were male and 49 (23.56%) were female. This was handled and was approved by the Institutional Ethics Committee of the Universidad Peruana Cayetano Heredia No. 118-07-15 (from March 22, 2015); for conducting the research was calibrated by an expert, it was approved of the school authorities, the informed consent of the parents and the informed consent of the schoolchildren; in addition, the respective selection criteria were considered. The questionnaire was administered individually, using a school time of 8 to 10 minutes, in the first hours of the school day.
The data collection was carried out in two stages: In the first stage, the students were asked to identify from a list of the 17 oral conditions, those that produced oral health problems in the last three months, and for a positive response they were asked which of these problems made it difficult for them to perform any of the eight daily tasks: eating, talking, cleaning their mouths, sleeping, emotion, smiling, studying and socializing. For frequency the student was asked that according to the problems he pointed out in the mouth or teeth, the difficulty for (performance) has been presented to him: once or twice in a month? (which corresponds to value 1); three or more times in a month? (for value 2) or more than three times in the last three months? (according to the scale corresponds to value 3). The second part, following the scheme suggested by Gherunpong et al (7); allowed to determine: Severity, intensity and extent of the impact. In severity, a sheet with a growing arrow was presented to the scholar where, he identified, the severity with ranges corresponding to (1 little, 2 regular, 3 a lot).
The scores of the Child-OIDP Index or the impact of the oral conditions on each daily performance were calculated by multiplying the severity of the impact by frequency (1,2,3) of the impact for each habitual performance (range 0 to 9) and obtaining the average score for each performance and for the total performance (range 0 to 72) then multiplying by 100; and dividing it by 72; from which the overall score of the Child-OIDP Index is extracted whose highest values indicate a greater change in quality of life.
To determine the intensity, it was necessary to count on the frequency, and this is valued in five categories, from “very low intensity”, “low”, “moderate”, “severe”, to “very severe intensity” and finally; extension of the impact of oral conditions on performance, corresponded to the number of daily performances affected, which could range from the value 0 (which means no performance impacted) to the value 8 (all performances impacted) and averaged the number of performances impacted among school children.
Absolute and relative frequency distribution tables are presented, means and standard deviations were calculated. The bivariate analysis was carried out using the Chi-Square test and Mann-Wihtney U test to associate HRQoL with sex. For the analysis of the extension according to covariates, the Test T test was used. The p value, or value of statistical significance, was extracted and the study had a confidence level of 95%.
RESULTS
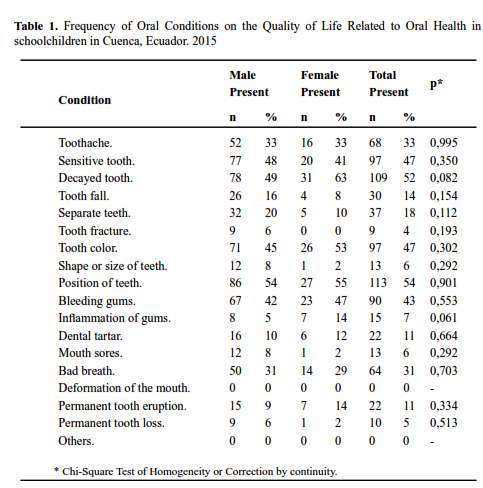
In the present cross-sectional study carried out in the urban area of Cuenca, Ecuador, a sample of 208 schoolchildren aged 11 and 12 years was compiled, who met the selection criteria and their parents gave their informed consent and the schoolchildren gave their assent. It was determined that of the 17 oral conditions self-perceived as problems, (Frequency of schoolchildren with one or more impacts of oral conditions) the most frequent conditions were: Position of teeth with 113 schoolchildren (54.3%), decayed tooth 109 schoolchildren (52%) and with the same number of sensitive tooth and color of the teeth with 97 schoolchildren (47%); It is important to mention that 90 schoolchildren manifested gum bleeding (43%); while the less frequent ones were: tooth fracture and tooth loss; likewise none reported self-perceived deformity of the mouth. No statistically significant association was found between sex and self-perceived oral conditions as a problem (table 1).
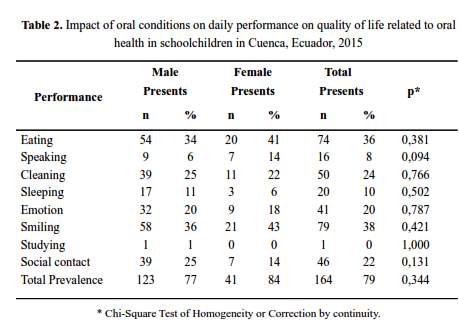
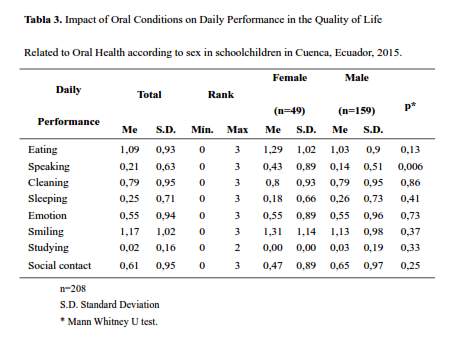
Regarding the daily performances that suffer impact, the most impacted and important were: smiling (38%), then eating (36%), cleaning the mouth (24%) and interact with friends (22%). It is important to mention that it was determined that for smiling performance, the highest frequency occurred in the group of women (43%) compared to that of men (36%), however, no statistically significant association was found (Table 2). The prevalence of school children who indicated some impact of oral conditions on their daily performances was high (79%) (table 2); when determining the severity of the impact (or degree of difficulty to develop the daily performances) in a global way, the performance that presented the highest value was: smiling 1.17 (± 1.024); then eating 1.09 (± 0.934), and then cleaning the mouth 0.79 (± 0.95). Only for performance, speaking 0.21 (± 0.632); a statistically significant difference was found between both sexes (table 3). When comparing severity according to sex, the highest was found coincidentally for women to smile at 1.31 (± 1.14) and 1.13 (± 0.98) (table 3).
The overall average of the Child-OIDP Index was determined, which was 9.79 (± 7.020); the highest values of the global average in the daily activities were for smiling 2.75 (± 2.88); followed by eating 1.94 (±2.07); with values ranging from 0 to 9; the least impacted was studying 0.03 (± 0.317) (table 4).
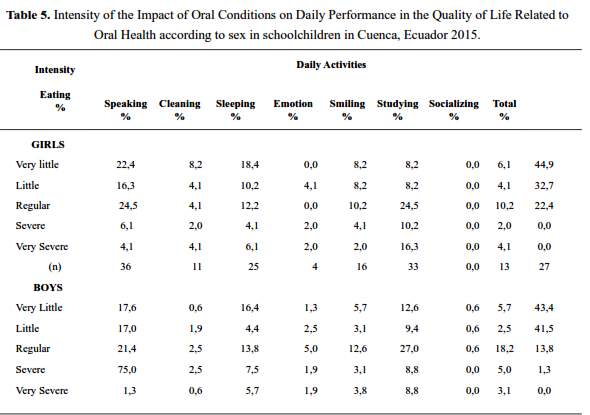
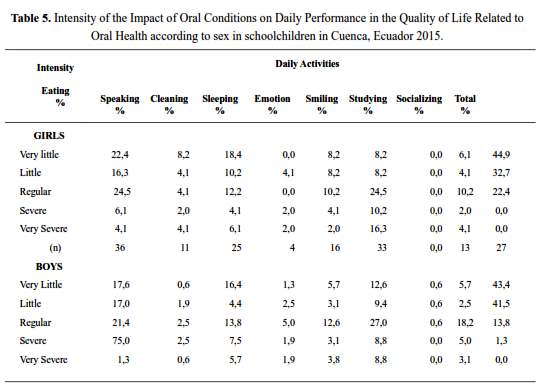
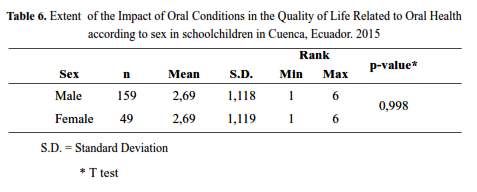
With regards to the intensity of impact, the majority was located in “very little” (44.90%) followed by the “little” level (table 5). The extent of the impact presented a mean of 2.69 (S.D. 1,118 males) with a minimum of 1 affected performance and a maximum of 6, without finding statistically significant differences between both sexes (p ˃0.05) (table 6).
DISCUSSION
The present investigation was carried out with schoolchildren of 11 and 12 years old, from the urban area of Cuenca, Ecuador; applying the Child Oral Impacts on Daily Performance instrument (Child OIDP Index) in Spanish, validated in Peru; likewise, lines of research have been presented using this instrument in relation to quality of life in Ecuador (16,17). In this study, a high prevalence of the impact of oral conditions on CVRSB was found in 79% of the sample, consistent with studies conducted in Peru by Sánchez (12) in Zapallal with 82.0%; Del Castillo in Piura with 88.7% (13). Major prevalences are found in Apurimac, Abancay by Tineo with 99.2% (18); likewise, Paredes (14) in the district of San Juan de Miraflores, and Ingunza (15) that reached 100%, the latter in Lima. In Brazil Castro (24) found 80.7%, higher figures were found in Thai teenagers by Gherunpong (25) with 89.8% and, lower in Italian schoolchildren by Bianco (21) with 66.8%; in the study conducted by Nurelhuda in Sudan (22) found 54.6%, Nucã in Romanian schoolchildren (26) found 64.9%, Yusuf in validating the instrument in English children (27) found 40.4%; and finally Cortes in Spanish children (23) found 30.5%.
The participants in this study reported 16 of the 17 oral conditions, consistent with Ingunza (15), and indicated in order: position of the teeth, decayed tooth, sensitive tooth, color of the teeth. Coinciding with the studies of Del Castillo (13); who reports sensitive teeth and decayed teeth as the second and third most frequent conditions; and Paredes (14) and Ingunza (15), sensitive tooth. Regarding the daily performances for both sexes, the most affected found in the present study was smiling (38%), eating (36%) and cleaning the mouth (24%); agreeing with Del Castillo (13) on the impact of eating (62.7%) and Paredes (14) sequentially found eating, smiling and cleaning, and Ingunza (15) eating and cleaning the mouth.
In severity of the impact, higher averages were found for smiling 1.17 (± 1.024); eating 1.09 (± 0.934) and cleaning the mouth 0.79 (± 0.095); coinciding with Del Castillo (13) for performance eating with 1.07 (±0.96); Paredes (14); 1.45 (± 1.38) in eating, and Ingunza (15) in eating 1.34 (± 0.94) and cleaning the mouth 1 , 03 (± 0.96). The lowest values were for the performances of studying 0.02 (± 0.16) and speaking 0.21 (± 0.63).
The findings in intensity were located at a global level in “very low intensity” for men in (43.4%) and (44.9%) for women; “low intensity” (41.5%) in men and (32.7%) in women being higher for smiling, then eating and cleaning their teeth; with significant differences according to sex for speech performance, having a greater impact on women with a p = 0.006 value. In this variable, Del Castillo (13) reports global levels of “very low intensity” (67.7%); with the highest performances being socialized (54.5%) smiling (46.9%) and studying (37.9%) ) and “low intensity” (21.8%) to sleep (44.4%), clean teeth (38.5%) and study (37.9%). Paredes (14) (38.5%), found “very low intensity” and (33.7%) “low intensity”, while Ingunza (15) (61.4%) “very low intensity” and (19),(7%) “low intensity”.
In the extension of the impact, in the present study it was evident that all the students showed a minimum of one and a maximum of six, of eight performances, which differs with the studies of Del Castillo (13), Paredes (14) and Ingunza (15), who obtained averages that varied between zero and eight. No statistically significant differences were obtained.
In this study, the global average of the Child-OIDP Index was high, of 9.79 (± 7.020); similar to Ingunza (15) 9.71; the lowest found was that of Del Castillo (13) 7.05, in the range of 1 to 35. It was found in performances, smiling 2.75 (± 2.88); followed by eating 1.94 (± 2.07) and cleaning the mouth 1.70 (± 2.54); with values ranging from 0 to 9 in all three cases, close to the findings obtained by Del Castillo (13); eating 1.59 (± 1.77) and cleaning the mouth 1.43 (± 1.61) in ranges from 0 to 9 and from 0 to 6, respectively. It is important to mention that Piaget (32,33); considers that in this age (11 and 12 years), the participants already consolidate the abstract thought, therefore; they perceive their poor dental position, this affects the aesthetic image and affects their self-esteem. In conclusion, the impact of oral conditions on the quality of life related to oral health in urban schoolchildren in Cuenca, Ecuador; it is high with a prevalence of 79% of school children. The oral condition most indicated by the schoolchildren was the positioning of the teeth and by relating the oral conditions with the daily performances and determining the impacts; smiling, the most affected performance. The average severity of the highest impact was found in eating performance. The overall average of the Child-OIDP Index was high, when compared with other investigations. The severity of the impact for schoolchildren of both sexes was found mostly in “moderate” or “regular”. The intensity of the impact for schoolchildren of both sexes was found mostly in “very little” and “little”. An average considered low was reached for the extension of impacts; coinciding in men and women.
Consequently, it allows us to recommend the urgent need to understand that the measurement of the physical affectation in the oral cavity is not complete when not considering the psychosocial dimension of the person.
REFERENCES
1. Organización Mundial de la Salud. Estudio Epidemiológico Nacional de Salud Bucal en Escolares Menores de 15 años de Ecuador 2009 – 2010. Boletín Informativo. 2011;29:66-68. [ Links ]
2. Ministerio de Salud Pública del Ecuador; Organización Panamericana de Salud, DNE. Estudio Epidemiológico de Salud Bucal en Escolares Menores de 15 Años del Ecuador, Quito, Ecuador, 1995 1996. Quito: Ministerio de Salud Pública del Ecuador; 2000 [ Links ]
3. Ministerio de Salud Pública del Ecuador. Plan Nacional de Salud Bucal: Proceso de Normatización del Área de Salud Bucal. Quito: Ministerio de Salud Pública del Ecuador; 2009. [ Links ]
4. Martins S, Álvarez E, Abanto J, et al. Epidemiología de la caries dental en américa latina: Relatorías de la mesa de representantes de sociedades de Odontopediatría de los países Latinoamericanos. ALOP. 2014;4(2):0-0. [ Links ]
5. WHO-QOL Group. The World Health Organization Quality of Life assessment: Position paper from the World Health Organization. Soc Sci Med. 1945: 41(10):1403-9. [ Links ]
6. Gherunpong S, Sheiham A, Tsakos G. A sociodental approach to assessing dental needs of children: concept and models. Int J Paediatr Dent. 2006; 16(2):81-88. [ Links ]
7. Gherunpong S, Tsakos G, Sheiman A. Developing and evaluating an oral health-related quality of life index for children; the Child-OIDP. Community Dent Health. 2004; 21(2):161-9. [ Links ]
8. Misrachi C, Espinoza I. Utilidad de las mediciones de la calidad de vida relacionada con la salud. Revista Dental de Chile. 2005; 96(2):28-35. [ Links ]
9. Moreno X, Vera C, Cartes R. Impacto de la salud bucal en la Calidad de Vida de escolares de 11 a 14 años, Licatén. Chile. Rev Clin Periodoncia Implantol Rehabil Oral. 2014; 7(3):142-148. [ Links ]
10. Rosel E. Evaluación del Programa de Asistencia Dental Infantil en Andalucía: Salud Oral y Calidad de Vida Oral 2009. PhD Thesis. Granada: Facultad de Odontología España, Universidad de Granada; 2009. [ Links ]
11. Bernabé P, Sheiham A, Tsakos G. A comprehensive evaluation of the validity of Chid-OIDP: further evidence from Peru. Community Dent Oral Epidemiol. 2008; 36(4): 317-25. [ Links ]
12. Sánchez P. Impacto de las condiciones orales sobre la calidad de vida en escolares de 11 y 12 años de edad de Zapallal-Puente Piedra, Lima. Lima: Facultad de Estomatología Perú, Universidad Peruana Cayetano Heredia; 2007. [ Links ]
13. Del Castillo C. Impacto de las condiciones orales sobre la Calidad de Vida Relacionada a la Salud (CVRS) de escolares del ámbito rural de Piura en el año 2010. Master thesis. Lima: Universidad Peruana Cayetano Heredia; 2010. [ Links ]
14. Paredes-Martinez E, Diaz-Pizán M. Impacto de las condiciones orales sobre la Calidad de Vida en escolares del Distrito de San Juan de Miraflores. Lima, Perú. Rev Estomatol Herediana. 2014; 24(3):171-7. [ Links ]
15. Ingunza M, Del Castillo-López C, Evangelista-Alva A, Sánchez-Borjas P. Calidad de Vida Relacionada a la Salud Bucal en escolares de ámbito urbano-marginal. Rev Estomatol Herediana. 2015; 25(3):194-204. DOI: https://doi.org/10.20453/reh.v25i3.2622 [ Links ]
16. Reinoso N, Del Castillo C. Calidad de vida relacionada a la salud bucal en escolares de Sayausí, Cuenca Ecuador. Rev Estomatol Herediana. 2017; 27(4): 227-34. DOI: https://doi.org/10.20453/reh.v27i4.3214 [ Links ]
17. Crespo C, Dominguez C, Vallejo F, et al. Impacto de las Maloclusiones sobre la calidad de vida y necesidad de tratamiento ortodóntico en escolares de dos escuelas privadas Azogues – Ecuador. Rev Estomatol Herediana. 2017; 27(3):141-52. DOI: https://doi.org/10.20453/reh.v27i3.3198 [ Links ]
18. Tineo P. Impacto de las condiciones orales sobre la calidad de vida relacionada a la salud (CVRS) de escolares de 11 y 12 años del ámbito urbano del distrito de Abancay-Apurímac en el año 2011. Master Thesis. Lima: Facultad de Estomatología, Universidad Peruana Cayetano Heredia; 2012. [ Links ]
19. Castro R, Portela M, Leão A, Vasconcellos M. Oral health-related quality of life of 11-12 year old public school children in Rio de Janeiro. Community Dent Oral Epidemiol. 2011; 39(4): 336-44. Doi: https://doi. org/10.1111/j.1600-0528.2010.00601.x [ Links ]
20. Krisdapong S, Sheiham A, Tsakos G. Oral health related quality of life of 12-year and 15-year-old Thai children: findings from a national survey. Community Dent Oral Epidemiol. 2009; 37(6):509-17. Doi: https://doi. org/10.1111/j.1600-0528.2009.00503.x [ Links ]
21. Bianco A, Fortunato L, Nobile CG, Pavia M. Prevalence and determinants of oral impacts on daily performance: results from a survey among school children in Italy. Eur J Public Health. 2010; 20(5):595600. Doi: https://doi.org/10.1093/eurpub/ckp179 [ Links ]
22. Nurelhuda N, Mutaz A, Astrom A, Tordis U. Evaluation of oral health-related quality of life among Sudanese schoolchildren using Child-OIDP inventory. Health Qual Life Outcomes. 2010; 8:152-64. Doi:10.1186/1477-7525-8-152 [ Links ]
23. Cortés F, Rosel E, Artázcoz J, Bravo M, Tsakos G. Adaptation and validation for Spain of the child-oral impact on daily performance (C-OIDP) for use with adolescents. Med Oral Patol Oral Cir Bucal. 2010; 15(1):106-11. [ Links ]
24. Castro RA, Cortes MI, Leão AT, et al. Child-OIDP index in Brazil: Cross-cultural adaptation and validation. Health Qual Life Outcomes. 2008; 6: 68. doi:10.1186/1477-7525-6-68 [ Links ]
25. Gherunpong S, Tsakos G, Sheiham A. The prevalence and severity of oral impacts on daily performances in Thai primary school children. Health Qual Life Outcomes. 2004; 2: 57. doi: 10.1186/1477-7525-2-57 [ Links ]
26. Nucã C, Amariei C, Martoncsak E, TomiD D. Study regarding the correlation between the Child-OIDP index and the dental status in 12-year-old children from Harsova, Constanta County. Oral Health Dent Manag. 2005; 4(4):4-13. [ Links ]
27. Yusuf H, Gherunpong S, Sheiham A, Tsakos G. Validation of an English version of the Child-OIDP index, an oral health-related quality of life measure for children. Health Qual Life Outcomes. 2006; 4:38. Doi: https://doi.org/10.1186/1477-7525-4-38 [ Links ]
28. Sánchez S, Juárez T, Reyes H, Fuente J, Solórzano F, García C. Estado de la dentición y sus efectos en la capacidad de los ancianos para desempeñar sus actividades habituales. Salud Pública Mex. 2007; 49 (3):173-81. [ Links ]
29. Masalu JR, Astrom AN. Applicability of an abbreviated version of the oral impacts on daily performances (OIDP) scale for use among Tanzanian students. Community Dent Oral Epidemiol. 2003; 31:7-14. Doi: https://doi.org/10.1034/j.1600-0528.2003.00011.x [ Links ]
30. Srisilapanan P, Sheiham A. The prevalence of dental impacts on daily performances in older people in Northen Thailand. Rev Gerodontology. 2001; 18(2): 102-8. Doi: https://doi.org/10.1111/j.1741-2358.2001.00102.x [ Links ]
31. Tsakos G, Marcenes W, Sheiham A. Cross-cultural differences in oral impacts on daily performance between Greek and British older adults. Community Dent Health. 2001; 18(4): 209-13. [ Links ]
32. Alvarez J. Características del desarrollo psicológico de los adolescentes. Granada: Innovación y Experiencias Educativas; 2010. [ Links ]
33. Colegio Oficial de Psicólogos de Catalunya. Desarrollo Cognitivo: Las Teorías de Piaget y de Vygotsky. Barcelona: Colegio Oficial de Psicólogos de Catalunya, Universidad Autónoma de Barcelona; 2009. [ Links ]
Correspondence
Neli Marile Gomescuello Gomescuello.
e-mail: draneligomescuello@hotmail.com
Recibido: 22-02-2018
Aceptado: 26-06-2018














