Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista de Gastroenterología del Perú
versão impressa ISSN 1022-5129
Rev. gastroenterol. Perú vol.37 no.2 Lima abr./jun. 2017
REPORTE DE CASO
Laparoendoscopic rendez-vous: a safe alternative to the treatment of choledocholithiasis
Rendez-vous láparo-endoscópico: una alternativa segura en el tratamiento de la colecocolitiasis
Fernanda Kreve1, Jonas Takada2, Janaina Gatto1, Francisco S. Loss1, Everson L. A. Artifon2
1 Medical School Academic, Centro Universitário Fundação Assis Gurgacz. Cascavel, Brazil.
2 Depar tmentof Surgery, University of Sao Paulo. Sao Paulo, Brazil.
ABSTRACT
The choice treatment for choledocholithiasis when associated with lithiasic cholecystitis is endoscopic retrograde cholangiopancreatography (ERCP). However, in some cases this therapeutic fails, which requires an alternative method to extract the stones. The surgical approach tends to be the next step, but it is related to greater complexity of achievement and higher complications rates. In 1993, Deslandres et al. developed the combined treatment called laparoendoscopic rendez- vous, that unites in a single stage the endoscopic treatment of choledocholithiasis and laparoscopic removal of the gallbladder. We report the case of a patient diagnosed with common bile duct (CBD) stones, in which the conventional CPRE was not successful, and was taken to treatment by laparoendoscopic approach. We conclude, based on this case and on other published studies, that this therapeutic modality has advantages for being feasible, presenting low complications rate, shorter hospital stay and acceptable cost.
Keywords: Common bile duct gallstones; Laparoscopic cholecystectomy; Endoscopic retrograde cholangiopancreatography (source: MeSH NLM).
RESUMEN
El tratamiento de elección para la coledocolitiasis cuando se asocia con colecistitis litiásica es la colangiopancreatografía retrógrada endoscópica (CPRE). Sin embargo, en algunos casos ese tratamiento falla, requiriendo un método alternativo para extraer los cálculos. El abordaje quirúrgico tiende a ser el siguiente paso, pero se relaciona con una mayor complejidad de ejecución y mayores tasas de complicaciones. En 1993, Deslandres et al. desarrolló el tratamiento combinado llamado rendez-vous laparoendoscópico, que reúne en una sola etapa el tratamiento endoscópico de la coledocolitiasis y la extracción laparoscópica de la vesícula biliar. Presentamos el caso de una paciente diagnosticada con litiasis en la via biliar común, en el que la CPRE convencional no tuvo éxito, fue entonces enviada al tratamiento laparoendoscópico. Llegamos a la conclusión, basado en este caso y en otros estudios publicados, que esta modalidad terapéutica tiene ventajas por ser factible, teniendo bajos índices de complicaciones, menor estancia hospitalaria y costo aceptable.
Palabras clave: Cálculos biliares; Colecistectomía laparoscópica; Pancreatocolangiografía retrógrada endoscópica (fuente: DeCS BIREME).
INTRODUCTION
In patients who present cholelithiasis and stones in the common bile duct, endoscopic treatment using endoscopic retrograde cholangiopancreatography (ERCP) is the most performed procedure on the resolution ofcholedocholithiasis, with success rates reaching 90%. However, even in experienced hands, selective cannulation is unsuccessful in 3 to 12% of cases, which determines the need of alternative therapeutic for extracting the stones from the CBD. We report the case of a patient with calculous cholecystitis and associated choledocholithiasis, which after the failure of ERCP was endoscopically treated during the
surgery with help from the rendez-vous technique guided by laparoscopy.
CASE REPORT
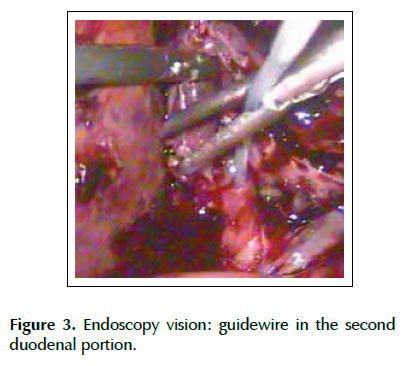
Female patient, 63, presenting calculous cholecystitis and obstructive jaundice. Laboratory tests found leukocytosis of 16,300/mm³ and increase of canalicular enzymes (Table 1). Submitted to abdominal CT scan examination, which showed biliary tract dilatation and obstruction of the distal CBD by an
8mm stone. She was initially submitted to ERCP, the papilla was found in intradiverticular position, which prevented the selective catheterization of the biliary tract. Due to the unfavorable development for acute cholangitis, it was proposed to do the laparoscopic removal of the gallbladder and endoscopic treatment of choledocholithiasis in the same step.
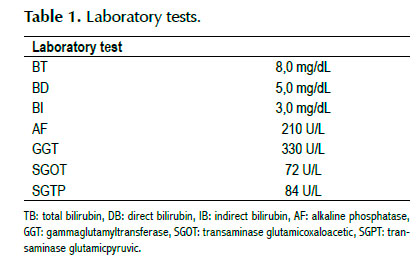
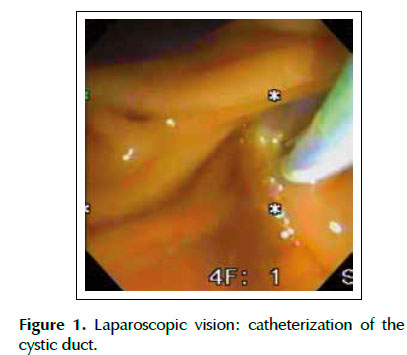
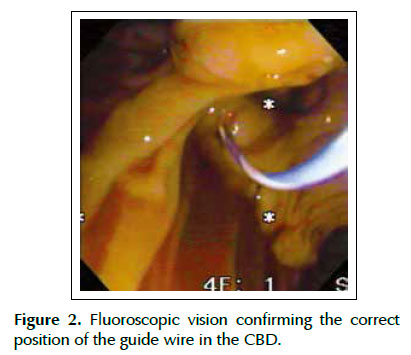
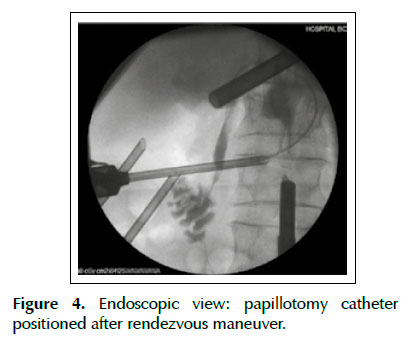
In surgery, we started with the laparoscopic dissection of the gallbladder. The Calot triangle was dissected; cystic artery was individualized, linked and sectioned. After, the cystic duct was identified and clipped proximally, we performed a distal opening that allowed its catheterization by passing a 0.035-inch guidewire (Jagwire; Boston Scientific Inc., Watertown Massachusetts, United States) attached to a catheter of cholangiography (Microknife ™ XL, Boston Scientific) (Figure 1). Under fluoroscopic vision and via transcystic, we performed the progression of the guidewire in the anterograde direction by the CBD and greater duodenal papilla to the second duodenal portion (Figure 2). A duodenoscope was introduced until the second duodenal portion, the guidewire was recovered (maneuver rendez-vous) using a polypectomy snare (Figure 3) and used to guide the retrograde cannulation of the bile duct (Figure 4). We performed endoscopic treatment of choledocholithiasis and finalized with laparoscopic gallbladder extraction.
The total surgical time was 172 minutes. We did not observe complications postoperatively. The return of peristaltic activity was evidenced on the first day after surgery. The patient was discharged from the hospital on the second day with good food acceptance. The GGT and bilirubin levels returned to normality within a week of follow-up.
DISCUSSION
Due to its effectiveness, ERCP is the most indicated treatment for patients who present with cholelithiasis and choledocholithiasis diagnosis. In such cases, this therapeutic modality enables the resolution of choledocholithiasis not only preoperatively to cholecystectomy, but also during or after gallbladder surgical removal. However, ERCP fails in 9 to 12% of cases (1). Once the duodenoscope has reached the second duodenal portion, the technical aspects that make the cannulation of the greater papilla difficult determine the failure of ERCP. Among the technical difficulties on the manipulation the biliary tract may be related: the difficulty of passing the guidewire by the stone, the "difficult cannulation", anatomical variations of the biliopancreatic confluence, intradiverticular papilla and surgical manipulations that prevent the device progression (2,3).
When endoscopic cannulation fails in the choledocholithiasis, the laparoscopic surgical exploration of the biliary tract has been the choice, considering that it presents lower complication rates compared to open surgery (4,5). Opting for laparoscopic surgery, the manipulation of the main bile duct occurs by the cystic duct or opening the CBD. The transcystic approach is safer, but restricted to small stones (usually less than 6 mm) and in favorable location to their removal. When transcystic approach is not possible, choledochotomy becomes an option (6). It is a difficult technique to execute when the main bile duct presents little dilated or compromised by intense inflammation. In addition, the exploration of the CBD requires primary suture or the placement of bile drain (aKher tube), which can increase the hospital stay and the chances of complications (e.g. stenosis and fistulas) (7).
Vecchio and MacFadyen claim that surgical exploration of the CBD requires extensive experience in advanced laparoscopic procedures. It also involves radiological and endoscopic expertise, unusual to many surgeons, which increases the surgical time and the rate of complications (8,9). Thus, owing to the technical difficulties, the long and hard learning curve and the need of technical resources (high quality fluoroscopy and choledochoscopy) not available in many operating rooms, laparoscopic exploration of the bile duct is a technique restricted to a few medical centers (10).
One has to consider also other alternatives to access the bile duct, such as transhepatic percutaneous drainage (DPTH) or endoscopy ultrasound (EUS). However, DPTH is generally used only as a temporary procedure for biliary drainage in acute cholangitis, associated with high rates of complications compared
to CPRE (11). The EUS, on the other hand, presents as an interesting tool in the realization of the rendez- vous technique, however it is associated with the need for more resources and costs that still make it a little feasible method in the current context (12).
The ERCP, in contrast, is a therapeutic modality that is easy to perform and widely available in hospitals. Combined to laparoscopic biliary tract exploration, it has the advantage of being a technique that can be applied independent of the diameter of the biliary tract, size or number of stones (13). Initially, it was proposed to be performed as in the conventional retrograde way, with the patient still anesthetized in order to decrease the hospital stay by allowing both endoscopic and surgical treatment in a single stage. However, this conduct did not lead to a reduction of the complications inherent to the manipulation of the biliary-pancreatic via (14-17).
In 1993, Deslandres et al. developed the combined treatment laparoendoscopic. The described treatment, performed during the laparoscopic cholecystectomy, consists in the intra-operative realization of ERCP after anterograde insertion (transcystic) of a guide wire to reach the major duodenal papilla and make its cannulation guided, easier and safer, allowing the removal of common bile duct stones by a balloon catheter or basket (18,19). In a period from 2005 to 2008, Ghazal et al. conducted a study in 45 patients
with evidence or suspicion of choledocholithiasis, which were submitted to treatment in a single stage –the laparoendoscopic rendez-vous. The study had favorable results. The guidewire passage through the papilla failed in only three patients and there were no postoperative complications related to the procedure like pancreatitis, bleeding and perforation. The patients were discharged after an average of 2 to 5 days, with no clinical and radiological evidence of retained stones in the bile duct (6).
The main advantage of the intraoperative ERCP using the rendez-vous technique is the selective access to the bile duct, preventing excessive manipulation of the duodenal papilla and unintentional cannulation of the pancreatic duct. Consequently, it results in lower chances of pancreatitis when compared to conventional ERCP. Furthermore, there is a reduction of surgical time through the anatomical passage of the guidewire by transcystic access, shorter hospital stays and lower costs (15,20). It may also be an alternative as a rescue therapy during surgery when the bile duct is not properly cleaned, and offers the possibility of saving when the preoperative ERCP fails, attempting to avoid surgical exploration (21,22).
Itislikelythatthemainobstacleofthelaparoendoscopic rendez-vous technique is the need to coordinate and synchronize the surgical and endoscopic teams, which should work together. Therefore, the endoscopic team must be familiar beforehand with the patient’s surgery programme and be ready to go into theatre as soon as the guidewire reaches the duodenum (20). Williams and Vellacot (23) affirm that in an ideal scenario, it would be more advantageous thatthe surgeon itself was able to perform ERCP. Otherwise, it would be necessary a longer time related to the logistical organization of the procedure, as reported in previous studies (24).
Although some studies (23,24) suggest some difficulty in visualizing the gallbladder after ERCP due to the gaseous distension of the proximal viscera, this did not prevent the appropriate surgical approach to the patient in this study. We started the cholecystectomy before ERCP and removed all the air from the gastric cavity after the endoscopic treatment, in order to facilitate the end of the cholecystectomy. Still, we believe the longer operative time in this case was primarily because of the intense inflammatory process associated with the gallbladder. Surely, the time spent with logistics factors such as handling of the fluoroscopy device and performing the intraoperative ERCP can be decreased with the improvement of the technique and the medical team organization.
In conclusion, a good management of the common bile duct stones depends on the technical skills of the medical team involved. Therefore, there is no doubt that the treatment in a single stage has advantages over the method in two stages. By decreasing the time of cannulation, the complications associated with endoscopic manipulation of the duodenal papilla, the hospital stays and the costs, laparoendoscopic rendez- vous is a safe and effective technique for the treatment of choledocholithiasis. It is an alternative for surgeons, especially those who do not often perform the surgical exploration of the common bile duct.
Conflicts of Interest: None.
BIBLIOGRAPHIC REFERENCES
1. Kumar S, Sherman S, Hawes RH, Lehman GA. Success and yield of second attempt ERCP. Gastrointest Endosc. 1995;41(5):445-7. [ Links ]
2. Martin DF. Combined percutaneous and endoscopic procedures for bile duct obstruction. Gut. 1994;35(8):1011-2. [ Links ]
3. Lobo DN, Balfour TW, Iftikhar SY. Periampullary diverticula: consequences of failed ERCP. Ann R Coll Surg Engl. 1998;80(5):326-31. [ Links ]
4. Grubnik VV1, Tkachenko AI, Ilyashenko VV, Vorotyntseva KO. Laparoscopic common bile duct exploration versus open surgery: comparative prospective randomized trial. Surg Endosc. 2012;(8):2165-71. [ Links ]
5. Ponsky JL, Heniford BT, Gersin K. Choledocholithiasis: evolving intraoperative strategies. Am Surg. 2000;66(3):262-8. [ Links ]
6. Nathanson LK, O’Rourke NA, Martin IJ, Fielding GA, Cowen AE, Roberts RK, et al. Postoperative ERCP versus laparoscopic choledochotomy for clearance of selected bile duct calculi: a randomized trial. Ann Surg. 2005;242(2):188-92.
7. Rábago LR, Ortega A, Chico I, Collado D, Olivares A, Castro JL, et al. Intraoperative ERCP: What role does it have in the era of laparoscopic cholecystectomy? World J Gastrointest Endosc. 2011;3(12):248-55. [ Links ]
8. Ghazal AH, Sorour MA, El-Riwini M, El-Bahrawy H. Single- step treatment of gall bladder and bile duct stones: a combined endoscopic-laparoscopic technique. Int J Surg. 2009;7(4):338-46. [ Links ]
9. Tinoco R, Tinoco A, El-Kadre L, Peres L, Sueth D. Laparoscopic common bile duct exploration. Ann Surg. 2008;247(4):674-9. [ Links ]
10. Flowers JL. ERCP versus laparoscopic surgery: the contest over common bile duct stones. Endoscopy. 1996;28(5):438-40. [ Links ]
11. Banerjee B, Harshfield DL, Teplick SK. Percutaneous transcholecystic approach to the rendezvous procedure when transhepatic access fails. J Vasc Interv Radiol. 1994;5(6):895-8. [ Links ]
12. Tsuchiya T, Itoi T, Sofuni A, Tonozuka R, Mukai S. Endoscopic ultrasonography-guided rendezvous technique. Dig Endosc. 2016;28 Suppl 1:96-101. [ Links ]
13. Sherman S, Hawes RH, Rathgaber SW, Uzer MF, Smith MT, Khusro QE, et al. Post-ERCP pancreatitis: randomized, prospective study comparing a low- and high-osmolality contrast agent. Gastrointest Endosc. 1994;40(4):422-7. [ Links ]
14. Siddiqui MN, Hamid S, Khan H, Ahmed M. Per-operative endoscopic retrograde cholangio-pancreatography for common bile duct stones. Gastrointest Endosc. 1994;40(3):348-50. [ Links ]
15. Cox MR, Wilson TG, Toouli J. Peroperative endoscopic sphincterotomy during laparoscopic cholecystectomy for choledocholithiasis. Br J Surg. 1995;82(2):257-9. [ Links ]
16. Meyer C, Le JV, Rohr S, Duclos B, Reimund JM, Baumann R. Management of common bile duct stones in a single operation combining laparoscopic cholecystectomy and peroperative endoscopic sphincterotomy. J Hepatobiliary Pancreat Surg. 2002;9(2):196-200. [ Links ]
17. Cemachovic I, Letard JC, Begin GF, Rousseau D, Nivet JM. Intraoperative endoscopic sphincterotomy is a reasonable option for complete single-stage minimally invasive biliary stones treatment: short-term experience with 57 patients. Endoscopy. 2000;32(12):956-62. [ Links ]
18. Deslandres E, Gagner M, Pomp A, Rheault M, Leduc R, Clermont R, et al. Intraoperative endoscopic sphincterotomy for common bile duct stones during laparoscopic cholecystectomy. Gastrointest Endosc. 1993;39(1):54-8. [ Links ]
19. LaGrecca G, Barbagallo F, Di Blasi M, Chisari A, Lombardo R, Bonaccorso R, et al. Laparo-endoscopic ‘‘Rendezvous’’ to treat cholecysto-choledocholithiasis: Effective, safe and simplifies the endoscopist’s work. World J Gastroenterol. 2008;14(18):2844-50.
20. Rábago LR, Vicente C, Soler F, Delgado M, Moral I, Guerra I, et al. Two-stage treatment with preoperative endoscopic retrograde cholangiopancreatography (ERCP) compared with single-stage treatment with intraoperative ERCP for patients with symptomatic cholelithiasis with possible choledocholithiasis. Endoscopy. 2006;38(8):779-86. [ Links ]
21. Tzovaras G, Baloyiannis I, Kapsoritakis A, Psychos A, Paroutoglou G, Potamianos S. Laparoendoscopic rendezvous: an effective alternative to a failed preoperative ERCP in patients with cholecystocholedocholithiasis. Surg Endosc. 2010;24(10):2603-6. [ Links ]
22. Enochsson L, Lindberg B, Swahn F, Arnelo U. Intraoperative endoscopic retrogradecholangiopancreatography (ERCP) to remove common bile duct stonesduring routine laparoscopic cholecystectomy does not prolong hospitalization:a 2-year experience. Surg Endosc. 2004;18(3):367-71. [ Links ]
23. Williams GL, Vellacot KD. Selective operative cholangiography and perioperativeendoscopic retrograde cholangiopancreatography (ERCP) during laproscopiccholecystectomy. A viable option for choledocholithiasis. Surg Endosc. 2002;16(39:465-7. [ Links ]
24. Montori A, Miscusi G, Masoni L, Gasparrini M, Pietropaolo V, Montori J, et al. Endoscopic and surgical integration in the approach to biliary tract disease. J Clin Gastroenterol 1999;28(3):198-201. [ Links ]
Correspondence:
Everson L. A. Artifon
Rua Guimaraes Passos, 260/apto 121 Sao Paulo. ZC: 04107-030; Brazil
E-mail: eartifon@hotmail.com
Recibido 14-8-2016
Aprobado: 11-11-2016