Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Peruana de Ginecología y Obstetricia
versão On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.4 Lima out./dez. 2021
http://dx.doi.org/10.31403/rpgo.v67i2372
Case Report
Vaginal rupture and evisceration related to contact ulcer due to prolapsed uterus: case report
31. Hospital Nacional Arzobispo Loayza, Lima, Perú
42. Hospital Nacional Edgardo Rebagliatti Martins, Essalud, Lima, Perú
Vaginal evisceration occurs in 0.36% to 0.96% of postoperative hysterectomy patients. The most frequent cause is vaginal vault dehiscence, with a higher risk in laparoscopic hysterectomy than in open approach. We describe the case of a 63-yearold woman with a history of total prolapse of the uterus, with no surgical history, who was admitted to the emergency room for vaginal evisceration. The rupture occurred in the posterior vaginal wall, where a friction ulcer had formed. Laparotomy was performed to reduce the bowel and repair the tear in the vaginal wall. Correction of the prolapse was done eight months later with satisfactory results. The type of reparative surgery depends on the type and viability of the herniated viscus and can be performed vaginally, abdominal or combined, by laparotomy or laparoscopy.
Key words: Pelvic evisceration; Pelvic organ prolapse; Operative wound dehiscence
Introduction
Vaginal evisceration is a surgical emergency that requires prompt recognition, evaluation and management to avoid major injuries to the prolapsed viscera.
The first publication was made by McGregor1, in 1907, when he described the case of a 63-year-old woman, with no surgical history, who presented evisceration of intestinal loops through the vagina after a fall. More than one hundred articles have been published on this subject, most of them referring to the presentation of individual cases or case series (≥3 patients). Some describe the incidence and characteristics of post-hysterectomy evisceration2-5. This emergency usually occurs secondary to hysterectomy, being rare without surgical history.
Dehiscence of the vaginal vault or cuff is associated with total or partial evisceration, which can be complicated by acute mesenteric ischemia and end in intestinal resection5.
The risk factors are fundamentally related to the menopausal state. In premenopausal women it is caused by trauma during intercourse, rape and introduction of foreign bodies. In postmenopausal women, it is linked to previous vaginal surgery or hysterectomy, in 65 to 75% of cases4,6,7. Other associated factors are poor healing of the vaginal vault (due to technical difficulty, malignancy, chronic steroid use, malnutrition and tissue radiation), Valsalva effort due to chronic cough or constipation, and postoperative infection or hematoma of the vaginal vault. Still, many women do not have an identifiable precipitating event. The ileum is the most frequently prolapsed viscus, although outpouching of the appendix, omentum or uterine tube has also been described8.
Evisceration without surgical history generally occurs in postmenopausal women with genital atrophy and enterocele. Vaginal ulceration due to severe atrophy and straining during defecation are commonly reported as associated factors9.
The clinical presentation preceding vaginal evisceration is characterized by abdominal pain and pressure, vaginal bleeding in most cases, and watery discharge2,3.
We present a clinical case of vaginal bowel loop evisceration in a patient with a history of prolapsed uterus and vaginal ulcer, which was resolved in two moments. A review of the subject is presented in order to propose an adequate management of this surgical emergency.
Case report
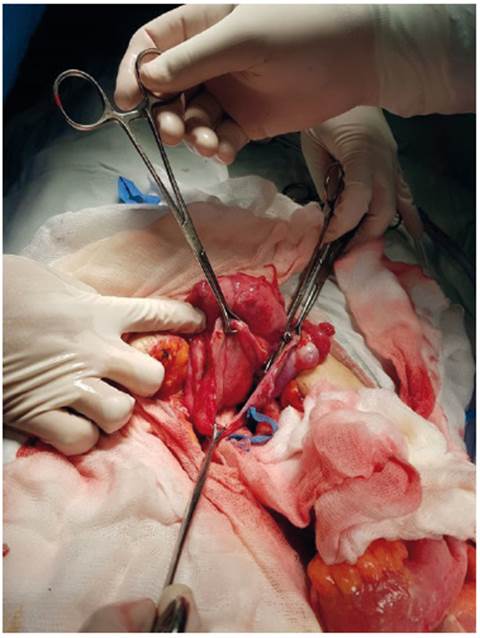
We present the case of a 63-year-old woman who came to the emergency room with protrusion of abdominal viscera through the vagina, stating that 12 hours before, while doing housework, she presented intense colicky abdominal pain that forced her to rest immediately. At the same time, she observed intestinal loops coming out of her genitals. She was evacuated to a primary care facility, where they reduced the prolapsed viscera, placed a vaginal plug and referred her to the hospital. On admission, the abdomen was found to be soft, depressible, with slight pain on deep palpation in the hypogastrium. Inspection of the genitalia revealed small bowel outside the vaginal introitus (Figure 1), apparently without areas of ischemia. She was irrigated with sterile water, the evisceration was reduced, a support plug was placed and she was prepared for surgery.
This patient had been diagnosed with grade III genital prolapse and posterior vaginal ulcer three months earlier; she was prescribed topical estriol.
As gynecological and obstetric history, she reported four vaginal deliveries, one cesarean section and one abortion; she had only one sexual partner and had denied sexual intercourse for four years. Surgical history was a laparotomy for peritonitis at age 23, inguinal hernioplasty at age 24, cesarean section with tubal ligation at age 38 and cholecystectomy at age 53.
Blood tests and tumor markers were normal, CT scan was reported without major alterations.
At laparotomy, total evaluation of the intestines was performed to confirm their viability and to rule out areas of ischemia. In the fundus of the pouch of Douglas, a solution of continuity was observed in a transverse direction of approximately 15 cm, which communicated with the vagina. The edges were edematous and the wall presented whitish thickened non-bleeding areas (Figure 2). Because of these characteristics, the edges of this opening were trimmed with a margin of 2 cm, and the specimen was sent for pathologic study. The lesion was sutured in two planes, the first with imbricated stitches using vicril 1 and the second plane in continuous Lembert suture with vicril 0.
The pathology service reported that the trimmed tissue submitted consisted of extensive erosion, fibrosis, granulation tissue, ulceration, dense inflammatory infiltrate and presence of some foci of granulation with foreign body-like giant cells.
Evaluated 15 days after surgery, total genital prolapse was observed with an ulcerated area of 5 x 4 cm in the posterior vaginal mucosa (Figure 3). The operative wound where the evisceration occurred, located in the posterior area of the ulcer, was found to be adequately healed.
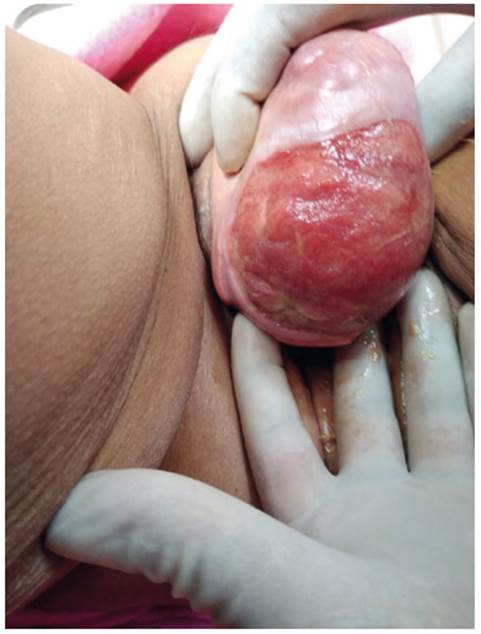
Figure 3 Ulcer in the posterior wall of the vagina one month after evisceration, note the operative scar in the posterior area of the ulcer.
Attempts were made to reduce the vaginal ulcer with topical estriol and hydrogen peroxide, without favorable results. At eight months the prolapse was surgically cured by means of vaginal hysterectomy, bilateral salpingo-oophorectomy, posterior Mc Call culdoplasty and anterior and posterior colpoperineoplasty (Figure 4). Postoperative evolution was favorable.
At the six-month follow-up, a 4 cm genital hiatus was observed and the vaginal vault was 8 cm from the introitus. The patient did not report any discomfort.
Discussion
The most frequent cause of vaginal evisceration is vaginal vault dehiscence after hysterectomy. Sexual intercourse before healing of the vaginal vault is the most important factor in young hysterectomized patients.
Fuchs10 found 23 eviscerations (0.96 %) in 2,382 total hysterectomies. Ceccaroni's study11 with 8,635 hysterectomized patients found an evisceration rate of 0.39% (34 patients)7. Uccella5, in a series of 12,398 hysterectomies, there was dome dehiscence in 0.64% of 3,573 laparoscopic hysterectomies, 0.2% in 4,291 abdominal hysterectomies and 0.13% in 4,534 vaginal hysterectomies. Ala Nissila12 described 22 cases of dehiscence in 13,645 hysterectomies (0.16%); evisceration occurred in 1.27% of total laparoscopic hysterectomies, in 0.11% of conventional laparoscopic hysterectomies (with vaginal dome closure), in 0.05% of vaginal hysterectomies and in 0.02% of abdominal hysterectomies.
Some attribute the high incidence of evisceration in total laparoscopic surgery to the use of electrosurgery, but most consider that it is due to the vaginal vault closure technique13.
Fuchs10 concludes that continuous dome suturing may be superior to interrupted suturing in preventing eviscerations.
The mean time for dehiscence of the dome is seven weeks in laparoscopic hysterectomy and 13 weeks in abdominal hysterectomy3. Baines14 publishes a case of evisceration that occurred 17 years after a total abdominal hysterectomy.
Canturk15 describes the case of a 63-year-old woman with vaginal evisceration after robotic hysterectomy to treat cervical cancer. The repair was also performed by robotic approach, with intraoperative fluorescence imaging for evaluation of intestinal perfusion.
The clinical case presented is a spontaneous vaginal evisceration that presented as risk factors a total genital prolapse with a wide, intractable vaginal ulcer caused by underwear rubbing. Few cases of evisceration are reported due to thinning of the vaginal wall in the ulcerated area16.
There are similar publications, such as that of Schreiner17, who describes a 40-year-old woman with lupus erythematosus who used glucocorticoids, with total uterine prolapse and a large vaginal ulcer through which rupture and subsequent evisceration of intestinal loops occurred. Surgical intervention confirmed intestinal viability. Vaginal hysterectomy and sacrospinous fixation of the dome were performed. Shehata16 describes a 66-year-old woman with a history of bowel cancer and irradiation, who presented with occult vaginal evisceration. Siddiqui18, in 2011, published a case of spontaneous vaginal evisceration in a woman suffering from a multi year pessary-controlled prolapse, which shifted two weeks before evisceration.
Vaginal evisceration is a surgical emergency. The technique depends on the type and viability of the herniated viscera and can be performed by laparotomy or laparoscopy, by vaginal, abdominal or combined route. The intervention consists of reducing the eviscerated abdominal contents, assessing its viability and performing segmental resection in case of vascular compromise. Subsequently, the vaginal defect is repaired with stitches of non-absorbable material3,8.
The abdominal approach is the best option when there is trauma or intestinal ischemia7. Vaginal treatment is recommended in cases of evisceration due to dehiscence of the dome when the integrity of the prolapsed viscera is confirmed and the possibility of intestinal resection is excluded19.
The decision to repair the pelvic floor dysfunction in the same surgical act or at a later time depends on the quality and viability of the tissues. In evisceration due to dehiscence of the vaginal vault, it is recommended to correct the prolapse in the same operative act; if the vaginal and supporting tissues are deteriorated, as in the clinical case presented, it is suggested to improve the conditions and treat the prolapse in a second surgical intervention.
In conclusion, it is necessary to evaluate the vaginal mucosa in prolapses, to detect ulcers that thin the vaginal wall. In all hysterectomies it is important to correctly close the vaginal vault to avoid the possibility of dehiscence and consequent evisceration.
REFERENCES
1. McGregor AN. Rupture of the vaginal wall with protrusion of small intestine in a woman 63 years of age; replacement, suture, recovery. BJOG. 1907;11(3):252-8. https://doi.org/10.1111/j.1471-0528.1907.tb11738.x [ Links ]
2. Croak AJ, Gebhart JB, Klingele CJ, Schroeder G, Lee RA, Podratz KC. Characteristics of patients with vaginal rupture and evisceration. Obstet Gynecol. 2004;103(3):572-6. DOI: 10.1097/01.aog.0000115507.26155.45 [ Links ]
3. Cronin B, Sung VW, Matteson KA. Vaginal cuff dehiscence: risk factors and management. AJOG. 2012;206(4):284-8. DOI: 10.1016/j.ajog.2011.08.026 [ Links ]
4. Kowalski LD, Seski JC, Timmins PF, Kanbour AI, Kunschner AJ, Kanbour-Shakir A. Vaginal evisceration: presentation and management in postmenopausal women. J Am Coll Surg. 1996;183(3):225-9. PMID: 8784315 [ Links ]
5. Uccella S, Ceccaroni M, Cromi A, Malzoni M, Berretta R, De Iaco P, et al. Vaginal cuff dehiscence in a series of 12,398 hysterectomies: effect of different types of colpotomy and vaginal closure. Obstet Gynecol. 2012;120(3):516-23. DOI: 10.1097/AOG.0b013e318264f848 [ Links ]
6. Cruickshank L, Amin A, DeSilva A. Small bowel evisceration: a late complication following vaginal hysterectomy. J Obstet Gynaecol. 2018;38(5):733. doi: 10.1080/01443615.2018.1444397 [ Links ]
7. Quiroz-Guadarrama CD, Martinez-Ordaz JL, Rojano-Rodriguez ME, Beristain-Hernandez JL, Moreno-Portillo M. [Vaginal evisceration. Report of a case and a literature review]. Ginecol obstet Mexico. 2013;81(6):349-52. [ Links ]
8. Alvite Canosa M, Rivas Duro J, Fandino Garcia D, Alvarez Gutierrez A, Monjero Ares I, Perez Moreiras I, et al. Spontaneous vaginal evisceration. Rev espanola enf digestivas. 2011;103(3):162-3. DOI: 10.4321/S1130-01082011000300015 [ Links ]
9. Moen MD, Desai M, Sulkowski R. Vaginal evisceration managed by transvaginal bowel resection and vaginal repair. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(3):218-20. doi: 10.1007/s00192-003-1056-1 [ Links ]
10. Fuchs Weizman N, Einarsson JI, Wang KC, Vitonis AF, Cohen SL. Vaginal cuff dehiscence: risk factors and associated morbidities. J Soc Laparoendoscop Surgeons. 2015;19(2). doi: 10.4293/JSLS.2013.00351 [ Links ]
11. Ceccaroni M, Berretta R, Malzoni M, Scioscia M, Roviglione G, Spagnolo E, et al. Vaginal cuff dehiscence after hysterectomy: a multicenter retrospective study. Eur J Obstet Gynecol Reprod Biol. 2011;158(2):308-13. doi: 10.1016/j.ejogrb.2011.05.013 [ Links ]
12. Ala-Nissila S, Laurikainen E, Makinen J, Jokimaa V. Vaginal cuff dehiscence is observed in a higher rate after total laparoscopic hysterectomy compared with other types of hysterectomy. Acta Obstet Gynecol Scand. 2019;98(1):44-50. DOI: 10.1111/aogs.13459 [ Links ]
13. Fanning J, Kesterson J, Davies M, Green J, Penezic L, Vargas R, et al. Effects of electrosurgery and vaginal closure technique on postoperative vaginal cuff dehiscence. J Soc Laparoendoscop Surgeons. 2013;17(3):414-7. doi: 10.4293/10860813X13693422518515 [ Links ]
14. Baines G, Jackson SR, Price N. Laparoscopic management of spontaneous vaginal vault dehiscence and bowel evisceration 17 years following total abdominal hysterectomy. Gynecol Surg. 2017;14(1):1. Doi: 10.1186/s10397-017-1004-6 [ Links ]
15. Canturk M, Ozben V, Kose MF, Baca B. Robotic repair of vaginal evisceration after hysterectomy and the role of intraoperative near-infrared fluorescence imaging. J Robotic Surg. 2017;11(3):383-6. doi: 10.1007/s11701-017-0688-y [ Links ]
16. Shehata F, Bougie O, Baker K, Khalil H. Occult vaginal evisceration: case report. J Obstet Gynaecol Canada. 2019. DOI: 10.1016/j.jogc.2018.11.025 [ Links ]
17. Schreiner L, Santos TG, Nygaard CC, Oliveira DS. Vaginal evisceration related to genital prolapse in premenopausal woman. Internat Braz J Urol. 2017;43(4):766-9. https://doi. org/10.1590/s1677-5538.ibju.2016.0249 [ Links ]
18. Siddiqui I, Samee A, Hall C, Cooper J, O'Mahony F. Spontaneous vaginal evisceration. BMJ case reports. 2011;2011. http://dx.doi.org/10.1136/bcr.10.2010.3410 [ Links ]
19. Bleull S, Smith H, Shapiro R. Transvaginal management of vaginal cuff dehiscence with bowel evisceration following delayed diagnosis. Case reports. Obstet Gynecol.. 2017;2017:4985382. Doi: 10.1155/2017/4985382 [ Links ]
Received: March 18, 2021; Accepted: June 11, 2021











 texto em
texto em