Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista de la Facultad de Medicina Humana
versão impressa ISSN 1814-5469versão On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.22 no.3 Lima jul./set. 2022 Epub 09-Jul-2022
http://dx.doi.org/10.25176/rfmh.v22i3.3179
Original Article
Validation of the patient health questionnaire-9 (PHQ-9) in human medicine interns at a university of reference in Peru during the COVID-19 pandemic
1Facultad de medicina Humana de la Universidad Privada San Juan bautista, Filial Chorrillos, Perú
2Facultad de medicina Humana de la Universidad Privada San Juan bautista, Filial Chincha, Perú
3Facultad de Medicina Humana de la Universidad Ricardo Palma, Lima, Perú
4Facultad de Medicina Humana de la Universidad Científica del Sur, Lima, Perú.
Introduction:
Major depression currently generates a high burden of disease in the general population, which is usually higher in medical students. The Patient Health Questionnaire-9 (PHQ-9) is a widely used instrument in the general population to assess the severity of depression in primary care.
Objective:
To validate the factorial structure of the PHQ-9 questionnaire in human medicine interns at a reference university in Peru.
Methods:
An observational, cross-sectional, and instrumental design was used. We worked with a sample of 343 human medicine interns. From the responses to the questionnaire, Cronbach's alpha coefficient was calculated, as well as the factorial analysis to determine the construct validity of this instrument in the target population.
Results:
Cronbach's alpha coefficient was 88.2%, and the item/test correlation coefficients presented values higher than 0.5. A value greater than 0.05 was obtained for the chi2 goodness-of-fit test for the model, as well as results greater than 0.9 for the model's goodness-of-fit coefficients.
Conclusion:
The factorial structure of the PHQ-9 has adequate validity and reliability in the population of human medicine interns.
Keywords: Validation Study; Medicine students; Depression; Factor Analysis . (fuente: MeSH NLM).
INTRODUCTION
Depressive disorders are among the most frequent mental disorders in the general population, and their impact extends to various areas such as personal, social, and occupational1,2. In addition, depression is among the main causes of the global disease burden, and its prevalence continues to increase1,3. In 2018, depression became the biggest contributor to disability worldwide, accounting for 7.5% of all years lived with disability1. In Peru, neuropsychiatric disorders represent the leading cause of health burden. Within them, depression generates the highest disease burden with an estimated 224,535 disability-adjusted life years, a prevalence of 6.4%, and greater affectation on women than men4,5. It has been reported that the prevalence of depression in certain population groups, such as medical students, can be significantly higher than in the general population2,6, reaching prevalences between 2.2 and 5.2 times higher than for peers from the same population and age of the general population7. A meta-analysis that included studies from 47 countries found a prevalence of depression of 22.7% and suicidal ideation of 11.1% in medical students, which exceed those estimated in the general population7. Likewise, other studies reveal that academic performance is an important factor related to depression (2.8), where it is estimated that the relationship can be bidirectional, causing a vicious circle. The different scales designed to assess depression include those conducted by doctors and those self-reported. Among these, the Patient Health Questionnaire-9 (PHQ-9) stands out, an instrument consisting of nine items designed to assess and monitor the severity of depression, self-administered in primary care and other settings9. The items included a focus on the diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders in its fourth edition (DSM-IV), although in its latest version (DSM-5), the depressive disorders working group considered including the PHQ-9 as a measure of severity for the diagnosis of major depression9. Although the PHQ-9 is based on the information reported by the subject, the tool has shown good sensitivity and specificity in various studies, taking a score of 10 as a cut-off point when compared with the diagnosis made by the patient-trained professionals using reference methods2,10,11. These characteristics make the PHQ-9 a very useful instrument in medical education scenarios since it is quick to apply and provides good reliability results. In support of this last point, a recent study on medical students from Peru, in a pre-pandemic context, reported adequate internal consistency (Cronbach's alpha = 0.903) and adequate psychometric properties to be applied to medical students12. However, to date, there are no national validation studies of this scale in medical interns in the context of the COVID-19 pandemic. Therefore, this study aims to validate the factorial structure of the PHQ-9 questionnaire in human medicine interns at a reference university in Peru in the context of the COVID-19 pandemic.
METHODS
Study design and area
An observational, descriptive, cross-sectional, instrumental-type study was conducted at a private university in the city of Lima, Peru13.
Population and sample
The population consisted of 343 students from the Universidad Privada San Juan Bautista attending a medical internship during the year 2021. As selection criteria, students who had completed the questionnaire and duly signed the informed consent were included students who are doing some university exchange rotation and who have withdrawn from the academic semester.
343 medical interns were included in the study, taking into consideration the optimal sample size to perform a factorial analysis, which is recommended to be greater than 20014; a simple random sampling was carried out, without replacement, using the epidemiological package of free access Epidat version 4.2.
Variables and instruments
The Patient Health Questionnaire (PHQ-9) scale consists of 9 items according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria, which are directly related to depressive symptoms in the last 2 weeks before self-assessment. Each item is scored on a Likert scale ranging from 0-3 for none and almost every day, respectively. According to the score obtained (0-27 points), 5 degrees of severity of the depressive disorder are reflected. These grades are none (0-4), mild (5-9), moderate (10-14), moderately severe (15-19), and severe (20-27).26,27.
Procedures
A virtual questionnaire was used through the Google Forms application, self-administered by the study subject, through the WhatsApp social network. The data collected were transferred to the statistical package SPSS version 26, where the statistical tests were performed.
Statistical analysis
The mean and standard deviation of the quantitative variables and the relative and absolute frequency of the qualitative variables of the target population were reported. Univariate descriptive statistics for each item, mean and standard deviation, as well as the item-test correlation, were evaluated, taking a Rho coefficient ≥ 0.3 as an acceptable value.
Cronbach's Alpha coefficient was used as an estimator of internal consistency to determine the reliability of the model,
To validate the hypothesized one-dimensional model, a confirmatory factor analysis was used, determining the goodness of fit by reporting the P-value of the chi-square statistical test of goodness of fit, with values greater than 0.05 indicating a good fit of the model, the ratio of the chi square statistic and its degrees of freedom (CMIN/DF) with values < 3 indicating an acceptable fit and < 5 a reasonable fit, as well as the Goodness of Fit Indices (GFI), Tucker Lewis (TLI) and comparative fit (CFI) where values > 0.9 indicate a good fit of the model; the mean square error of approximation (RMSEA) was calculated considering values less than 0.01, 0.05 and 0.08 as excellent, good and mediocre fit respectively, their respective confidence intervals at 90% and P-value, where the latter, by providing a p-value >0.05, represents a good fit to the model 15,16; the square root of the squared mean of the standardized residual (SRMR) values between 0.00 and 0.08 are taken as acceptable ranges.17Finally, structural equation modeling was performed to represent the one-dimensional construct of the scale.
Ethical aspects
This article was approved by the Faculty of Medicine of the Universidad Privada San Juan Bautista and the ethics committee of the same faculty. Likewise, to comply with the statutes given in the Declaration of Helsinki, the absolute anonymity of each of the subjects who participated in the study was respected.
RESULTS
The item/test correlation coefficients presented optimal values greater than 0.5 for each of the nine items, the lowest coefficient being item number eight with 0.537 and item number seven the highest with 0.707 (Table 1).
Table 1. Correlación ítem/test.
| Ítems | Correlation item / test |
|---|---|
| Ítem 1 | 0,592 |
| Ítem 2 | 0,625 |
| Ítem 3 | 0,612 |
| Ítem 4 | 0,671 |
| Ítem 5 | 0,654 |
| Ítem 6 | 0,662 |
| Ítem 7 | 0,707 |
| Ítem 8 | 0,537 |
| Ítem 9 | 0,633 |
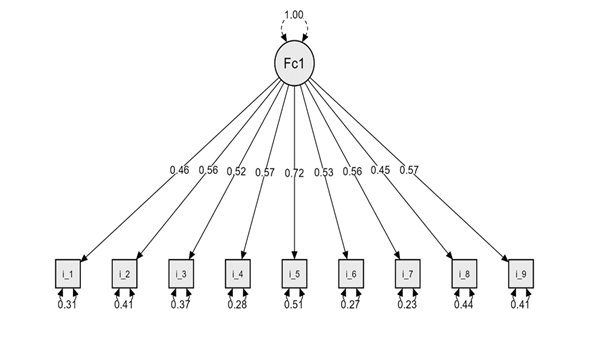
The confirmatory factor analysis was used to determine the goodness of fit of the unidimensional model in which the chi2 goodness of fit test presented a p-value greater than 0.05 and the Chi2/gl coefficient presented a value less than 5. In turn, the values for the coefficients of the goodness of fit (GFI), Tuker Lewis (TLI), and comparative fit (CFI) gave results greater than 0.9. The RMSEA showed an optimal fit for the model, presenting values lower than 0.05 and a P-value > 0.05. Likewise, the SRMR gave a value of 0.042. The results of these statistical tests are summarized inTable 2, presenting the goodness-of-fit coefficients of the two-dimensional model. In addition, one-dimensional structural modeling of the PHQ-9 scale was carried out, including each of the items and the dimension evaluated. (Figure 1)
Table 2. Pruebas y coeficientes de bondad de ajustes el modelo unidimensional de la escala PHQ-9.
| Pruebas de Ajuste | Modelo Unidimensional | Modelo bidimensional |
| P-valor Chi2 | <0,001 | <0,001 |
| Ratio Chi2 / gl | 3,10 | 3,78 |
| RMSEA (IC-90%) | 0,078 (0,060 - 0,098) | 0,09 (0,069 - 0,113) |
| SRMR | 0,042 | 0,045 |
| GFI | 0,948 | 0,947 |
| TLI | 0,939 | 0,921 |
| CFI | 0,954 | 0,947 |
| AIC | 6289,617 | 6361,104 |
DISCUSSION
This study sought to validate the factorial structure of the Patient Health Questionnaire-9 (PHQ-9) in human medicine interns at a reference university in Peru. The results determined a good fit for the one-dimensional model, whose coefficients of the goodness of fit as the AIC, showed a value of 6289.617. In addition to this, through Cronbach's alpha coefficient, a value of 0.882 was obtained for internal consistency, reflecting a consistent estimate. On the other hand, the GFI, TLI, and CFI obtained values of 0.948, 0.939, and 0.954, respectively. This last value indicates that the model can reproduce at least 90% of the covariance in the data. Likewise, both the RMSEA and SRMR indexes yielded values of 0.078 (<0.08) and 0.042 (0<05), indicating a good fit for the model, respectively.
The value of internal consistency obtained (Cronbach's alpha: 0.882) was analogous to a study at the Latin American level in medical students from Colombia (Cronbach's alpha: 0.830), while at the international level, a study in Korea showed an alpha Cronbach's of 0.837 (18.19). On the other hand, in a sample of students not studying medicine in China and Korea, values of 0.854 and 0.83, respectively, were found20,21. Additionally, a study carried out by Arturo CM, et al22validating the PHQ-9 in adults from a primary care center reported a value for Cronbach's alpha of 0.80. However, a study carried out in Peru, applied to medical students, showed a higher value than the one reported (0.903)23. Given these data, it is important to consider that the previously mentioned studies, both nationally and internationally, did not report the value of the AIC, unlike our study (6289.617). The lower the AIC value for the instrument, it is considered the best model to choose, but a contrast with other models of 1 or more dimensions is required24.
Confirmatory factor analysis determined that the factor structure and internal consistency fit the original (one-dimensional) model of the Patient Health Questionnaire-9 (PHQ-9) in human medicine interns. These findings are similar to studies previously carried out in Asia18,20,21, while, at the Latin American level, both Peru and Colombia validated a bifactorial model19,23.
It is important to consider that this study adds to the few that exist at the national level on validating the construct in human medicine interns. Therefore, it is also necessary to consider that the instrument was designed for outpatients. After the above, there are some limitations. First, only students from a single university house were included, therefore, the data cannot be completely generalized to interns from other houses of study. Second, the nature of the study, the inmates may show varying degrees of depression or other associated pathologies depending on the previous or current situation that is happening, and there may be intervening variables not considered as the history of mental illness. Finally, there was no control group. In the future, it is recommended to carry out longitudinal cohort studies, including a multicenter sample, and carry out more validation studies due to its scarcity in this population and high prevalence25.
CONCLUSION
This study demonstrated that the PHQ-9 questionnaire has adequate validity and reliability in the population of medical students. These findings could help screen for depression in this population and thus be able to carry out interventions early to avoid consequences that limit the performance of health personnel.
REFERENCES
1. World Health Organization. Depression and Other Common Mental Disorders Global Health Estimates [Internet]. 2017. Available from: https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf [ Links ]
2. Yoon S, Lee Y, Han C, Pae C-U, Yoon H-K, Patkar AA, et al. Usefulness of the Patient Health Questionnaire-9 for Korean medical students. Academic Psychiatry: The Journal of the American Association of Directors of Psychiatric Residency Training and the Association for Academic Psychiatry [Internet]. 2014 Dec 1 [cited 2022 Jun 29];38(6):661-7. Available from: https://pubmed.ncbi.nlm.nih.gov/24804631/ DOI: 10.1007/s40596-014-0140-9 [ Links ]
3. Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet [Internet]. 2020 Oct 17;396(10258):1204-22. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30925-9/fulltext DOI: 10.1016/S0140-6736(20)30925-9 [ Links ]
4. Lineamientos de política sectorial en salud mental: Perú 2018 [Internet]. www.gob.pe. [cited 2022 Jun 29]. Available from: https://www.gob.pe/institucion/minsa/informes-publicaciones/279661-lineamientos-de-politica-sectorial-en-salud-mental-peru-2018 [ Links ]
5. Hernández-Vásquez A, Vargas-Fernández R, Bendezu-Quispe G, Grendas LN. Depression in the Peruvian population and its associated factors: analysis of a national health survey. Journal of Affective Disorders [Internet]. 2020 Aug 1 [cited 2022 Apr 23];273:291-7. Available from: https://cris.usil.edu.pe/es/publications/depression-in-the-peruvian-population-and-its-associated-factors--2 [ Links ]
6. Moir F, Yielder J, Sanson J, Chen Y. Depression in medical students: current insights. Advances in Medical Education and Practice [Internet]. 2018 May;Volume 9:323-33. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5944463/ doi: 10.2147/AMEP.S137384 [ Links ]
7. Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of Depression, Depressive Symptoms, and Suicidal Ideation Among Medical Students. JAMA [Internet]. 2016 Dec 6;316(21):2214. Available from: https://jamanetwork.com/journals/jama/fullarticle/2589340 doi: 10.1001/jama.2016.17324 [ Links ]
8. Mao Y, Zhang N, Liu J, Zhu B, He R, Wang X. A systematic review of depression and anxiety in medical students in China. BMC Medical Education. 2019 Sep 2;19(1). https://doi.org/10.1186/s12909-019-1744-2 [ Links ]
9. Spitzer RL, Williams JBW, Kroenke K, & Colleagues. Test Review: Patient Health Questionnaire-9 (PHQ-9). Rehabilitation Counseling Bulletin. 2014;57(4):246-248. doi:10.1177/0034355213515305 [ Links ]
10. Levis B, Benedetti A, Thombs BD. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ [Internet]. 2019 Apr 9;365:l1476. Available from: https://www.bmj.com/content/365/bmj.l1476 doi: https://doi.org/10.1136/bmj.l1476 [ Links ]
11. Baader M T, Molina F JL, Venezian B S, Rojas C C, Farías S R, Fierro-Freixenet C, et al. Validación y utilidad de la encuesta PHQ-9 (Patient Health Questionnaire) en el diagnóstico de depresión en pacientes usuarios de atención primaria en Chile. Revista chilena de neuro-psiquiatría [Internet]. 2012 Mar 1;50(1):10-22. Available from: https://scielo.conicyt.cl/scielo.php?script=sci_arttext&pid=S0717-92272012000100002 http://dx.doi.org/10.4067/S0717-92272012000100002 [ Links ]
12. Huarcaya-Victoria J, De-Lama-Morán R, Quiros M, Bazán J, López K, Lora D. Propiedades psicométricas del Patient Health Questionnaire (PHQ-9) en estudiantes de medicina en Lima, Perú. Revista de Neuro-Psiquiatría. 2020;83:72-8. Available from: http://www.scielo.org.pe/pdf/rnp/v83n2/0034-8597-rnp-83-02-72.pdf doi: https://doi.org/10.20453/rnp.v83i2.3749 [ Links ]
13. Carretero-Dios H, Pérez C. Normas para el desarrollo y revisión de estudios instrumentales. International Journal of Clinical and Health Psychology [Internet]. 2005 [cited 2022 Jun 29];5(3):521-51. Available from: https://www.redalyc.org/articulo.oa?id=33705307 [ Links ]
14. Kyr iazos TA. Applied Psychometrics: Sample Size and Sample Power Considerations in Factor Analysis (EFA, CFA) and SEM in General. Psychology. 2 de agosto de 2018;9(8):2207-30. doi:10.4236/psych.2018.98126. https://doi.org/10.4236/psych.2018.98126 [ Links ]
15. MacCallum R, Browne M, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1(2):130-49. doi:10.1037/1082-989X.1.2.130 https://doi.org/10.1037/1082-989X.1.2.130 [ Links ]
16. Marsh HW, Hocevar D. Application of confirmatory factor analysis to the study of self-concept: First- and higher order factor models and their invariance across groups. Psychological Bulletin. 1985;97(3):562-82. doi:10.1037/0033-2909.97.3.562https://doi.org/10.1037/0033-2909.97.3.562 [ Links ]
17. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1 de enero de 1999;6(1):1-55. doi:10.1080/10705519909540118 https://doi.org/10.1080/10705519909540118 [ Links ]
18. Yoon S, Lee Y, Han C, Pae C-U, Yoon H-K, Patkar AA, et al. Usefulness of the Patient Health Questionnaire-9 for Korean Medical Students. Acad Psychiatry [Internet]. 2014 Dec 8;38(6):661-7. Available from: http://link.springer.com/10.1007/s40596-014-0140-9 [ Links ]
19. Cassiani-Miranda CA, Vargas-Hernández MC, Pérez-Anibal E, Herazo-Bustos MI, Hernández-Carrillo M. Reliability and dimensionality of PHQ-9 in screening symptoms of depression among health science students in Cartagena, 2014. Biomédica [Internet]. 2016 Oct 31;37:112-20. Available from: http://www.revistabiomedica.org/index.php/biomedica/article/view/3221 [ Links ]
20. Kim YE, Lee B. The Psychometric Properties of the Patient Health Questionnaire-9 in a Sample of Korean University Students. Psychiatry Investigation. 2019 Dec 25;16(12):904-10. doi: 10.30773/pi.2019.0226. https://doi.org/10.1080/10705519909540118 [ Links ]
21. Zhang Y-L, Liang W, Chen Z-M, Zhang H-M, Zhang J-H, Weng X-Q, et al. Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia-Pacific Psychiatry. 2013 Oct 10;5(4):268-75. doi: 10.1111/appy.12103. https://doi.org/10.1111/appy.12103 [ Links ]
22. Cassiani-Miranda CA, Cuadros-Cruz AK, Torres-Pinzón H, Scoppetta O, Pinzón-Tarrazona JH, López-Fuentes WY, et al. Validez del Cuestionario de salud del paciente-9 (PHQ-9) para cribado de depresión en adultos usuarios de Atención Primaria en Bucaramanga, Colombia. Rev colomb psiquiatr [Internet]. 2021 [cited 2022 Jun 29];11-21. Available from: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1251627 [ Links ]
23. Huarcaya-Victoria J, De-Lama-Morán R, Quiros M, Bazán J, López K, Lora D. Propiedades psicométricas del Patient Health Questionnaire (PHQ-9) en estudiantes de medicina en Lima, Perú. Rev Neuropsiquiatr [Internet]. 2020 Jul 15;83(2):72-8. Available from: https://revistas.upch.edu.pe/index.php/RNP/article/view/3749 [ Links ]
24. DiStefano C, Hess B. Using Confirmatory Factor Analysis for Construct Validation: An Empirical Review. J Psychoeduc Assess [Internet]. 2005 Sep 18;23(3):225-41. Available from: http://journals.sagepub.com/doi/10.1177/073428290502300303 https://doi.org/10.1177/073428290502300303 [ Links ]
25. Yuan L-L, Lu L, Wang X-H, Guo X-X, Ren H, Gao Y-Q, et al. Prevalence and Predictors of Anxiety and Depressive Symptoms Among International Medical Students in China During COVID-19 Pandemic. Front Psychiatry [Internet]. 2021 Nov 4;12(November):1-11. Available from: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.761964/full DOI: 10.3389/fpsyt.2021.761964 [ Links ]
26. Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the patient health questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. Journal of General Internal Medicine [Internet]. 2006 Jun;21(6):547-52. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1924626/ doi: 10.1111/j.1525-1497.2006.00409.x [ Links ]
27. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine [Internet]. 2001 Sep;16(9):606-13. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1495268/ DOI: 10.1046/j.1525-1497.2001.016009606.x [ Links ]
8Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: April 20, 2022; Accepted: July 24, 2022











 texto em
texto em