INTRODUCTION
Acquired Immunodeficiency Syndrome (AIDS) is a disease caused by the HIV virus and is transmitted mainly through sex. By the end of 2017, approximately 1.8 million AIDS cases were registered in Latin America 1. The disease represents one of the biggest public health problems nowadays, since, in the advanced stages, the individual becomes susceptible to opportunistic infections, hepatitis, gastritis, and tuberculosis, among other manifestations. A third of HIV-infected patients could be unaware of having the infection 2.
It is estimated that approximately 60%-80% of HIV-infected individuals have oral manifestations, which may represent the first signs of infection 3. Some factors may be associated with the appearance of oral manifestations in HIV-infected patients are a T-CD4 lymphocyte count of <200 cells/mm3 and a high viral load 4 Thus, oral health is an important indicator of the general condition of HIV-infected patients 5. Based on the frequency with which they present, oral manifestations can be classified into three groups: manifestations strongly associated with HIV infection such as candidiasis, hairy leukoplakia (LP), Kaposi’s sarcoma (KS), non-Hodgkin’s lymphoma, necrotizing ulcerative gingivitis (GUN), and necrotizing ulcerative periodontitis (PUN); lesions associated with HIV such as diseases of the salivary glands, herpetic viral infections, and melanotic pigments; and lesions seen in HIV infection 6. The aim of this study was to present three clinical cases of patients who were unaware of being infected with the HIV virus and whose first manifestations of the disease were oral and whose clinical diagnosis made by the dentist was fundamental in the suspicion and subsequent diagnosis of HIV infection.
Case report
Case 1
A 42-year-old female, with no reports of systemic diseases, presented to the Oral Pathology Clinic, Faculty of Dentistry, University of Chile, with complains of extensive white plaques on the hard and soft palate and the tongue’s edge, which could be scrapped off. The medical history revealed fever, asthenia, adynamia, and vomiting since a week. Clinically, the condition was compatible with pseudomembranous candidiasis (Figure 1). She was prescribed 2% miconazole topically three times a day for 2 weeks and was asked to undergo an enzyme-linked immunoassay (ELISA) test for HIV, complete blood count, and liver and lipid profiles. The results of the exams showed the following: 1) hepatic deficiency: aspartate aminotransferase (AST): 36 U/L (ref: 10-37 U/L); 2) low leukocyte count: 2560/mm3 (reference 4000-10000/mm3); 3) high speed of globular sedimentation: 96 mm/hr (1-20 mm/hr); 4) anemia: erythrocytes: 3.81 × 10 6 µL (ref: 4-5 × 10 6 µL), hemoglobin: 10.3 g/dL (ref: 12-16 g/dL), hematocrit: 32.9% (ref: 36%-48%); and 5) renal failure: uric acid: 6.50 mg/dL (ref: 0.5-5 mg/dL), urea: 48.7 (15-36) 6) reagent for HIV. The patient was referred to the medical clinic; however, she died due to multiorgan failure 2 months after the initial dental consultation.
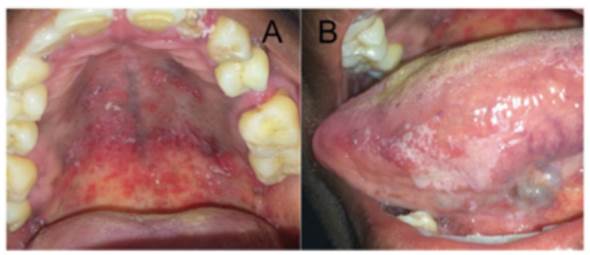
Figure 1. White plaques that could be scrapped off, associated with erythema and ulceration, distributed on the palate (A) and lateral border of the tongue (B).
Case 2
A 41-year-old male was referred to the Oral Pathology Clinic, Faculty of Dentistry, University of Chile, for the evaluation of a painless gingival lesion, which was persistent for about 15 days. Aside from the history of smoking for about 20 years and using legal drugs (alcoholic beverages) and illicit drugs (marijuana, cocaine, and ecstasy), his medical history revealed psychiatric treatment for bipolar disorder; hypovitaminosis B, D, E (justified by vegan food); and tuberculosis treatment for 3 years. On clinical examination, a 1.5-cm ulcerated lesion was found inserted in the gingiva and alveolar mucosa associated with tooth 46 and periapical; radiography of the region revealed horizontal bone loss, compatible with PUN (Figure 2). The patient was referred for periodontal therapy, whose treatment helped to treat the clinical aspect of the lesion. ELISA tests for HIV and Venereal Diseases Research Laboratory test were requested, which revealed positivity only for HIV. In light of the findings, the patient was referred for further medical treatment.
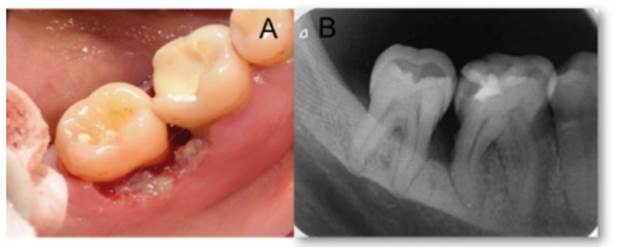
Figure 2 A: Area of ulceration and necrosis located in the gingiva and alveolar mucosa associated with tooth 46. B: Periapical radiography showing horizontal bone loss located through the mesial area of tooth 46 and the distal area of tooth 45.

Figure 3 A: Vesiculoulcerative lesions in the anterior region of the palate seen on initial consultation. B: Appearance of the palate after a week of follow-up.
Case 3
A 33-year-old male was referred to the Oral Pathology Clinic, Faculty of Dentistry, University of Chile, for the evaluation of painful vesicle-like lesions on the palate, since 2 days. On clinical examination, he had fever, asthenia, and adenopathy. Intraoral examination revealed the presence of vesicle-ulcerative lesions on the anterior third of the hard palate (Figure 4 and Figure 5). After a one-week follow-up, the lesions were resolved. The clinical picture was compatible with intraoral recurrence of herpes simplex virus 1 (HSV-1). Due to the unusual manifestations of this intraoral recurrence, an ELISA test was requested, which revealed a reagent for HIV. The patient was referred to the medical clinic.
DISCUSSION
The fact that the first manifestations of this infection or progression to AIDS can be oral highlights the importance of the dentist in detecting oral manifestations associated with HIV 6. The spectrum of oral changes related to HIV infection is wide, comprising >40 lesions 7. According to the classification of oral manifestations associated with HIV infection, oral candidiasis is one of the most prevalent infections and can affect up to 94% of infected patients 6. The literature points out that erythematous candidiasis is more associated with progression to AIDS whereas pseudomembranous candidiasis most often reflects the already established disease 3,7. In the first case presented, the intensity of the intraoral characteristics observed (extensive white plaques detachable to the scraping associated with erythema) suggested a state of immunosuppression, which was confirmed with laboratory tests and the patient’s death 2 months after the initial dental consultation. Hematological tests revealed, in fact, liver dysfunction, renal failure, and anemia 8. The reasons why patients with advanced immunosuppression have more severe candidiasis can be explained by an epithelial dysfunction in the oral mucosa produced by an increase in the HIV viral load 9, in addition to a decrease in the salivary flow, also associated with disease progression 10. It is important to note that the diagnosis of oral candidiasis is clinical and must be performed by the dentist 3.
Periodontal diseases, such as candidiasis, are classified in the group of injuries most frequently associated with HIV infection. Clinical manifestations such as linear gingival erythema, GUN, and PUN can be predictive of progression to AIDS 11. PUN represents a type of periodontal disease characterized by presenting areas of tissue necrosis, extensive or terminating, with loss of periodontal insertion, and bone sequestration, with rapid progression. Case 2 had PUN and horizontal bone loss of rapid evolution. In addition to being associated with local factors such as poor hygiene and smoking, periodontal diseases can also be linked to systemic alterations 12. The patient in this case had acceptable oral hygiene, but some systemic conditions, such as being under treatment for psychic illness (bipolarity) for 12 years. With the reported habits, such as chronic smoking in addition to the regular use of alcoholic beverages and marijuana, being decisive to understand the greater aggressiveness and speed in the progression of the periodontal clinical condition, it is observed in the literature that bipolarity is capable of generating an increase in the production of pro-inflammatory cytokines, which could lead to an increase in the chance of developing periodontal diseases 13. It has been reported that smoking alters the immune response and causes cytotoxicity in the periodontal tissues in addition to modifying the oral microbiota, facilitating the progression of tissue destruction. Smoking is able to stimulate the production of prostaglandin E2, decreasing the specific antigenic response of CD8+T lymphocytes by altering the recruitment of polymorphonuclear cells 14. P. gingivalis can induce the reactivation of HIV via chromatin modification; the bacterial metabolite butyric acid produced in anaerobic conditions is responsible for this effect. These findings suggest that periodontal diseases may act as a risk factor for the reactivation of HIV in infected individuals and may contribute to the progression of AIDS 15. The condition of Case 2 improved quickly after periodontal treatment. The use of illicit drugs highlights the need for a multidisciplinary approach to promote and guarantee the health of individuals with such profile 16.
Some reports indicate that >80% of the population is seropositive for HSV-1, which is in a state of latency in the trigeminal ganglion under immunological surveillance. The typical intraoral clinical presentation of HSV infection consists of vesicular lesions that coalesce and ulcerate on an erythematous base in keratinized mucosa. The third case presented vesicle-ulcerative lesions on the hard palate, which were compatible with an intraoral recurrence of HSV-1 and associated with intense painful symptoms. In addition, the patient reported having asthenia and adenopathy. The attenuation of the immune system in HIV-infected patients affects the immunity of the oral mucosa due to the rupture of the hermetic epithelial junctions, facilitating the spread of HSV-1 17. Recurrent intraoral HSV-1 infections can be effectively treated with systemic acyclovir (400 mg, three times a day) or systemic valacyclovir (500-1000 mg, twice a day) for 3-5 days. The dosage and duration of systemic antivirals, however, are different when administered to HIV-immunosuppressed patients 18. Even in a latent state, HSV-1 in an immunocompetent patient is not a risk factor, but its activation in an HIV-immunosuppressed patient could cause changes in the central nervous system 19. In Case 3, it was not necessary to use antivirals, since the clinical picture showed an evident improvement after one-week follow-up. It is important to note that the diagnosis of HSV-1 intraoral manifestation is exclusively clinical, and the dentist must consider its different and more severe manifestations in an immunosuppressed individual. Antiretroviral therapy (ART) helps to reduce the severity of opportunistic diseases and oral manifestations. The patients in the present study were referred for medical treatment and two of them (one died) were treated with ART, which also helps in the suppression of viral load and immunological reconstitution, in addition to increasing the life expectancy of these individuals 20.
CONCLUSION
Despite the effectiveness of current treatments and global campaigns to prevent the spread of HIV, large numbers of people still do not know they are infected. In these cases, the role of the dental surgeon is fundamental, since sometimes the first manifestations of infection and progression to the disease (AIDS) can be intraoral. Pseudomembranous candidiasis and intraoral recurrence of HSV-1 usually present a clinical diagnosis, as presented in both cases. It should also be noted that these evaluations were conducted in an emergency setting in the public service and supplementary molecular testing was not warranted. In the case of candidiasis, the lesions coincided with the clinical description of a pseudomembranous candidiasis, presenting as asymptomatic white plaques that were dislodged upon scraping. In the case of intraoral herpes, they corresponded to lesions of 2 to 3 mm oval ulcerative vesicles on keratinized mucosa and the only difference with the classic intraoral clinical presentation was that they cross the midline. To reach an adequate diagnosis, the dentist must always carry out an adequate anamnesis and clinical examination, understanding that oral lesions may be a reflection of the systemic state of the patient and not only of a local infection.














