INTRODUCTION
Numerous studies link cow’s milk protein allergy (CMPA) to further manifestations of autoimmune diseases. CMPA was found to be associated for example with inflammatory bowel disease, autoimmunity against beta cells and also rheumatic diseases 1.
In rheumatoid arthritis antibodies against dietary proteins such as cow’s milk and soya have been detected in the jejunum. Patients with juvenile idiopathic arthritis have reported improvement of arthritic symptoms when CMP was removed from the diet. This symptomatic improvement with a hypoallergenic diet also has a histological correlation: one study showed, using endoscopies, that one-third of children with JIA who had gastrointestinal symptoms were found to have eosinophilic infiltration.
Furthermore, a CMP-free diet would not only influence the evolution of symptoms but also the very genesis of the disease. There are case-control epidemiological studies that have revealed the onset of JIA is associated with the antecedent allergy to cow’s milk protein and antibiotic use in males 2.
Food hypersensitivity in patients is usually non-immunoglobulin E mediated. A European epidemiological study found a significant association between polyarthritis and red meat consumption, elevated serum levels of immunoglobulin M were found in this type of patient. The research also detected that the total level of immunoglobulin M in jejunum liquid in patients with rheumatoid arthritis had increased compared to the healthy controls, and this was evident for some titers of immunoglobulin specific to food. Both systemic and intestinal immunity was found to be aberrant in patients with rheumatoid arthritis, particularly elevated antibodies in the proximal intestinal fluid 3.
Despite the numerous cases reported which explore the association, studies that link diet and JIA are not consistent and generally conclude that the relationship between CMPA and JIA is only incidental 4.
This study shows the evolution of a case that met JIA criteria and which presented exacerbations related to diet. Remission of the disease was achieved by only adhering to a hypoallergenic diet. This supports the hypothesis that food allergy is involved, not only with the genesis but also with the evolution of food allergy cases. The fact that there are multiple, non- IgE mediated, patient specific allergies, means that obtaining complete improvement in all cases would not be possible.
CASE REPORT
A 7-year old boy with a history of repeated hives since the age of one, was admitted to the emergency room on 07/07/16 due to fever, general malaise, headache, abdominal pain on the right flank, adenopathies and facial skin lesions with a 15-day evolution. Patient´s CRP was high indicating a possible infection. He was evaluated by surgeons and a tomography was performed which showed multiple mesenteric adenopathies. Ceftriaxone was indicated. The febrile pattern was irregular during hospitalization, every other day at the beginning and daily during the last 8 days of hospitalization, reaching maximum peaks of 38.8°C, predominantly in the evening. Skin lesions subsided with antihistamine prescribed by dermatologists on 24/07/16 when maculopapular rash on the thorax and abdomen were noticed, coinciding with recorded arthritis in the left knee that day.
Furthermore, the fever study showed negative results for: blood cultures, Brucella serology, TORCHs and EBV, ANA (-); normal B2-microglobulin, echocardiography without vegetations, mild anaemia (10.1mg/dl), peripheral eosinophilia (8.5%), elevated rheumatoid factor 32.6 (VN <14 IU/ml), negative antibodies against citrullinated peptide, elevated ASO (724) and normal ferritin. Fever did not abate despite 7 days of ceftriaxone (7-13th July) and rheumatology suggested starting naproxen on 26/07/16 for possible JIA. The child left the next day having been afebrile for 24 hours, with a diagnosis of fever of unknown origin (FUO) and probable JIA. The patient received naproxen 250 mg c/12 and oral ranitidine when discharged.
The child returned to the emergency room on 28/08/16 because of recurring maculopapular rash, headache, arthralgia in hands and feet and abdominal pain. The parents said that the child had continued with the same irregular fever pattern, which did not subside, despite regular use of naproxen and metamizole. Abdominal pain was daily and predominantly in the morning, associated with constipation, early satiety and nausea. He also presented ocular erythema which occurred at the same time as the rash.
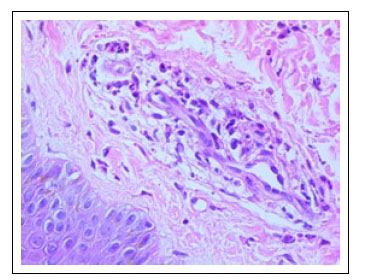
The physical examination found severe pain in the right iliac fossa and angioedema like lesions on the chest and face. Tests showed Hb 7.8 mg/dL, normal blood count and platelets 716,000, IgE 1215 IU/ml (VN<52 IU/ml), IgA 454 mg/dL (VN<231). Due to fever, thrombocytosis and anaemia, bone marrow aspiration was performed to rule out lymphoproliferative diseases and myeloculture. He was evaluated by ophthalmology which established active uveitis. A skin biopsy of the active lesions was carried out and this showed acute vasculitis of the small blood vessels, and negative IgA immunofluorescence and C3c (Figure 1).
Due to the persistence of abdominal pain, an upper and lower endoscopy was done on 05/09/16 which found nodular ileocolitis. The biopsies showed: transverse colon with acute and chronic inflammation, congestion and the presence of lymphoid follicles (Figure 2); ileum with moderate acute and chronic inflammation, flattening of villi, presence of lymphoid follicles-up to 6 eosinophils/hpf (Figure 3); rectum with acute and mild chronic inflammation, congestion and presence of lymphoid follicles with up to 5 eosinophils/ hpf (Figure 4).
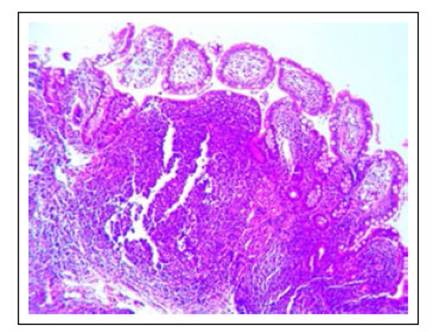
Figure 2 Transverse colon with acute and chronic inflammation, congestion and the presence of lymphoid follicles. 5 eos/c. H/E 100X.
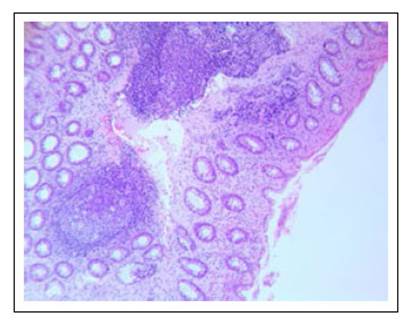
Figure 3 Ileum with moderate acute and chronic inflammation, flattening of villi, presence of lymphoid follicles-up to 6 eosinophils/hpf. H/E 100X.
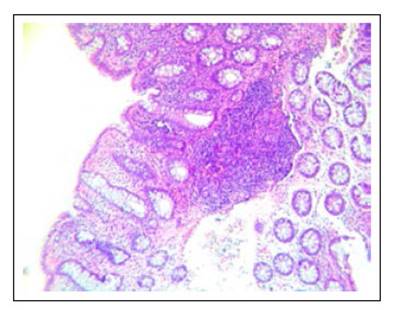
Figure 4 Rectum with acute and mild chronic inflammation, congestion and presence of lymphoid follicles with up to 5 eosinophils/hpf /c. H/E 100X.
Due to the ruling out of Henoch-Schönlein purpura, Crohn´s disease; infectious, rheumatic and neoplastic causes and the finding of atopy and nodular ileocolitis which point to food allergy, a hypoallergenic diet (free of dairy, beef, soy, egg, wheat, nuts , fish and shellfish) was prescribed from 05/09/16. The fever and joint pain subsided from 12/09/16. Once the biopsy results of nodular hyperplasia and infiltrating eosinophils were available, methylprednisolone 1mg/kg/d was indicated from the 16-21st of September and oral prednisone (40 mg/d, for 5 days) was continued at discharge on 22nd September.
During the follow-up the patient was directed to continue a hypoallergenic diet. Corticosteroids were continued at low doses (prednisone 5mg) for 1 month and mesalazine was taken for one year. The patient did not have fever again but there was recurrence of arthralgia on the 12 and 13th of October despite the diet. At later dates there was recurrence of urticarial lesions a few hours after the occasional ingestion of food containing milk and/or wheat. The recurrences were self-limited and less than a week long. They stopped happening in March 2018 and at that time the patient was not taking medication. In his last appointment (19/02/19), the patient said that he did not have the urticarial reaction, but he still avoids wheat.
The improvement was not only clinical but also in the lab results. The IgA normalized (fell to 200.7mg/ dL) and the IgE dropped to 280 IU/ml one year after the hypoallergenic diet. Last tests (09-02-19) showed Hb=12.4mg/dL, leucocytes 5690, platelets 299,000. The patient is asymptomatic from the digestive and rheumatological point of view and was diagnosed by dermatology as a carrier of chronic hives due to his continuing hypersensitivity to wheat.
DISCUSSION
The present case met all diagnostic criteria for systemic JIA (International League of Associations for Rheumatology): arthritis/arthralgia with a limited range of motion, fever for more than two weeks, erythematosus rash for at least one day and generalized adenomegaly 1. This patient also presented uveitis which is a condition frequently associated with JIA, although it is only present in 30% of patients. Nobody knows why it does not occur in all JIA cases but we do know that the aberrant immune response mediated by T cells (Th1 and Th17 phenotypes) is significant in both conditions 5.
In the patient´s second hospitalization, a biopsy of the rash was studied by dermatologists, with Henoch- Schönlein purpura being suspected. The biopsy showed vasculitis of the small blood vessels and negative IgA immunofluorescence, therefore discarding Henoch- Schönlein purpura from the diagnosis. Urticarial vasculitis is an extremely rare manifestation, it is caused by vasodilation and exudation in the skin, accompanied by extravasation of erythrocytes and damage to the walls of the blood vessels. It is reported in connection with the ingestion of some additives and also due to some food types such as eggs, strawberries, nuts, tomatoes, chocolate, dairy and seafood 6.
Due to all the manifestations described, the medical plan was comprehensive and multidisciplinary. This enabled the ruling out of Crohn’s disease; infectious, neoplastic or rheumatologic causes. Finally, the case study led to a suspicion of food allergy owing to the above diseases being discarded, the patient´s history of atopy, repeated urticaria and the endoscopic findings. In hindsight, the evolution of the case clearly showed all the diagnostic phases of food allergy: improvement with a hypoallergenic diet and recurrence of symptoms with the reintroduction of the allergens (recurrence of rash, abdominal pain and arthralgia) 1.
Food allergy is a systemic inflammatory state triggered by allergens in the diet. Food-triggered digestive allergies (rash in this case) come very early in life before other types of manifestations in the respiratory and integumentary systems. This is because the three systems (including the digestive) are the main shock organs. However, we propose that the synovium could be another shock organ, especially in cases labelled as JIA.
There is histological, immunological and clinical evidence supporting the inclusion of food allergy and/or sub-products of the luminal contents of the digestive tract in the genesis of JIA. Studies have shown that up to nine out of ten patients with JIA who have digestive symptoms, have a food allergy. Almost all of these patients have some evidence of activation of the intestinal mucosa, either having biopsies that detected nodular lymphoid hyperplasia or an increased number of intraepithelial lymphocytes or lymphocytes γ/δ+T 7,8. There is also a correlation in the severity of inflammation found and the presence of anaemia or an elevated erythrocyte sedimentation rate. In addition to the inflammatory changes and activation of the intestinal mucosa, there is evidence of increased intestinal permeability and this would explain the possible influence of the bacterial microflora at the beginning of the inflammatory surge triggered by the intestinal luminal content 9,10,11.
Immunological markers are also affected in JIA cases such as the increase in serum immunoglobulin A 12. These changes are also part of the non- IgE mediated manifestations in relation to food hypersensitivity 10,13,14. Serum immunoglobulin A was elevated in our patient at double the normal level and normalized in the follow-up. Another case was reported in Yildiz B & Kural N et al. where the elevation of immunoglobulin A remained the same 12. Therefore our finding is much more significant and is probably linked to the controlling of diet and possible allergens since symptomatic or anti-inflammatory medication, as we know, can only be withdrawn when the disease has been controlled.
From the clinical point of view, there is indirect evidence that exclusive enteral nutrition works with JIA, inducing remission, just as it does in patients with Crohn’s disease 10,11. It has also been reported that, in patients with rheumatoid arthritis, an association exists between dietary intake and disease activity but the evidence is insufficient; this is, in part, due to allergy non-IgE-mediated manifestations being extremely difficult to identify 1. Nevertheless, a European epidemiological study determined the odds ratio (ORs) for the intake of red meat and derivatives in relation to inflammatory polyarthritis (RA), finding significant association (OR 2.9) 13.
The level of bacteria in the intestinal luminal content is very high in the colon. The bacterial microbiota is closely associated with the gut-joint axis, which is now being recognised as part of the genesis of food allergies 1. A series of immunological events are triggered from this content due to the incorrect functioning of the intestinal barrier. Gram-negative bacteria carry lipopolysaccharide (LPS) in their outer membrane. The absorption of LPS binding protein (LBP) is up-regulated by the LPS, and in turn increases innate immunity to bacterial infections. The LPS linked to LBP is transferred by CD14, expressing in monocytes the complex toll-like receptor 4 (TLR-4)/ myeloid differentiation factor 2 (MD2). Activation of this TLR4/MD2 complex triggers inflammation. LPS induces apoptosis of human cartilage chondrocytes. In addition, LBP has been found to be associated with joint inflammation based in high intra-articular concentration levels seen in rheumatoid arthritis.
There is also α-1-acid glycoprotein, which is another acute phase protein reactant with immunomodulatory properties that neutralizes the toxicity of LPS and accelerates its clearance from the body. This concentration of α-1-acid glycoprotein is associated with inflammatory bowel disease activity and JIA 9,11. Thus, the natural course of JIA could be related to intestinal microflora, and in turn, with antibiotic abuse at an early age. Dysbiosis has been seen in patients with rheumatoid arthritis, the implication of this finding is reinforced by the clinical improvement reported in arthritis cases which receive therapeutic treatment for bacterial overgrowth 11.
Another point is that genetics also intervenes. Reactive arthritis in humans seems to be related to a combination of microbial/diet impact on the intestinal mucosa and genetic predisposition to an aberrant immune response. For example, 90% of patients with ankylosing spondylitis express HLA-B27 and are thus associated with Crohn’s disease and ulcerative colitis. Animal experiments have demonstrated a diffusion of dietary antigens soon after feeding which would initiate the formation of immune complexes at the synovial level and autoimmune reactions in the joints. Patients with ankylosing spondylitis have high intestinal levels of IgM and IgA in direct correlation with disease activity 8.
Although the patient displayed clinical improvement with a hypoallergenic diet, a short course of corticosteroids was prescribed due to the severe systemic inflammation that was seen in the uveitis, urticarial vasculitis and nodular hyperplasia. Anti-inflammatory therapy with mesalazine was then continued and it was reported as beneficial for both conditions. Literature states that treating patients with sulfasalazine for at least 16 weeks reduces the increased level of antibodies, suggesting it has an intestinal immunosuppressive response. It has been proposed that this drug decreases mucosal intestinal permeability 15.
In conclusion, there is evidence supporting the existence of a gut-joint axis, where the luminal content (both diet and microflora) triggers a series of immunologically mediated reactions that can cause systemic diseases such as JIA. Since this condition´s name includes the term "idiopathic", we suggest that part of the medical plan includes a therapeutic trial with a hypoallergenic diet prior to therapy escalation, which leads to undesirable side effects not seen on the hypoallergenic diet. Therefore, we put forward that food allergy is possibly one of the causes of juvenile idiopathic arthritis and also that a hypoallergenic diet would allow the control of the symptoms.