INTRODUCTION
Drug-induced esophageal ulcers are an acquired chemical injury to the esophageal mucosa caused by the direct caustic effects of oral medications 1. Although various drugs have been implicated in this condition, antimicrobial agents account for more than 50% of cases, with tetracyclines, particularly doxycycline, being accountable for the majority of the reported cases 2. Mucosal damage occurs due to the direct contact of the drug tablet with the esophageal mucosa, resulting in erosions and ulcers, which may present in a specular distribution 3. We report a case of a patient who developed "kissing ulcers," identified during an esophagogastroduodenoscopy following doxycycline ingestion.
CASE REPORT
A 34-year-old woman with a 6-week history of daily 100 mg doxycycline intake indicated for rosacea presented with an episode of a reported sensation of food impaction that improved with fluid intake. Subsequently, she developed a two-week history of dysphagia, epigastralgia, pyrosis, and an unquantified feverish sensation, prompting her to seek medical attention.
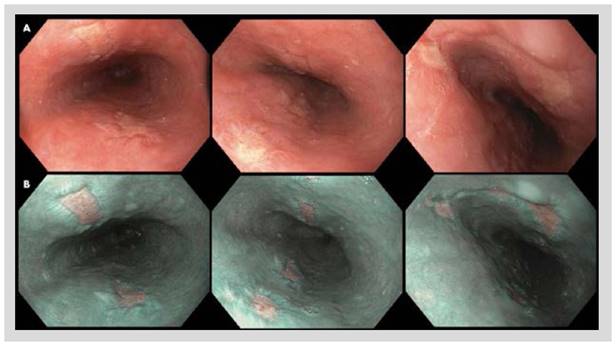
Esophagogastroduodenoscopy was performed, revealing multiple ulcers in the midportion of the esophagus (Figure 1A) with a specular distribution. Narrow-band imaging (NBI) evaluation of the esophageal mucosa showed complete distortion of the esophageal mucosal surface (Figure 1B), findings consistent with drug-induced esophageal ulcers. Biopsies were obtained for further evaluation. Histopathological analysis with hematoxylin and eosin staining revealed keratinocyte hyperplasia in the basal layer of the squamous epithelium, spongiosis, and a slight increase in intraepithelial lymphocytes, without evidence of eosinophilic infiltration in the mucosa. No additional studies were deemed necessary. The treatment plan included discontinuation of doxycycline, initiation of double-dose proton pump inhibitors (PPIs), and administration of oral sucralfate twice a day. The patient showed favorable clinical evolution, with complete symptomatic remission at six weeks. No followup esophagogastroduodenoscopy was requested after the completion of treatment.
DISCUSSION
Esophageal ulcers that present in a specular distribution are strongly indicative of chemical injury to the esophageal mucosa. In this report, we describe a case of "kissing ulcers" following doxycycline ingestion, a drug that accounts for the majority of such cases 2,4. Patients receiving treatment with tetracyclines, particularly younger individuals, for conditions such as rosacea, acne, or urinary tract infections are especially vulnerable to this acquired condition 5,6. However, esophageal ulcers of a similar nature have also been associated with other medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), antihypertensive agents, bisphosphonates, warfarin, among others 2, which are often prescribed for elder populations, potentially increasing the risk of esophageal injury in this demographic group.
The pathogenesis of drug-induced esophageal ulcers involves drug-specific properties and patientrelated factors, including anatomical and physiological characteristics. Among drug-specific factors, the direct caustic effect of medications with hyperosmolar properties is considered a leading mechanism 7. Medications with a low pH, such as certain antibiotics, may similarly contribute to mucosal damage (1,7 . Additionally, pharmaceutical formulations such as capsules have been shown to adhere to the esophageal wall, prolonging mucosal exposure to the drug and thereby increasing the risk of injury. Conversely, oral suspensions and syrups tend to minimize this risk due to their rapid transit through the esophagus. Moreover, certain behaviors, such as lying down immediately after drug ingestion or consuming insufficient water during ingestion, have been identified as modifiable risk factors 8,9.
Patient-specific factors also play a critical role in the development of esophageal ulcers. Conditions such as esophageal motility disorders or decreased saliva production, commonly observed in patients with connective tissue diseases or older populations 10, can lead to prolonged transit times and increased direct exposure of the esophageal mucosa to the drug. Anatomical considerations, such as the proximity of the mid-esophagus 1,4 to the aortic arch, may result in extrinsic compression, further impairing pill clearance and predisposing this region to injury.
The clinical presentation of drug-induced esophageal ulcers typically includes the sudden onset of symptoms such as chest pain, dysphagia, and odynophagia, usually occurring with a latency of 10-14 days after drug initiation 4,9. While many patients experience self-limiting symptoms, this often leads to under recognition and under estimation of this condition 1. Prompt diagnosis and management are crucial to prevent severe complications, including esophageal perforation 11 or bleeding 12. A thorough medical history focusing on recent medication use should raise clinical suspicion when evaluation of recent onset of dysphasia or chest pain. Esophagogastroduodenoscopy remains the gold standard for diagnosis, often revealing characteristic findings such as mucosal erythema, erosions, bleeding ulcers, or impacted pill fragments. Particularly, a "kissing ulcer" presentation is reported in 7.6% to 43.6% of cases 3,13. Chronic complications, such as esophageal strictures, may arise from ongoing mucosal damage, particularly in patients using NSAIDs over prolonged periods 14. This report adds to the existing literature by including high-definition endoscopic images with NBI, an optical technique not frequently reported in prior cases.
Histopathological findings in drug-induced esophageal ulcers can vary significantly. While intraepithelial eosinophilic infiltration is frequently observed, supporting eosinophilic esophagitis as a key differential diagnosis 15, this feature was absent in the present case. Instead, nonspecific acute inflammatory changes were identified, further emphasizing the heterogeneity of tissue responses in this condition 9.
Treatment involves discontinuation of the causing agent and initiation of PPIs or oral sucralfate to mitigate to facilitate mucosal healing and minimize gastric acid reflux 3. In cases where discontinuation of the causative agent is not feasible, switching to an alternative pharmaceutical formulation should be considered. Preventive measures, such as ingesting at least 100 mL of water with medications and avoiding lying down for 15-30 minutes post-ingestion, have been recommended by some authors to reduce the risk of esophageal injury 4. Drug-induced esophageal ulcers are typically self-limiting, with symptom resolution expected within two weeks. Routine follow-up endoscopy is generally unnecessary unless symptoms persist, in which case further evaluation is warranted.
Drug-induced esophageal ulcers are a rare but significant complication of medication use, particularly associated with tetracyclines like doxycycline. While typically self-limiting, prompt recognition and appropriate management are crucial to prevent complications such as strictures or perforation. A thorough history of medication use, supported by diagnostic endoscopy, facilitates timely diagnosis. Preventive measures, including adequate hydration and avoiding recumbency post-ingestion, are essential in reducing the incidence of this condition.