Introduction
Cryptococcus neoformans, a yeast-like fungus, exhibits a remarkable capacity for adaptation in variable environments, allowing it to survive both in the environment and in the host. Its association with severe and sometimes fatal infections in immunocompromised patients, such as meningoencephalitis and pneumonia, is well known. 1,2 Although Cryptococcus endocarditis is rare, its presentation and clinical course have been documented on rare occasions over the years. 3 This article provides a detailed description of the presentation and clinical course of a patient who developed Cryptococcus endocarditis on a native valve, a rare but clinically relevant phenomenon.
Case report
A 36-year-old female patient with a history of stage IV chronic kidney disease since 2018 and severe malnutrition presented to the adult emergency department with symptoms of asthenia, fever, intense itching, and generalized pain. On admission, the following laboratory studies were notable: serum creatinine of 17.5, urea 252 mg/dL hyperkalemia of 7.8 mEq/L, severe anemia (hemoglobin 6.07 mg/dL), and thrombocytopenia 12,000/μL. Due to the urgent need for dialysis, a temporary right femoral catheter was placed to initiate hemodialysis. During hospitalization, she developed a persistent fever, prompting central and peripheral blood cultures, which isolated methicillin-sensitive Staphylococcus aureus. A transthoracic echocardiogram (TTE) revealed thickening and sclerosis of the mitral valve leaflets, with a suggestive image of vegetation attached to the anterior leaflet measuring 13 x 15 mm, and severe insufficiency. Based on these findings and the antibiogram, empirical antibiotic therapy with ceftriaxone was initiated. After 34 days of treatment and subsequent negative blood cultures, along with clinical improvement, she was discharged while continuing renal replacement therapy with hemodialysis.
Twenty days after discharge, she returned to the emergency department due to persistent fever of up to 38.5 °C. Physical examination revealed uremic frost, increased abdominal girth due to ascitic fluid, and edema of the lower extremities. Blood cultures were repeated, and the results showed the growth of Cryptococcus neoformans five days later. A repeat set of blood cultures confirmed this microorganism. Upon finding this pathogen, a chest tomography was performed, revealing hypodensity in multiple areas of the upper lobes, as well as multiple atelectasis and bilateral pleural effusion (Figure 1A). A new transthoracic echocardiogram was performed, showing persistent vegetation measuring 10 x 7 mm predominantly on the posterior leaflet of the mitral valve in the two-chamber apical view, now causing severe regurgitation with a Coanda effect in the long-axis and four-chamber views (Figures 1B, 1C, and 1D). The new Duke 2023 criteria were used in the patient, including among the minor criteria: prior history of Infectious Endocarditis (IE), documented temperature >38 °C. Among the major criteria: positive blood cultures rarely causing IE isolated in three separate blood cultures, significant new valvular insufficiency on echocardiography compared to previous images.
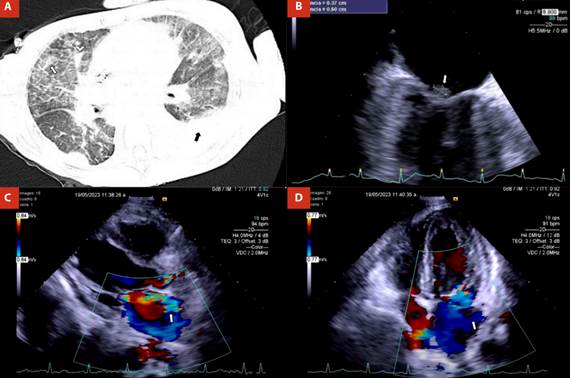
Figure 1 A) Chest computed tomography with multiples areas of hypodensity in the upper lobes, as well as atelectasis, bilateral pleural effusion, and consolidations. B) Two-chamber view in transthoracic echocardiography showing the vegetation of 10x7 mm on the posterior leaflet of the mitral valve. C) Long-axis view, and D) Four-chamber apical view in transthoracic echocardiography showing severe mitral regurgitation.
As part of the approach, laboratory tests were conducted to rule out human inmunodeficiency virus (HIV) infection and other underlying immunodeficiencies, which were negative. A lumbar puncture was performed, revealing glucose of 28 mg/dL and proteins of 44.76 mg/dL. The cerebrospinal fluid culture isolated Cryptococcus neoformans. Subsequently, a paracentesis was performed with a cytological study showing a GASA < 0.1, along with a peritoneal fluid culture reporting the same previously mentioned microorganism. Due to the findings on the echocardiogram, she was transferred to the cardiology department of Hospital Civil Fray Antonio Alcalde for surgical intervention. However, due to the severity of the disseminated infection and the patient's severe malnutrition, she died before valve repair could be performed.
Discussion
Infective endocarditis is a disease that affects mainly the endocardial surface of the heart and cardiac valves (native or prosthetic), as well as indwelling cardiac devices. In recent years, the annual incidence has varied from 7 to 15 cases per 100,000 population. 4) The main risk factors have been male sex, older age, intracardiac shunts, prosthetic valves, rheumatic, and congenital heart disease, intracardiac devices, intravenous drugs use, immunosuppression, and hemodialysis. Historically, women have had worse prognosis than men, and the in-hospital mortality rate ranging from 14 to 22%. 5
Historically, Streptococci and Staphylococci spp. have been the most frequently isolated organisms, accounted collectively for approximately 80% of IE cases. However, this proportion varies by region (Staphylococci spp. is most prevalent in North America; Streptococci spp. is most prevalent in South America and Europe) 6. In a non-cardiovascular center in Mexico, in a ten-year period, it was described that Staphylococci species were the most frequent isolated organisms (45%, mainly S. aureus). On the other hand, the most common fungal organism in infective endocarditis is Candida albicans (24-46%), followed by Aspergillus spp. (25%), which is consistent with Mexican epidemiology, where fungi were present in 9.6% of cases, being candida species the only fungal organism, which are associated with the worst prognosis. 7,8
In this case, our patient was a young woman in hemodialysis (end-stage renal disease) with mitral valve infective endocarditis related to a fungal pathogen (C. neoformans), with several risk factors for a gloomy prognosis. Also, in the case recompilation of Cryptococcus neoformans infective endocarditis (12 cases until now) by McGuire and Walter 2 five patients (41.6%) died due to a disseminated infection. Interestingly, only 3 previous cases with a native valve involvement have been described, being aortic and mitral valves the only affected valves. This finding can be explained due to endocarditis is developed in a secondary manner, after an initial fungemia that starts in another site (central nervous system and/or lungs). 9
The clinical presentation of patients with fungal endocarditis is usually like other causes of endocarditis. However, the diagnosis is often delayed due to negative blood cultures, which translates into a delay in anti-fungal therapy. Interestingly, Pappas 10 described that non-HIV/non-transplant patients, cryptococcosis affected mainly the lungs and had a higher rate of death at 90 days and one year of follow-up. In the clinical and demographic characteristics, seven patients (6%) were classified with end-stage renal disease, which is consistent with our case.
It is important to mention that chronic kidney disease (CKD) is linked to a broad impairment of almost every aspect of the immune system, creating a distinct condition of "chronic inflammatory immune depression." The effects on the innate immune system in CKD may stem from the buildup of uremic toxins, higher levels of pro-inflammatory molecules, increased oxidative stress, and reduced erythropoietin production. Additionally, CKD patients tend to have T-cell lymphopenia and have abnormal activation of fully differentiated memory cells, and an imbalance between regulatory T cells and T helper 17 cells. These T-cell irregularities are linked to uremic toxins, oxidative stress, secondary hyperparathyroidism, iron overload, and inflammation. Moreover, CKD is associated with a significant deficiency and malfunction of B cells, driven by increased apoptosis and hindered maturation. 11,12
Diagnosis of fungal endocarditis is based on the new Duke’s Criteria. 13 Interestingly, it is described that in cases of Cryptococcus endocarditis, most blood cultures will return positive (as in this case). However, the probability of an in-hospital acquired fungal infection is high, which is like the results described by Ruiz-Beltrán et al. 7 where 56.5% of cases were classified as health care-associated infective endocarditis, being the most frequent cause the presence of intravenous access device in 46.8% of them.
In conclusion, this case provides additional information to the international literature about how Cryptococcus neoformans can affect patients with several risk factors (chronic kidney disease, hemodialysis, malnutrition, female sex), and could develop to a fatal outcome. These cases are necessary due to the exceptionally low percentage of patients who develop cryptococcal endocarditis.















