INTRODUCTION
The World Health Organization (WHO) has recently stated that no health or sustainable development can be achieved without mental health 1. In addition, psychiatric disorders are now recognized as major causes of morbidity, burden of disease, and health costs 1,2,3. In 2019, major psychiatric disorders (mainly anxiety and depression) accounted for 970 million cases, increasing by half the number of cases in 1990 2,3. Similarly, the number of disability-adjusted life-years (DALYs) attributable to psychiatric disorders have raised from 81 million to 125 million during the same period 2,3, the latter representing 1 out of 5 DALYs globally 1. In this line, global (e.g., WHO) and regional (e.g., Pan American Health Organization) organizations have launched initiatives to promote and increase the access to mental health care and, thus, reduce the consequences of psychiatric disorders (e.g., suicide mortality) 1,4,5. Hence, metrics that focus on mental health care (e.g., outpatient visits) could help to tailor mental health strategies, specially across low- and middle-income countries (LMICs) like Peru.
Characterizing the frequency of psychiatric disorders at the outpatient setting has several benefits because it measures the utilization of health care services 6. From the healthcare system perspective, characterizing the population that visits health services due to psychiatric disorders is important for the corresponding planning 7. From the public health perspective, the frequency of psychiatric disorders at the outpatient setting conveys one of the greatest burdens in the Peruvian health system and, therefore, where mental health policies should be directed. Furthermore, it is unknown whether and how much the COVID-19 pandemic and the subsequent lockdown affected the flow of psychiatric outpatient visits in the country, an important to guide for the Peruvian health system’s response to ongoing and future global or local health emergencies.
To provide evidence of the national frequency and monthly trends of psychiatric disorders in the outpatient setting of Peru, outpatient morbidity registries between 2018-2021 were analyzed. This information is important for both national and subnational organizations working on mental health policies in Peru and other LMICs in order to guide the development of preventive strategies and the allocation of resources. Furthermore, to highlight subnational inequalities in terms of healthcare utilization for psychiatric disorders, we also described the number of psychiatric outpatient visits in relation to population at the province level. This evidence could help to track progress towards the materialization of the objectives of the recently launched Peruvian Mental Health Law, which pursue a universal mental health coverage in the country 8.
METHODS
1.1. Study overview
This is a cross-sectional study of outpatient morbidity data from the National Health Superintendence (SUSALUD, acronym in Spanish) of Peru. Outpatient visits for psychiatric diagnoses were identified and gathered into major groups. The frequency of each group of psychiatric disorders is described by demographic and health care facility (HCF)-related variables. Monthly trends of each group of psychiatric disorders and the number of outpatient visits per 10,000 population at the subnational level are also described.
1.2. Study setting
Peru is an upper-middle income country with a population of 33 million people 9. It is subdivided in three geographic levels: region > province > district. Our findings will be summarized at the national and province level; it was not done so at the district level because of the limited number of observations (i.e., visits). Peru is also divided in three natural geographic regions: Coast (next to the Pacific Ocean), Highlands (crossed by the Andes Mountains) and Jungle or Amazon (rainforest mostly bordering East with Brazil); these geographic areas were also used to characterize the findings.
Peru has a fragmented healthcare system, in which the most salient insurance providers are: the SIS (Seguro Integral de Salud, in Spanish), run by the Ministry of Health (MINSA, acronym in Spanish), mainly targeting people with limited financial resources and providing care to ~60% of the population; ESSALUD, which is run by the Ministry of Labour, provides care for people formally employed; Armed Forces and Police, funded by the Ministry of Defense; and private health insurance providers, which are commonly used by wealthy people 10,11.
1.3. Data source
Outpatient morbidity data between 2018 and 2021 from SUSALUD were analyzed 12. These data are not recorded at the individual level, and contain information (in absolute numbers) about the monthly outpatient visits in every HCF from all health sectors in Peru; this implies that an individual patient could have accounted for multiple visits. SUSALUD also records information about the patient (sex, age group, and diagnosis by the International Classification of Diseases 10th revision [ICD-10] codes), and the HCF in which the visit occurred (geographical location, level of complexity, health sector). SUSALUD data are available since January 2018 and are updated every month 12.
Population data at the province level were retrieved from the Peruvian National Centre for Strategic Planning (CEPLAN, acronym in Spanish) 13; the latest year available for these data was 2019. Data at the province level on human development index (HDI) in 2019 13, and proportion of the population living in poverty (presented as percentage, in 2018) 13, were also retrieved from CEPLAN. The proportion of people living in rural areas (presented as percentage of the total population, in 2017) was retrieved from the Peruvian National Census 14.
1.4. Study population
A complete-case analysis of psychiatric outpatient visits was conducted. First, outpatient visits with a psychiatric diagnosis using the ICD-10 codes for mental and behavioural disorders, were identified: F00-F99. Second, individual psychiatric diagnoses were included into 12 major groups: 1) Anxiety disorders (F40-F42, F43.0, F43.1, F93.0, F93.1, F93.2, F93.8); 2) Bipolar disorders (F30, F31, F34.0); 3) Conduct disorders (F91); 4) Depressive disorders (F32-F39); 5) Eating disorders (F50); 6) Mental retardation (F7); 7) Organic mental disorders (F0); 8) Psychological development disorders (F8); 9) Schizophrenia spectrum disorders (F2); 10) Sleep related disorders (F51); 11) Substance use disorders (F1); and 12) Other mental disorders (ICD-10 codes not elsewhere classified). This categorization was based on the Global Burden of Diseases (GBD) 2019 Study regarding mental disorders 2 and other recent works 15. This was done in order to ensure comparability with studies on the burden of psychiatric disorders.
1.5. Variables
The following variables were used to describe the psychiatric outpatient visits: sex and age of the patient, date of the visit, and level of complexity and health sector of the HCF.
Rather than a continuous variable, age was originally coded in 5-year groups (except for three of them: 0-1, 1-4, and ≥65 years). To provide the most granular evidence and to be consistent with the GBD 2019 Study for mental disorders (2), we kept the original age groups; thus, the age groups herein analyzed were: 0-1, 1-4, 5-9, 10-14 ,15-19, 20-24, 25-29, 30-34, 35-39, 40-44, 45-49, 50-54, 55-59, 60-64, 65+ years.
The level of complexity of each HCF was originally coded in three levels: I (primary HCFs), II (secondary HCFs), and III (tertiary HCFs, e.g., hospitals). Of note, the higher the level, the more services the HCF provides. When describing the absolute number of psychiatric outpatient visits by this variable, those with other codes (e.g., "0") were excluded because we assumed it was a data entry error; this only represented 3.0% of all psychiatric outpatient visits.
The health sector of each HCF was grouped these into five categories: 1) MINSA; 2) EsSalud; 3) Armed Forces and Police; 4) Private; and 5) Others.
1.6. Statistical analysis
This is a descriptive analysis conducted with the R (version 4.1.2) that includes three main aims: 1) To describe the frequency of each group of psychiatric disorders in the outpatient setting at the national level; 2) To describe monthly trends in the relative and absolute number of outpatient visits for each of such groups; and 3) To characterize the levels of utilization of psychiatric outpatient care at the subnational level.
For the first aim, the outcome variable was visits per year. The outcome in each group of psychiatric disorders (e.g., anxiety disorders) was described by sex, age groups and HCF-related variables using absolute numbers and proportions above all psychiatric visits (i.e., the denominator was all psychiatric outpatient visits). Because the highest number of observations (i.e., visits per year) was in 2019 and this year was not affected by the COVID-19 pandemic, the results in 2019 were included on the main text.
For the second aim, the outcome variable was visits per month. The outcome in each group of psychiatric disorders was described using absolute numbers (i.e., absolute number of visits per month) and proportions above all psychiatric visits. To compare the average monthly visits in different years (e.g., 2019 vs 2020), unpaired t-tests were used to document if the monthly number of psychiatric visits was different in 2020 because of COVID-19 (e.g., lockdown). A p-value <0.05 was considered statistically significant.
For the third aim, the outcome variable was visits/year/population. At the province level, the outcome in relation to its population was described, specifically, outpatient visits per 10,000 people 16. The outcome for all, combined psychiatric disorders was assessed. Results for 2019 are presented on the main text. We also described the outpatient visits per 10,000 people at the province level in 2019 in relation to HDI 13, proportion of the population living in poverty 13, and proportion of people living in rural areas 14. Scatterplots which included the Pearson’s correlation coefficient and p-value were used. The correlation coefficients are reported as an aid to identify potential patterns. The correlation coefficients should not be interpreted as the strength of the association between these two variables, nor in terms of causality.
1.7. Ethics
This analysis used open-access data from SUSALUD (http://datos.susalud.gob.pe/dataset/consulta-b2-morbilidad-en-consulta-ambulatoria ). These data do not contain personal identifiers, as they are aggregated by month and HCFs, not by individuals. Therefore, approval by an Ethics Committee was not sought and consent was not required.
RESULTS
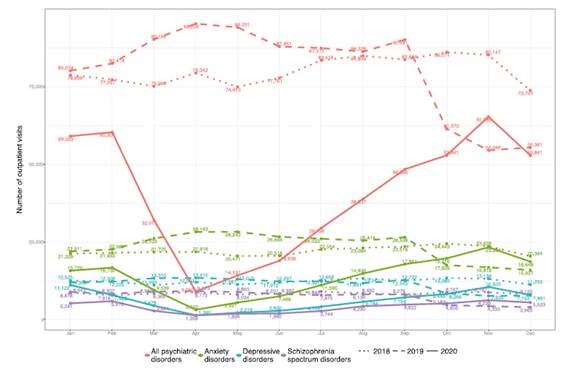
Between 2018 and 2021, a total of 3,062,618 outpatient visits due to psychiatric disorders in Peru were registered, a figure that represented 2.3% of all outpatient visits (Table 1). This proportion increased slightly within the studied period: from 2.0% in 2018 to 2.8% in 2021. Out of all outpatient visits destined for psychiatric disorders in 2018-2021, 54.7% were in women, and 58.2% in those aged 15-64 years (i.e., working age). Stratified by HCF levels, 39.6% and 39.0% of all outpatient visits for psychiatric disorders took place in secondary and tertiary HCFs, respectively. Half of the outpatient visits for psychiatric disorders (50.7%) took place in MINSA HCFs. The 48.5% of all psychiatric outpatient visits took place in Lima, whereas only 0.2% took place in Madre de Dios (Amazon region).
National frequency of psychiatric disorders in outpatient care
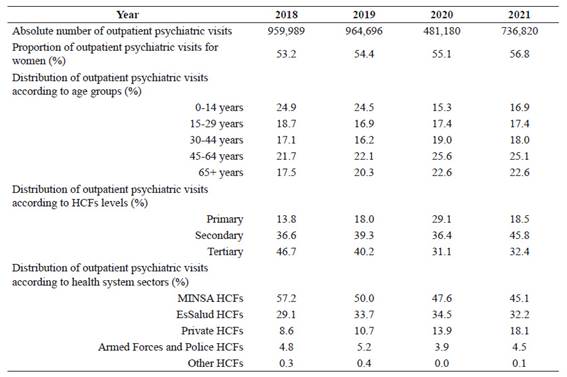
Between 2018-2021, there were little variations in the relative contribution of specific groups of psychiatric disorders to the total outpatient burden of psychiatric disorders (Figure 1); nonetheless, the psychiatric outpatient burden differed by sex and age. The absolute number of psychiatric outpatient visits shifted from men in younger age groups to women in older age groups; for example, in 2019, 65.7% of all psychiatric outpatient visits in those aged <15 years were from men vs. only 36.1% among those aged ≥65 years were in men (Figure 1).
Results for 2018, 2020, and 2021 are presented in Supplementary Figures 2-4. Similar figures but showing the proportion of visits above all psychiatric visits for each psychiatric disorder are shown in Supplementary Figures 5 (overall) and 6-8 (stratified by HCF level).
Figure 1 Outpatient visits by groups of psychiatric disorder, sex, and age groups, 2019.
In the working age groups (i.e., 5-year age groups between 15-64 years), most psychiatric outpatient visits were due to anxiety disorders regardless of sex; of note, the proportion of all psychiatric visits for anxiety disorders increased with older age groups and was higher in women (~40-47% in 2019) than men (~30-33% in the same year). The psychiatric disorders that accounted for the second highest number of psychiatric outpatient visits in the working age groups varied by sex; in 2019, they were schizophrenia spectrum disorders in men (except in those aged 15-19 years) and depressive disorders in women. The proportion for depressive disorders decreased with older age groups in women but increased with older age groups in men >35 years; across working age groups, proportions were consistently higher in women (~22-26%) than men (~10-14%). Notably, the proportion for organic mental disorders peaked in those aged >65 years (29.2% in men, and 24.5% in women; 2019).
In general, the same relative frequency of psychiatric disorder groups was observed when stratified by HCF levels. Nonetheless, schizophrenia spectrum and bipolar disorders were most frequent in tertiary HCFs, whereas anxiety and sleep related disorders were most frequent in primary and secondary HCFs.
Monthly trends of the number of outpatient visits for psychiatric disorders
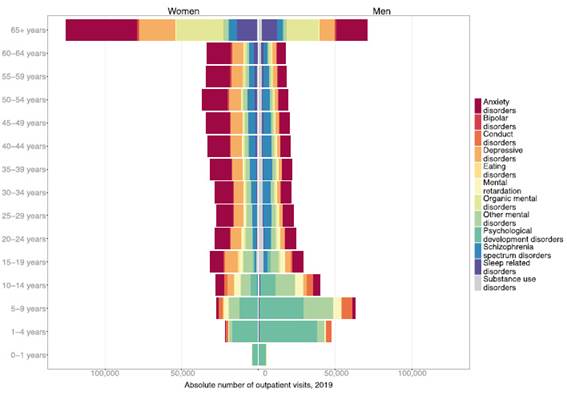
Monthly variations were noticed regarding the absolute number of visits for the combined group of psychiatric disorders and the three psychiatric disorders with the highest number of visits (i.e., anxiety, depressive, and schizophrenia spectrum disorders) before the COVID-19 pandemic (2018-2019). Nonetheless, there were no monthly differences in the proportion of psychiatric visits for each of those three disorders. The monthly average number of outpatient visits in 2019, was 80,391 for all psychiatric disorders, 21,339 for anxiety disorders, 11,396 for depressive disorders, and 7,456 for schizophrenia spectrum disorders (Figure 2). For the combined group of psychiatric disorders and the three psychiatric disorders with the highest number of outpatient visits (i.e., anxiety, depressive, and schizophrenia spectrum disorders), we observed two peaks in the absolute number of outpatient visits in 2019. The first peak began in February and peaked in April/May, while the second one began and peaked in September.
Results by HCF levels are presented in Supplementary Figure 9. Results for the rest of psychiatric disorders are presented in Supplementary Figure 10. We only included results for 2018, 2019, and 2020 for better data visualization.
Figure 2 Monthly trends of the absolute number of outpatient visits for all psychiatric, anxiety, depressive and schizophrenia spectrum disorders, 2018-2020.
The monthly average of outpatient visits in 2020 was 40,098 for all psychiatric disorders, 11,897 for anxiety disorders, 6,144 for depressive disorders, and 3,999 for schizophrenia spectrum disorders; these were significantly lower than the monthly average of outpatient visits in 2019 (p<0.05 for all and each psychiatric disorder) and 2018 (p<0.05). In March-April 2020 (i.e., after the beginning of COVID-19 lockdown in Peru), a sharp decrease was observed in the absolute number of monthly outpatient visits for all, anxiety, depressive and schizophrenia spectrum disorders compared with January-February 2020 and March-April 2019 (Figure 2); this finding was consistent in all HCF levels and in the rest of psychiatric disorders. In March and April 2020, the absolute number of outpatient visits for all psychiatric disorders dropped by 65% and 90% compared with March and April 2019, respectively. This finding was consistent across all specific groups of psychiatric disorders.
Since May 2020, the absolute number of monthly outpatient visits for all, anxiety, depressive and schizophrenia spectrum disorders heavily increased; after October 2020, it even surpassed the absolute numbers of visits in 2019. After June 2020, the proportion of psychiatric visits above all outpatient visits slightly increased and surpassed the proportions in previous months (e.g., 3.1% in September 2020 vs 1.9% in March/April 2020) and in 2019 (e.g., 1.7% in September 2019).
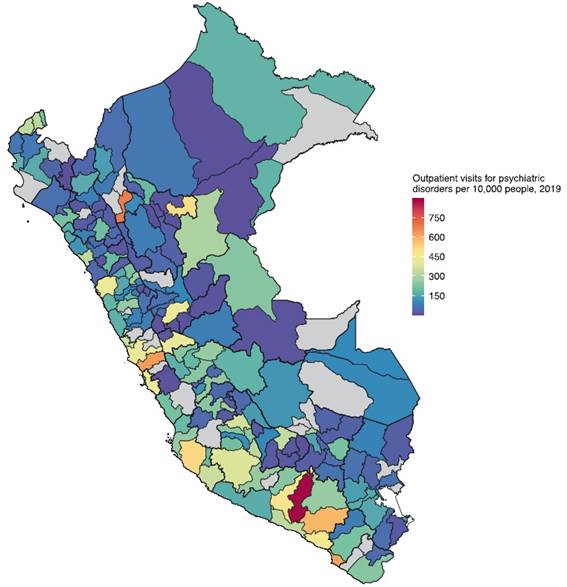
Subnational frequency of psychiatric disorders in outpatient care
At the province level, there was high variability in the number of psychiatric visits relative to the province population (Figure 3). The provinces with the highest psychiatric outpatient visits per 10,000 population were mainly in the Coast, whereas provinces with the lowest numbers were in the Highlands; this finding was consistent across the years, although visits per 10,000 population decreased in most provinces in 2020 and 2021. In regions with both Coast and Highlands areas, psychiatric outpatient visits per 10,000 population decreased from the Coast to the Highlands; for instance, in 2019, in the Ancash region, Santa (Coast) had the highest outpatient visits per 10,000 population (425), whereas Antonio Raymondi (Highlands) had the lowest level (7 visits per 10,000); that is, although both provinces are in the same region (~170 km apart), the visits per 10,000 population were 60 times higher in the coastal locality.
Results for 2018, 2020, and 2021 are presented in Supplementary Figure 12.
Figure 3 Number of outpatient visits for psychiatric disorders per 10,000 people, 2019.
At the province level, there was a moderately positive correlation between the number of psychiatric outpatient visits per 10,000 population with HDI (p<0.05), yet a moderately negative correlation with the proportion of people living in poverty (p<0.05) and in rural areas (p<0.05) (Supplementary Figure 13).
DISCUSSION
Leveraging on a nationwide registry of ambulatory visits, the first national and subnational estimates of the frequency of major psychiatric disorders in the outpatient setting of Peru have been provided. It was found that half of the outpatient visits due to psychiatric disorders took place in the capital city of Peru (Lima), which hosts a third of the Peruvian population, and encompasses 37% of all HCFs 17. Also, across working age groups, from all outpatient visits for psychiatric disorders, those identified as anxiety/depressive disorders represented approximately 6 out of 10 visits in women, and 4 out of 10 visits in men. Monthly trends of the major psychiatric disorders in outpatient care during the pre-pandemic period in Peru showed two peaks in the absolute number of visits: April-May and September. After the beginning of lockdown, the absolute number of monthly outpatient visits for the major psychiatric disorders dropped by more than a half (compared to 2019) but increased after May 2020. After three months of lockdown, the proportional contribution of psychiatric visits to the total outpatient burden started to increase. When analyzing subnational trends, provinces in the Highlands had lower psychiatric visits per 10,000 population compared to Coastal provinces.
Public health relevance
Our results indicate which psychiatric disorders are the most important drivers of the burden of outpatient visits in Peru. This finding has relevant implications in Peru and similar countries (e.g., Andean Latin America) from a public health perspective, as it informs and substantiates decisions on mental health policies by local health authorities. As anxiety/depressive disorders represent most of the outpatient visits for psychiatric disorders in Peru, mental health policies should guarantee the inclusion of specific health service planning strategies for them, i.e., increasing the availability of appointments for mental health counselling, and increasing the number of options for pharmacological treatment. Furthermore, while local clinical guidelines for depressive and schizophrenia spectrum disorders are available 18,19, there is a need for clinical guidelines for anxiety disorders adapted to the Peruvian population.
As mentioned above, in 2018 and 2019, the absolute number of monthly outpatient visits for the major psychiatric disorders in Peru (i.e., anxiety, depression, and schizophrenia spectrum) peaked in April-May and September: it can, then, be concluded that HCFs in Peru should be prepared to receive more psychiatric visits during these periods. To face such situation, the availability of psychiatric drugs, the number of mental health workers, and restructure schedules should be increased to minimize contact among outpatients (according to current COVID-19 guidelines). Furthermore, as the number of people living with psychiatric disorders is expected to increase because of population growth 2, other general measures could also help to reduce the burden of psychiatric outpatient visits, such as offering mental health services virtually or at the patient’s home and implementing electronic medical records 20,21.
We observed large subnational differences in the psychiatric outpatient visits per population; in particular, provinces in the Highlands had lower psychiatric outpatient visits per 10,000 people than Coastal provinces. This finding calls for urgent actions to improve the access to mental health care in Peru, particularly in the Highlands. The latter is currently endorsed by the Peruvian Mental Health Law, which seeks to guarantee the universal access to mental health care in the whole country 8. People living in the Highlands are often poor (e.g., 50.4% of poverty in rural Highlands) and live in rural areas (e.g., 60% in Huancavelica, a region crossed by the Andes) 22,23. Considering that people living in poverty and rural areas are less likely to seek mental health care 24, this could result in a lower number of outpatient visits for psychiatric disorders. This is consistent with ecological analyses at the provincial level, which shows that localities with low HDI and high levels of poverty and rurality had lower psychiatric outpatient visits per 10,000 people. Of note, these differences could also be attributed to the lower number of healthcare workers and HCFs in Highland provinces 25, as well as to the strong stigma regarding mental disorders, and the registry underreporting in the Highlands 26.
Results in context
We have provided the first national evidence of the burden of different groups of psychiatric disorders in the outpatient setting in Peru. Our study is positioned to inform clinicians and public health authorities from Peru and countries with similar profiles, about their health system and frequency of psychiatric disorders, relevant aspects of any planning of healthcare delivery at this setting.
Our results indicate an abrupt decrease in the number of psychiatric outpatient visits across all HCFs during the first months of the COVID-19 pandemic in Peru (March/April 2020), which corresponds to the beginning of the strict lockdown period established by the Peruvian Government 27. Other countries have also reported a similar phenomenon during the pandemic. In Brazil, there was a 28% decrease in the number of mental health outpatient visits, coupled by an increase in the number of mental health emergency visits 28. At a South Korean hospital, there was a 13.1% reduction in the number of mental health outpatient visits, compared to the number before the pandemic 15. At the largest admitting psychiatric facility in the capital city of the United Arab Emirates, there was a 20-30% drop in the total number of outpatient visits, and an 80% drop-in new appointment visits in the early months of the pandemic 29. At a public health service specifically dedicated to vulnerable groups in Italy, there was nearly a 35% drop in the number of mental health outpatient visits in March 2020 (i.e., lockdown period in Italy) in contrast to the number of visits in March 2019 30. On the other hand, during the COVID-19 pandemic surge in Massachusetts (USA), there was a 9.1% increment in the number of outpatient visits for mental health/substance use disorders relative to the pre-pandemic period 31.
Anxiety and depressive disorders represent most psychiatric outpatient visits in Peru. This is consistent with the fact that such disorders are the mental diseases with the highest twelve-month prevalence in the general population of Peru and South America 32. This could also be explained by the fact that people with anxiety/depressive disorders often require regular appointments, especially in early months of their treatment. It should be noted that the COVID-19 pandemic could have affected the prevalence of psychiatric disorders as well. A population-based study in Peru showed an increase in the prevalence of anxiety and affective disorders after the COVID-19 lockdown, which could explain in part our findings regarding the increase of the number of psychiatric outpatient visits after May 2020 33,34.
Strengths and limitations
The information about the frequency of different outpatient groups of psychiatric disorders at the national and subnational level in Peru, obtained from a careful examination of a nationwide registry is useful for clinicians and public health authorities in Peru and Latin America. Nonetheless, this study also has some limitations. First, although the registry has national coverage, there could be an under-representation of psychiatric visits in the outpatient setting because of two reasons: a) As the registry herein analysed aggregates monthly visits reported by every HCFs in Peru, it is possible that some HCFs may have not reported any data, or they are delayed in reporting their estimates; and b) There could have been errors during the data entry or ICD-10 codification. As the data we used only register one diagnosis for each individual attention, and diagnosis could be adjusted to treatment, there could be underreporting of other, comorbid psychiatric diagnoses. Because of this, the absolute number of psychiatric visits could be higher and therefore, the results may show a conservative scenario. Conversely, data entry errors could have also inflated such results if non-psychiatric diagnoses were coded as psychiatric disorders.
Second, other covariates to describe the psychiatric outpatient visits were lacking; this limitation is inherent to the outpatient registry. For example, had we known the mode of visit method (in-person vs. telemedicine), we could have estimated what proportion of all psychiatric outpatient visits was performed using telemedicine, a feature that could have been useful to describe how Peruvian HCFs changed their method of delivering outpatient visits during the pandemic (i.e., using more telemedicine).
CONCLUSION
Psychiatric disorders represent a small fraction of the outpatient visits in Peru, out of which anxiety and depressive disorders remain the most frequent, especially across working age groups. Mental health policies from national and subnational organizations in Peru are needed to tackle the psychiatric outpatient burden, considering demographic and subnational differences, monthly trends, and the impact of the COVID-19 pandemic.
ETHICS
This analysis used open-access data that do not contain personal identifiers. Therefore, we did not seek approval by an Ethics Committee and consent was not required. The opinions presented in this work are those of the authors alone, and do not necessarily represent those of the institutions to which they belong. The authors are collectively responsible for the accuracy of the findings presented.