Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Medica Herediana
versión impresa ISSN 1018-130Xversión On-line ISSN 1729-214X
Rev Med Hered v.21 n.4 Lima oct./dic. 2010
Perceived quality of life comparison between medical graduates from Peru who migrated and those who stayed in their home country.
Comparación de la calidad de vida entre médicos graduados en el Perú que migraron al extranjero y los que permanecieron en el país.
Luis R Leon Jr.1,2,3, Herminio Ojeda1, Christopher S Wendel 3, Christine Renee Leon, Hugo Villar1, Shemuel Benn Psalms3.
1
University of Arizona Health Science Center, Tucson, Arizona, USA.2
Tucson Medical Center and Agave Surgical Associates, PC. Tucson, Arizona, USA.3
Southern Arizona Veteran Affairs Health Care System. Tucson, Arizona, USA.
RESUMEN
Objetivo: Comparar la calidad de vida (CDV) de los egresados de una Escuela de Medicina peruana que migraron al extranjero y de los que permanecieron en el país. Material y método: Se utilizó un cuestionario basado en una combinación de dos herramientas para medir la CDV de proveedores de salud previamente validadas, para evaluar auto-satisfacción (grupo A), las relaciones interpersonales y sociales (grupo B) y los niveles de satisfacción personal (grupo C). Es cuestionario se envió por correo electrónico a los graduados de la Universidad Peruana Cayetano Heredia. Resultados: La tasa de respuesta fue 35%. Los niveles de ingreso económico fueron significativamente menores en los médicos que permanecieron en el Perú en comparación con los que migraron. En muy pocas preguntas se encontró diferencia significativa. En el grupo A, los médicos que migraron percibieron una CDV significativamente mayor solo en la expectativa de futuro. En el grupo B, esto se alcanzó diferencias sólo en el grado de apoyo y el nivel de conflicto entre colegas , y en el grupo C, en el nivel de información recibida acerca de los resultados de su trabajo ("feedback"), el esfuerzo físico del trabajo diario (estrés físico), las oportunidades de expresar lo que se piensa y necesita, el esfuerzo del hospital para mejorar la CDV de sus trabajadores, el entrenamiento necesario para realizar el trabajo diario, y la variedad en el trabajo. Los médicos que migraron percibieron una mayor aceptación en la profesión, en la sociedad en general y dentro de la comunidad donde viven. De manera significativa más médicos que migraron no tenían intenciones de cambiar sus niveles actuales de vida. Conclusiones: La CDV percibida de los médicos estudiados fue similar en la mayoría de preguntas examinadas entre ambos grupos, a pesar de la marcada diferencia encontrada en los niveles de ingreso económico. La migración medica teniendo el Perú como procedencia parece ser un factor favorable en el logro de una adaptación exitosa a una nueva cultura. (Rev Med Hered 2010;21:187-196).
PALABRAS CLAVE: Médicos graduados, calidad de vida, educación médica, fuga de talentos, migración.
SUMMARY
Objective: To compare the quality of life (QOL) of the graduated from a Peruvian medical school who migrated abroad and those who remained in the country. We also intended to address the level of integration of Peruvian international medical graduates (IMGs) into the United States (US). Material and methods: A combination of two previously validated tools designed to measure QOL of health care practitioners (HCPs) was used to create a survey, including questions that analyzed self-satisfaction (group A), interpersonal/social relationships (Group B) and professional satisfaction (Group C), which was e-mailed to graduates from a Peruvian Medical School. Results: The response rate was 35%. Income levels were significantly lower for HCPs practicing in Peru than those practicing abroad. Very few question items reached statistical significant differences between groups. In group A, IMGs who migrated perceived a significantly higher QOL only in the perception of their future. In group B, was achieved only in the peer support and the conflict level with coworkers categories. In group C, only in the work feedback, job physical discomfort, expression opportunities, hospital attempts to improve the QOL of their position, necessary training for job performance and work variety categories. However, of 41/44 items showed a better (more satisfied) response from the abroad group, of which 13 achieve statistical significance (8 at the 1% level). IMGs practicing abroad perceived a high acceptance into the foreign profession, society and living community. Significantly most IMGs do not intend to change their current status. Conclusions: Very few significant differences were noted in the perceived QOL of physicians between groups, in spite of a marked income discrepancy. However, there was a clear trend for dissatisfaction in the Peru group on several important items that, without reaching statistical significance, may indicate the adverse effect of Peruvian conditions on physicians level of satisfaction in their country. Further studies with larger samples are needed to confirm our findings. Migration from Peru as a physician seems favorable in achieving successful adaptation to a new culture. (Rev Med Hered 2010;21:187-196).
KEY WORDS: International medical graduates, quality of life, graduate medical education, brain drain.
INTRODUCTION
Many international medical graduates (IMGs) try to enter graduate medical education (GME) in the United States (US), hoping to obtain excellence in medical training and better living conditions. This process is difficult, costly and time consuming (1). Furthermore; migrants suffer complex psychosocial changes with long-lasting effects on their identity (2).
Leaving ones country involves important losses, such as familiar food, friends, music, customs, loss of self-identity and even ones language. The new nation offers unusual food, songs, political concerns and language, situation also known as cultural shock. There is an expected mourning over these losses. Both loss and mourning challenge the stability of the immigrants psyche. Anecdotal experience suggests that many IMGs also experience burnout, depression, and work dissatisfaction. It is often said that Health Care Providers (HCPs) that migrate face issues such as idealization, closeness and distance, hope and nostalgia, or linguistic transformation now take a big role in shaping their lives and in their perceived quality of life (QOL) (2).
The presence of IMGs in the US is to say the least, controversial. There are several critics of their presence. For instance, the social and interpersonal challenges that IMGs face in providing care to patients in the US have been described. It has been said that many of them may have problems understanding colloquial speech, patient dialects, body language and speech inflection (3). The depth of their undergraduate education has been placed in doubt, as far as the importance given to communication skills in their schools curricula. It has also been stated that IMGs may find it difficult to establish rapport with patients who do not share their appearance or cultural background. In addition, it is thought that fear of rejection or being singled out may cause IMGs to appear more aloof in their interactions with patients, or to insist more unyieldingly on their authority as doctors. Lastly, concerns regarding IMGs and specific health-related beliefs of patients that may reduce patients compliance have been raised (3). These criticisms greatly add to the already-heavy emotional burden associated with migration.
It has been estimated that by 2010 in the US, almost half of all new workers will be individuals traditionally classified as minorities and by the year 2040, ethnic minorities will represent >50% of its population (4). It has been also well documented that 1 out of 4 physicians in the US are IMGs (5).
The effect of the migration process on both the donor and recipient countries has been extensively documented (5). However, the effect of the same process on the migrant him/herself has not been previously studied in terms of QOL. There is no documentation as to whether the perceived QOL of the migrant, in relation to greater career fulfillment, social and interpersonal affairs and self-satisfaction, is better than those physicians who decided to stay in their countries of origin.
The World Health Organization defines QOL as "individuals perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns"(6). This study aimed to evaluate the QOL of HCPs that graduated from a medical school in Peru, comparing the QOL of IMGs who migrated abroad to that of those who remained in their country. A second objective was to attend to the level of integration of Peruvian IMGs into the US society.
MATERIAL AND METHODS
Population
An initial contact with a Peruvian medical school, the Universidad Peruana Cayetano Heredia (UPCH), was made in order to obtain a list of electronic mails (e-mail) of all graduates from 1990 until 2005. This list was also supplemented with information obtained from personal and peer records. This medical school enrolls about 120 students per class every year, and on average 50% of them successfully graduate. From those, about 30% migrate every year, with small variations. It was in this manner that we collected 211 e-mails addresses all together. The study was conceived in December 2006 and the collection of data finished by July 2007.
Survey Instrument
A combination of two previously validated research tools designed to measure QOL of HCPs: the Brief Life Satisfaction Scale (BLSS)(7) and the Professional Quality of Life (QPL-35) (8) questionnaires, was created. The survey was translated into Spanish for its accurate application. Both tools have been shown to be easy to apply, obtaining adequate measurements of QOL in the work environment. Their strong reliability and validity has also been previously documented (7,8).
The BLSS is a 10-item measure, which begins: "Using the following 5-point scale, indicate how satisfied you are with each of the following areas:" Points on this scale are: The authors note that depending on the researchers specific areas of interest, a few additional items (areas) could be added. Because our interest was to broaden the scope of QOL evaluation to include other measurable outcomes, additional items were added. The BLSS tool was combined with the QPL-35, from which most of the proposed questions were taken. This tool consists of 35 questions that are answered on a scale from 1-10 on perceived professional QOL, where 10 is the best rate. These scores are then grouped for analysis into the following categories: "very low" (values 1-2), "low" (3-5), "high" (6-8), and "highest" (9-10), which corresponds well to the five satisfaction levels in the BLSS. Three main domains encompass all questions: "supervisor support", "work load" and "intrinsic motivation". Two questions are not able to be grouped by those domains, and they refer to the measurement of the perceived professional QOL and to the ability to "disconnect" from job pressures at the end of the work day.
Our two-page questionnaire included 48 questions, mostly taken from the QPL-35, that are answered with the 1-5 scale taken from BLSS, 1) very dissatisfied, 2) dissatisfied, 3) neither satisfied nor dissatisfied, 4) satisfied, and 5) very satisfied according to the satisfaction level felt to the questions posed. These questions fall into three domains: self-satisfaction (self, achievement, health, future); interpersonal/social relationships (family, friends, home); and professional role satisfaction (work setting, work relations).
The questionnaire was e-mailed to all these HCPs. In an attempt to boost our response rate, two additional e-mail notifications were sent for initial non-responders, approximately two weeks after the first one. E-mail was used primarily; however, phone calling was used when necessary for the HCPs whom we had their phone numbers available.
Completed questionnaires were centrally collected. A written promise of confidentiality of the data was guaranteed to all IMGs and no financial remuneration was offered; their responses were completely voluntary.
Statistical analysis
Data was entered into a Microsoft Excel® database and analyzed using Stata® version 8.2 (StataCorp LP, College Station, Texas). Descriptive statistics were used to analyze the HCP demographic features, practices characteristics and their responses. Differences between groups were analyzed using the c2 test for categorical variables and the Students t-test for continuous variables. Satisfaction responses were treated as a categorical variable. For tabulations where all cells contained >5 responses, the Pearson c2 p-value was used (which only applied to questionnaire items 25 and 28). For all others, in which at least 1 cell contained <5 responses, the Fishers exact p-value was used. The responses were analyzed by grouping very dissatisfied + dissatisfied as a single group; satisfied + very satisfied as another group; and neither satisfied or dissatisfied as the last group. To facilitate the analysis, answers were divided in: self-satisfaction area, which incorporated questions 1, 3, 4, 10, 28, 39, 42 and 43; interpersonal/social relationship area, including 5-8, 21, 22, 27, 34 and 46-48; and professional role satisfaction area, counting 2, 9, 11-20, 23-26, 29-33, 35-38, 40, 41, 44 and 45.
RESULTS
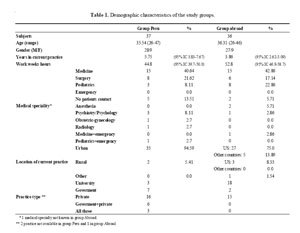
A total of 211 e-mails were obtained, and 73 questionnaire responses were received, for a response rate of 34.6%. Demographic data, including age, gender and practice environment (type and location of their current practices, medical specialty, and years in their current work, weekly work-hours and yearly income) was recorded. The demographic features in both groups are shown in table 1.
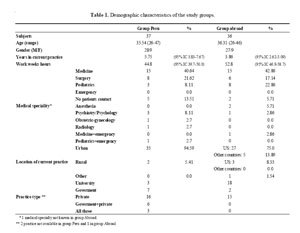
There were six physicians (16.2%) who, after obtaining GME, returned to Peru to establish their practices and are included with others who practice in their country for analysis. No significant differences were found in age (p= 0.5), gender (p=0.95) or years in current practice (p= 0.1) between groups. As a whole, the survey respondents have been in practice only a mean of 4.8 years (95% confidence intervals [CI] 3.7- 6). IMGs who migrated reported significantly more hours at work (p=0.04) and a higher income (p<0.001) than those who practice in Peru. Financial disclosure was obtained in 71 out of 73 responders (97.3%). The average yearly income for HCPs practicing in Peru was US$ 28,386 (95% CI 19,502-37,271), whereas for HCPs practicing abroad was US$ 173,344 (95% CI 129,070-217,619).
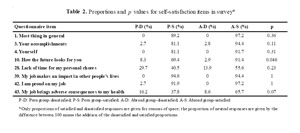
Self-satisfaction (
Table 2)IMGs who migrated perceived a significantly higher QOL in what the future brings, which was the only category that reached statistical significance.
Interpersonal/social relationships
(Table 3)The QOL for IMGs was only perceived significantly superior in the peer support and the conflict level with co-workers categories.
The last three questionnaire items were also related to social issues and only applicable to IMGs practicing abroad. They scored high as far as their perceived acceptance into the foreign medical profession (mean score 4.42; standard deviation [SD] 0.55), the foreign society (mean score 4.3; SD 0.79) and into their new living community (mean score 4.6; SD 0.56).
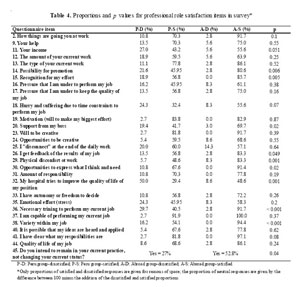
Professional role satisfaction (
Table 4)The QOL for IMGs was perceived significantly superior in the following: feedback from their job, physical discomfort at work, opportunities for expression, hospital attempts to improve the QOL of their position, necessary training to perform their job and work variety. Significantly most IMGs intend to remain in their current practice, not changing their current status.
DISCUSSION
Most of the HCPs surveyed migrated during the decades 1980-2000 and a brief description of the political context may be of relevance to better understand a reality, which is common in many developing countries that supply physicians to the US. In 1980, democracy was established in Peru (9).The social turmoil resulted in about 69,000 people killed during the 1980 to the early 1990s period (9). Economic crisis was profound, terrorism was at its peak and corruption was widespread. By 1995, most of the terrorist groups had been defeated and economic stability arrived with relative national bonanza but with an extremely limited job market especially for physicians. However since the year 2000, Peru has had one of the best performing economies in Latin America, largely attributable to growth in the mining and export sectors (10,11). Yet there still are signs of discontent, manifest for instance in social protests and high emigration rates. The top 1% of families commands one third of the national income, while the bottom third receives only 5% (12,13). Poverty affects 52% (under $58/month) and extreme poverty 19% (under $32/month) of its population. Underemployment levels total 64.5%(11). Middle class, from where many of Peruvian physicians derived from is relatively inexistent, when compared to the US middle class.
Is in the above historical context that 5,000 doctors graduated in Peru between 1995 and 2005 In the same time frame, a net increase of only 1200 physicians was seen. In 1992, 4,416 physicians migrated increasing to 14,130 by 2004 (14).There is as yet no downward trend in the population living in absolute poverty. In 1998, Peru had 24800,768 habitants and 30,529 registered physicians, yielding a rate of 1 physician/813 habitants. This is a misleading ratio given the severe misdistribution of physicians in the Peruvian territory, concentrated in the capital and lacking in the rural areas (15).
The UPCH is an autonomous, private, non-profit institution created in 1961, dedicated to academic and social service activities. In 1965, the Johns Hopkins University established a program to benefit the UPCH, after a careful study of the main Faculties of Medicine in Latin America was performed led by their Chairman, Dr. Turner. Faculty exchange programs, study and organization plans and scholarships for graduates from the UPCH were established (16).
We felt that neither one of the pre-existing survey tools for measuring QOL by themselves was perfectly applicable in order to achieve our research goals. They do not include features peculiar to a physician who migrates and all issues related to this phenomenon. The BLSS was designed to provide useful information while being concise enough to be included with other instruments. The scale system to answer the proposed questions was taken from this first tool, whereas most of the questions were obtained from the QPL-35. We analyzed the data by grouping choices 1 + 2 as one option, and 4 + 5 as another one, keeping choice 3 unchanged. We feel that the differences between choices 1 and 2, or 4 and 5 are so subtle that, statistically significant differences between those data points may not translate into real-life, QOL differences. Surveyed subjects were not asked to just select among three choices only rather than five in order to keep the modifications to the combined tool as little as possible. In fact, the analysis of the QPL-35 results entitles grouping some of the scale points identically to our analysis, for the reason exposed above.
There is a wide variation in the reported survey response rates, particularly among physicians, typically ranging from 29 to 74% (17-22). The response to our survey was therefore with the expected range, but was somewhat disappointing given the fact that this indirectly reflects the interest of the responder. Time constraints or lack of incentives for completion of the questionnaire may have played a role (19,23). However, the response rate to the question of income in the surveys was surprisingly high, given that financial disclosure is often not easy to obtain. The fact that the survey was e-mailed may have limited the access only to those who have internet access, restricted only the graduation classes from 1980 and after. Also all were part of a single University in the private sector located in an urban geographic area.
Both groups matched well in terms of age, gender and years of practice. The latter however, shows that both groups of HCPs are in an early stage of their professional career. A mean of 4.8 years for years in practice for the entire group indicates that most of the respondents are in an earlier stage of their professional career, which means that our results do not necessarily reflect their ultimate QOL. The significant differences in the number of weekly hours at work may be related to the same issue. The average workweek for some surgical specialties in the US is about 42 hours per week, which correlates with our results for the Peru group, but is significantly less than HCPs in the Abroad group. An explanation may be that some of the respondents abroad were still undergoing GME, and as it is widely known, they typically work long hours, now limited to 80 hours per week in the US. The difference may be a reflection of more people in the Abroad group undergoing training. This cannot be proven as it was not ascertained by our study. Our results apply only for physicians working mostly in urban areas, in both the US and Peru. The practice type of respondents in Peru seemed to favor the private setting (45.7%), whereas IMGs mostly practice in a University setting (51.4%). Most respondents in both groups practice non-surgical specialties (about 80% of them as a whole). Our anecdotal experience suggests that this is an underestimation, which is likely due to a population selection bias. In the UPCH, this figure should be around 5% for the surgical specialty.
Our results reflect an abysmal difference in wages. Our survey however, did not differentiate global or net salary, before or after taxes or included extra-salary income. Nevertheless, when considered in the context of costs of living differences between Peru and the US or Canada, there is a gross mismatch. To some peoples surprise, we could not identify significant differences in the perceived QOL with respect to income. However, our findings are not totally surprising. More earnings do not necessarily translate into greater financial satisfaction, in the situation of higher expense bills or considerable debt to pay as a consequence of residing in a nation with comparative elevated cost of living. It is also important to consider that the p value obtained with regard to satisfaction with salaries in Peru and abroad did not reach statistical significance for very little (p= 0.051), and this could be easily the reflection of a type 2 error.
Our results show that IMGs who migrated have adjusted reasonably well to their new environment. HCPs in both groups seem to be equally satisfied with their perception of self-satisfaction. Our study revealed that the future for HCPs that migrated is perceived significantly "brighter" than for those who stayed, as the only meaningful difference. This may indicate the reflection of a better professional outlook, as it was shown in the analysis of items questioning on professional satisfaction (Table 4). Better possibilities for professional promotion and to be heard, less physical discomfort in the work environment, higher levels of feedback and recognition for the daily professional effort, higher perceived supervisor and hospital support, can all translate into higher perceived outlooks.
Our results support the notion that the impact of cultural issues over the QOL of IMGs is not as negative as some may imagine. The high scores as far as their perceived acceptance into the foreign medical profession, the new society and into their novel living community speak of a high adaptation level and also of a positive attitude of the US medical and living community to the arrival of a foreigner. The perceived higher degrees of peer support and lower conflict levels with coworkers in the abroad group further support our hypothesis.
Most of the significant differences have been found in this area, in favor of IMGs who migrated. We believe that this is well summarized by the responses obtained to one question, the one referring to the HCPs intention to change their current status. The fact that most IMGs significantly intend to remain in their current practices indicates a higher satisfaction level with the foreign working conditions. As no differences were identified in salary satisfaction, the job environment itself has to be an important explanation for this difference.
A likely explanation for this disparity maybe related to the major challenges posed by migrating to a new working environment, which for some, can be fuel for a full development of their scientific potential (24). Our results appear to indicate that the working environment in Peru does not offer enough professional encouragement, translated into less feedback or recognition for daily endeavors, less perceived supervisor and hospital support, and fewer possibilities for professional promotion or self-expression. Of the 44 items that were included in the survey tool, 41 show a better (more satisfied) response from the abroad group, of which 13 achieve statistical significance (8 at the 1% level). It seems reasonable to conclude that there is a great level of discontent in the Peru group on several important items. This conclusion however, should be carefully analyzed, always tempered by doubts over sample representativeness or over the effects of the response rates obtained by our study, as we have indicated in the Limitations section of our manuscript. Further studies with larger samples are needed to confirm our findings.
Our study reflected that about 84% of HCPs who migrated, did not return to Peru to practice. While being true that the vast majority permanently migrates, we believe that the real figure is even greater. Most IMGs like to believe that they made a conscious choice to leave Peru. Some may argue that they however, had no choice to practice in their country due to financial or safety reasons and that, in the search for better professional and personal prospects, the only suitable alternative was to emigrate. For most IMGs that successfully complete GME abroad, the choice to return to Peru is clearer and yet, most do not. The majority of IMGs migrate in their late 20s, when the stress level can be considered intermediate and when probably most people have achieved a reasonable capacity for separateness. The reasons for leaving ones country also play a role. Financial hardship or political persecution can be reasons for failure in adaptation.2 While the latter has little to none application in our cohort, financial hardship represents a prevalent reason to migrate. Other important reasons include better outlooks for financial and professional progress, and not necessarily hardship. This was not inquired by our survey and therefore remains hypothetical. The varying emotions with which the host culture receives the migrant, in which the immigrants race may play a strong role(2). The extent of cultural differences between the adopted and the home country is important. Moving from England or Canada to the US is clearly not the same as one from Yemen or Peru (2). The extent to which ones original professional role can be resumed upon immigration is key. Maintaining this role assures an "inner continuity in change"(2). Our results indicate that most IMGs continue to practice Medicine in its different specialties. However, a sizeable number do not currently have patients contact, about 10% of HCPs overall and 8.7% in the group abroad. This may have an important impact in the overall ability of the group to adjust to a new reality.
Even though very few statistically significant differences were noted in the perceived QOL of physicians between groups, there was a clear trend for dissatisfaction in the Peru group on several important items that, without reaching statistical significance, may indicate the adverse effect of Peruvian conditions on physicians level of satisfaction in their country.
After examining each of the factors described above, migration as a physician seems to have favorable conditions to achieve successful adaptation to the new culture.
Our study has some limitations. The first resides in that the survey tool used is a combination of two validated surveys. Our approach is the first one to measure the perceived physician wellbeing in relation to their migratory status and by simply combining two validated tools; the modifications were kept to a minimum. Second, the extent to which this tool accurately reflects the perceived QOL cannot be determined. It measures several factors in graduates of a single medical school in one country over a limited period of time. We have measured QOL at a defined survey points, but a different perception of QOL could occur between survey time points. Also, the negative view of the Peruvian that graduated in the midst of the 1990 economic and political crisis may have changed.. Responders work mostly in the urban setting but in very different clinical settings and practices, suggesting they are only likely to be representative of similar situations from other countries.
Another important issue is that our sample possibly does not represent with fidelity the perception of HCPs from the UPCH. As stated previously, from a universe of about 900 graduates (60 per year) in the 15 years of the study, we only collected e-mails from 211 and questionnaire data from 73, which corresponds to less than 10% in both groups (migrants and non-migrants). It is always possible that this small sample is affected by a selection bias. Differences may exist in those who had e-mails vs. those who do not. This information remains unknown at this time. Our findings however, match findings that we anecdotically expected prior to the execution of this study. A higher response rate and a more exhaustive attempt to contact more people from the same medical school, possible using alternative ways for contact (regular mail, phone calls, and fax numbers) may help in increasing representativeness of the sample.
Our survey response rates were in the low end of those reported for other physician surveys, suggesting that our results may vary with higher response rates (potential type II error).
Finally, the models reported in this study evaluate each QOL variable individually. Because of multicollinearity between QOL variables, we have limited ability to separate the effects of individual variables from one another. Because of these issues, our results are best interpreted as general associations
Acknowledgements
All authors deny any conflict of interests. No funding was required for this work. The main author (Luis R Leon) had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
1. Leon LR, Psalms SB, Leon CR, Arana G, Villar H. The journey of a foreign trained physician to a US residency. J Am Coll Surg 2007; 204: 486-494. [ Links ]
2. Akhtar S. A third individuation: immigration, identity, and the psychoanalytic process. J Amer Psychoanal Assn 1995; 43:1051-1084. [ Links ]
3. Fiscella K, Frankel R. Overcoming cultural barriers: International Medical Graduates in the United States. JAMA 2000; 283:1751. [ Links ]
4. Spanish Translation Services. Dynamic Demographics. In: http://spanishsts.net/fastfacts.htm (Access date: April 18, 2010). [ Links ] 5. Mullan F. The metrics of the physician brain drain. N Engl J Med 2005; 353:1810–1818. [ Links ] 6. World Health Organization. Division of Mental Health and Prevention of Substance Abuse. WHOQOL-Measuring quality of life. WHO/MS A/MNH/PSF 97.4. In: 7. Lubin B, Van Whitlock R. Psychometric properties of the Brief Life Satisfaction Scales. J Clin Psychol 2004; 60:11-27. [ Links ] 8. Martin J, Cortes JA, Morente M, Caboblanco M, Garijo J, Rodriguez A. Metric characteristics of the Professional Quality of Life Questionnaire [QPL-35] in primary care professionals. Gac Sanit 2004; 18:129-136. [ Links ] 9. Infoplease. Peru. In : 10.Infoplease. U.S. Department of State Background Note. Peru. In: 11.Central Reserved Bank of Peru. Annual Report 2002. In : 12.Wright K, Altamirano T, Copestake J, Figueroa A. Poverty studies in Peru: towards a more inclusive study of exclusion. Special issue of global social policy 4.3. Bath, UK: Wellbeing in Developing Countries ESRC Research Group; 2004. p.1-41. [ Links ] 13.Webb RC. Government policy and the distribution of income in Peru, 1963-1973. Harvard: Harvard University Press; 1977.p. 239. [ Links ] 14.Fraser B. Human resources for health in the Americas. Lancet 2007; 369:179-180. [ Links ] 15.Berrios J. La creación de Facultades de Medicina en el Perú-1998. Rev Med Hered 1998; 9:95-97. [ Links ] 16.Porturas F. Origen de la Universidad Peruana Cayetano Heredia. Rev Med Hered 1998; 9:95-97. [ Links ] 17.Rastel D, Perrin M, Guidicelli H. Compressive therapy after varicose vein surgery: results of a French national inquiry. Mal Vasc 2004; 29:27-34. [ Links ] 18.Pillny M, Luther B, Muller BT, Sandmann W. Survey of therapy of deep venous thrombosis among members of the German Society of Vascular Surgery. Chirurg 2002; 73:180-184. [ Links ] 19.McDermott MM, Greenland P, Hahn EA, et al. The effects of continuing medical education credits on physician response rates to a mailed questionnaire. Health Mark Q 2003; 20:27-42. [ Links ] 20.Caprini JA, Arcelus JI, Hoffman K, et al. Prevention of venous thromboembolism in North America: results of a survey among general surgeons. J Vasc Surg 1994; 20:751-758. [ Links ] 21.Wijesinghe LD, Gamage L, Berridge DC, Scott DJ. Measuring serum total cholesterol: do vascular surgeons know what they are doing? Ann R Coll Surg Engl 1999; 81:32-36. [ Links ] 22.Basnyat PS, Moseley LG, al-Rawi M, Galland RB, Lewis MH. Smoking-do vascular surgeons practice what they preach? Ann R Coll Surg Engl 2000; 82:424-427. [ Links ] 23.Leung GM, Ho LM, Chan MF, Johnston JM, Wong FK. The effects of cash and lottery incentives on mailed surveys to physicians: a randomized trial. J Clin Epidemiol 2002; 5:801-807. [ Links ] 24.Stepansky PE. The memoirs of Margaret S. Mahler. New York: Free Press; 1988.p. 179. [ Links ] Correspondence: Luis R Leon Jr., MD, RVT, FACS Department of Vascular and Endovascular Surgery 5240 East Knight Drive. Suite # 118 Tucson, AZ 85712 Phone: 520-320-5665 Fax: 520-320-1779 e-mail:














