INTRODUCTION
Stroke is a leading cause of death and disability worldwide and the fifth cause in the United States of America 1,2. Of all supratentorial cerebrovascular diseases, the malignant infarction of the middle cerebral artery (MCA) can occur in 1 - 10% of the cases. Clinical presentation includes neurological deterioration, progressive neurological deficit, cerebral edema and herniation which can be seen in an ischemic lesion with an arterial territory comprise > 50% with a mortality that can reach 80% 3-7.
Decompressive craniectomy (DC) as part of the treatment for malignant infarction of the MCA continues to be controversial nowadays despite multiple randomized controlled trials showed favorable mortality outcomes but with paradoxical outcomes regarding long-term functional status (modified Rankin score > 3) 8-10.
Therefore, our study aimed to describe clinical, surgical and post-operative characteristics of patients with malignant MCA infarction who underwent DC and assess post-operative outcomes.
METHODS
Observational, descriptive, retrospective study, type case series, carried out between March 2017 and March 2020. Consecutive patients with the diagnosis of malignant stroke of the MCA who underwent DC at the Hospital José Casimiro Ulloa were reviewed. Inclusion criteria included patients with MCA infarction with midline shift and clinical deterioration (Glasgow Coma Scale ( 8).
Demographics and clinical characteristics included age, sex, past medical history, Glasgow and modified Rankin Scale at admission, the presence of anisocoria, motor deficit, blood pressure at admission and time to surgery since diagnosis were evaluated.
The diagnosis of MCA infarction was made based on brain CT images: a hypodensity in the MCA territory with midline shift was assessed by the radiologist, neurologist or neurosurgeon. MRI and CT perfusion were not employed in our institution. In cases of hemorrhagic transformation, the presence of blood within the hypodensity and clinical presentation were assessed. The surgical decision was made by clinical deterioration and if the territory of the MCA infarction was ( 50%.
DC was done based on previous technical principles. A question mark incision was made in the affected side, the skull flap was removed, the dura was opened and then duroplasty was performed. The bone flap was kept in the abdominal subcutaneous tissue. Time of surgery, blood loss and mortality were analyzed.
The study was exempted from the institutional board review due to the retrospective design and review of clinical charts.
RESULTS
Patient characteristics
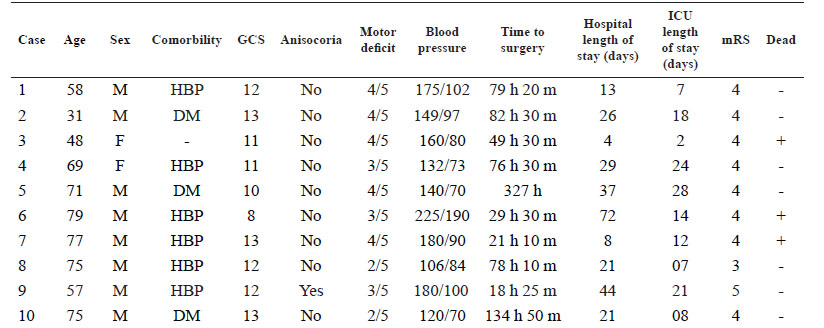
Ten patients were retrospectively reviewed. Eight patients were men. The mean age was 64 ± 15.4 years (range 31 to 79 years); six cases were older than 60 years. The mean Glasgow Coma Scale at the moment of the diagnosis was 11 points (range 8 to 13 points). Anisocoria and motor deficit were present in one and ten patients, respectively. The mean systolic pressure was 156.7 mmHg and the mean diastolic pressure was 95.6 mmHg at the time of the diagnosis. The mean time from diagnosis of stroke to surgery was 89.7 hours. The mean preoperative modified Rankin score was 4. All the patients had right dominance. Overall characteristics of the patients are shown in Table 1.
Stroke characteristics
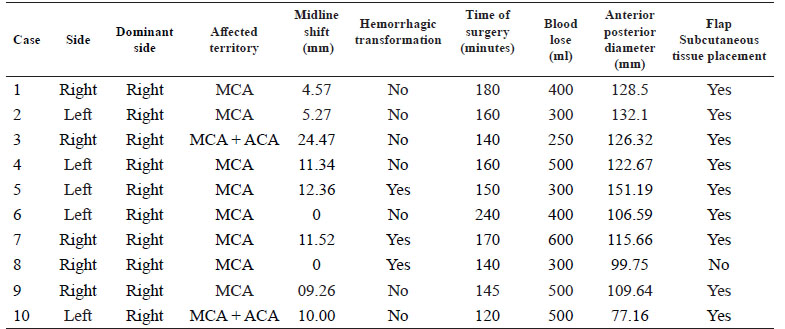
The left middle cerebral artery was affected in 50% of the cases. In all cases the MCA was affected and in two cases the anterior cerebral artery was also comprised. Midline shift was present in eight cases with a mean shift of 8.9 mm. Three patients had a hemorrhagic transformation of the stroke. An illustrative case is shown in figure 1. Radiological characteristics are shown in table 2.
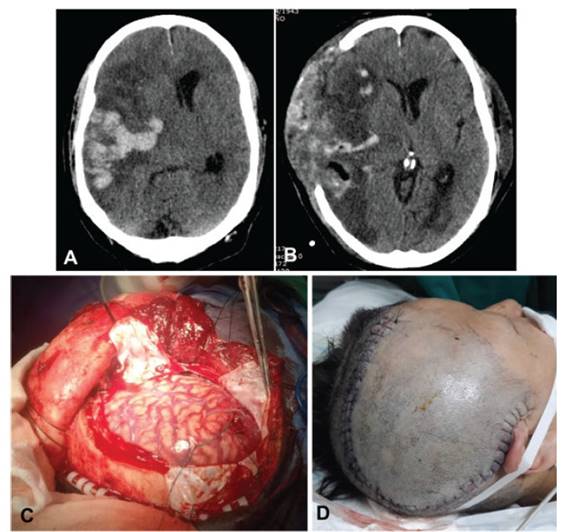
Figure 1 A: Brain CT scan shows a malignant infarction of the right middle cerebral artery with hemorrhagic transformation. B: Brain CT scan following decompressive craniectomy 72 hours after hospital admission. C-D: Intraoperative dura opening and post-operative skin incision.
Surgical characteristics, post-operative evolution and complications
DC was done in the left side in 50% of the cases. The mean anterior-posterior diameter of the bone flap was 116 mm ( 20.3 mm (range 77.2 mm to 151.2 mm). The average time of surgery was 151.5 minutes and the mean blood loss was 405 ml. In nine patients the skull flap was kept in the abdominal subcutaneous tissue. The mean ICU length of stay was 14.1 days (range 2 to 28 days). The mean hospital length of stay was 27.5 days (range 4 to 72 days). No patient improved clinically at discharge. Three patients died (30%), of which two of them were older than 60 years.
DISCUSSION
According to our results, the in-hospital mortality rate after performing DC in patients with malignant MCA infarction was 30% and time to surgery since the initial diagnosis of stroke was 89.7 hours. DC is a life-saving neurosurgical procedure used in cases of increased intracranial pressure due malignant infarction of the MCA. Previous papers have shown the benefits of this procedure in mortality but not in functional recovery.
Three controlled randomized trials have evaluated the rationale of DC in cases of MCA strokes. The DESTINY trial evaluated 32 patients and determined a considerable mortality reduction in their analysis (88% of non-DC versus 47% of patients who underwent DC 8, the DECIMAL trial evaluated 38 patients with a survival rate favoring patients who underwent DC (75% versus 22%) 9, and the HAMLET trial evaluated 64 patients in which an ARR of 38% in mortality favored the DC-group 10.
Overall, these studies found that patients under 60 years had a lower mortality rate at 12 months when compared with medical management. In addition, Vahedi et al. 11, performed a pooled analysis of these three RCT and determined a considerable reduction in mortality (22% versus 71%), no improvement in the proportion of survivors with good outcomes and no difference in clinical outcomes among dominant and non-dominant hemispheres. On the other hand, DESTINY II trial evaluated patients older than 60 years and their results showed that survival without severe disability was higher in the DC-group in comparison to the control group (38% versus 18%). Although, overall mortality was lower in the DC-group (33% versus 70%) 12 .Other studies also shown poor outcomes in patients older than 60 years 13. Nevertheless, other authors reported better functional outcomes and lower mortality rates in this subgroup of patients 14,15.
In addition, the variable time to surgery since the initial diagnosis of stoke does not reflect the time elapsed from malignant stroke development to surgery.
In our country, few studies have evaluated in-hospital mortality rates due to cerebrovascular diseases. In a national hospital, the overall mortality rate was 19.6%, most of them within the first three days 16, whereas another study reported a mortality of 20.8% 17. Obviously, these studies did not evaluate mortality in patients with MCA occlusion who underwent DC. Conversely, they report a general overview of cerebrovascular diseases and set a landmark for future investigations in the cerebrovascular field. Despite these results, a recent paper reported a decreased tendency which was heterogeneous among locations within the same country 18. Previous studies reported that patients who underwent DC with larger bone flaps showed better outcomes 19-21. This is particularly special in traumatic brain injury cases 22,23. We found that our mean anterior-posterior diameter of the bone flap was 116 mm. Two patients who died had a skull flap less than 12 cm.
The study has several limitations: the small number of patients, the retrospective design and the lack of longer clinical follow-up are the most important. Our center is an emergency hospital where life-saving surgeries are performed and patients are therefore transferred to other centers or discharged home when they recover, making mid- and long-term clinical follow-up unviable.
DC is a life-saving procedure performed in an emergency-setting with an adequate in-hospital mortality rate despite time to diagnosis and age. Mid-term and long-term follow-ups are needed in this setting. Future directions should be established in order to improve the public services in developing countries in terms of neurosurgical care.