INTRODUCTION
The proximity of the maxillary sinuses to the roots of the upper molar teeth, mainly the upper first molar (UFM) or upper teeth 1, can affect the integrity of the sinus floor when inflammation, infection or odontogenic iatrogenic trauma are present, resulting in in-flammatory processes of the sinus membrane called odontogenic maxillary sinusitis (OMS) 2.
A recent article showed that 30 to 40% of the cases of chronic maxillary sinusitis were associated with the teeth 3. Among the main etiological factors that trigger and/or maintain the inflammatory/infectious processes are: caries, endo-antral syndrome, peri-odontal disease, iatrogenesis, oroantral fistula and odontogenic cysts. Pain, headache, face tenderness, nasal congestion and nasal secretion are among the symptoms most commonly reported by patients 4,5.
Although the symptoms are similar, OMS differ in its pathophysiology, microbiology, diagnosis and man-agement from other sinusitis 3. The diagnosis of OMS involves anamnesis and a physical examination of intraoral and extraoral anatomical structures as well as intraoral and extraoral radiographic images. Once intraoral and extraoral radiographic images are always necessary. Reconquered the etiology of OMS the plan of treatment involves a series of care that includes the elimination of dental etiological factors and antibiotic therapy to control infection 4.
This paper describe two case reports of odontogenic maxillary sinusitis (OMS), comparing the difference of the image details between the 2D x-ray images and the Cone Beam Computed Tomography (CBCT) and its relevance for OMS diagnosis and treatment plan.
Case 1
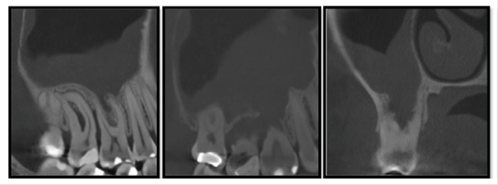
A 48-year-old white woman, described “pain in the left side of the face and in the left maxillary molars”, especially in the upper left first molar tooth. She was under treatment for type II diabetes mellitus and hypertension. The patient reported one month of nocturnal symptomatic episodes of pain and running nose. She also reported a cervical edema on the left side of the face and neck, exacerbated during movements of the head and neck. The medicine prescribed was continuous tramadol, but it wasn’t effective for pain control. An extraoral exam showed an inflammatory lymphadenopathy in the submandibular, ton-sillar, buccal and superficial left cervical lymph nodes chain on the left side. Pain was experienced during palpation without edema. The intraoral exam revealed a carious lesion in the left upper first molar with positive vertical percussion signs and pulp sensibility test compatible with irreversible pulpitis. The panoramic x-ray showed an extensive carious lesion in the upper left first molar with circumscribed bone rare-faction and defined limits, suggestive of a periapical cyst. The lesion involved the periapical region and alveolar extension of the maxillary sinus. For better evaluation of the relationship between the periapical lesion and the maxillary sinus, CBCT was done and showed a hypodense image in the periapical region of the left UFM with rupture of the cortical floor of the maxillary sinus, thick maxillary sinus mucosa, and expansion and rupture of the palatine cortical bone (figure 1). The diagnose was OMS associated with an infected radicular cyst the patient was referred for endodontic treatment.
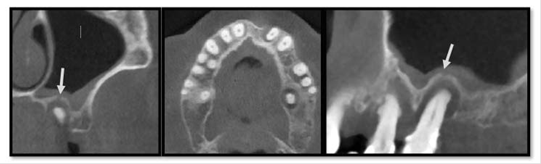
Figure 1 Case 1, coronal (A), axial (B) and sagittal (C) reformation of CBTC showed a hypodense image, cir-cumscribed in the periapical region of 26 and 27 teeth, promoting bugging cortical floor rupture of the adjacent maxillary sinus (arrow), thickening maxillary sinus mucosa, expansion and rupture of palatine cortical bone. Image was compatible with odontogenic maxillary sinusitis by root canal infection of 26 and 27 teeth.
Case 2
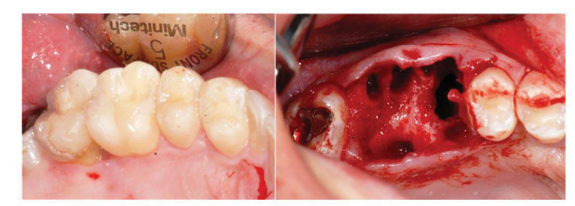
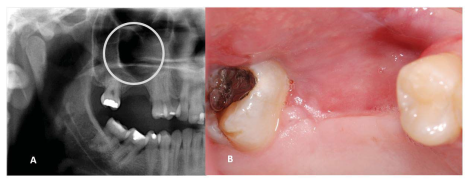
A 33-year-old man reported an episode of bleeding in the mouth and extravasation of fluid through the nose during liquid ingestion. The bleeding occurred in the upper right first molar region over one year, and there was extravasation of blood and serous fluid through the nose associated with pain and pressure on the same side of the face, when the patient was yawning. The medical condition did not show any comorbidity. In the intraoral exam, a 7mm periodontal pocket was detected. A gingival recession was also observed around the UFM and a Valsalva test was negative. The panoramic x-ray showed vertical bone loss in the super right first and second molar (URFSM) region. There was a bilateral alveolar ex-tension of maxillary sinus with opacification on the right maxillary sinus only (figure 2). We prescribed a CBCT exam, which showed severe furcation in-jury, external root reabsorption and vertical bone loss around cortical floor, and a thickening of the sinus mucosa around the URFSM. There was a rupture in the floor of the cortical sinus (figure 3). The diagnostic hypothesis was OMS related to periodontal disease or maxillary sinus tumor of the maxillary sinus floor. The extraction of the URFSM was done with curettage of the soft tissue associated with dental roots. In the surgical procedure, a 1cm diameter oroantral communication was observed, treated with intra alveolar fibrin sponge covered with a vestibular flap of oral mucosa (figure 4). The microscopic analysis showed no signs of malignancy and chronic inflammatory cell infiltrate compatible with inflammatory periodontal disease (figure 5). The final diagnosis was odontogenic maxillary sinusitis related to periodontal disease. A corticosteroid nasal spray was prescribed, and three months after the surgical procedure no clinical signs or symptoms were observed. A new panoramic x-ray six months after the surgical procedure showed normal radiopacity of the right maxillary sinus (figure 6).

Figure 2 Case 2, panoramic radiography showed bilateral alveolar extension of maxillary sinus, opacification of right maxillary sinus and vertical bone loss in the alveolar bone crest between 16 and 17 teeth (arrow).
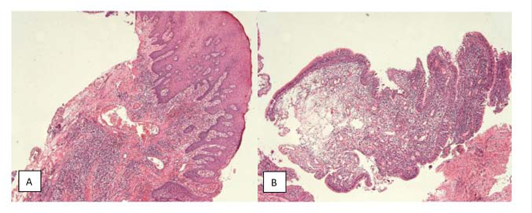
Figure 5 Case 2, image A shows hyperplastic parakeratinized epithelium with polymorphonuclear exocytosis. Conjunctive tissue with diffuse mononuclear inflammatory infiltrate, congestive blood vessels, hemorrhage region and bacterial colonization. Image B shows maxillary sinus mucosa with pseudostratified ciliated epithelium and mucosal cells with underlying mononuclear infiltrate, some congested blood vessels and edema.
DISCUSSION
The involvement of the maxillary sinus in inflammatory or infectious odontogenic processes occurs, mainly, through a generalized thickening (65.2%) and localized (24.8%) sinus mucosa preceded by maxillary sinusitis (6.4%) and a mucosal retention cyst (3.6%) 6. Thickening of the sinus mucosa is defined as when the thickness exceeds 1.0mm 7. The chances of occurrence are higher in men, with periodontal disease, moderate and severe bone loss. Periapical lesions near the maxillary sinus way are also reported 5. The majority of cases of sinusitis report a thickening of the sinus mucosa greater than 2.0 mm 6, and this value is an important indicator of maxillary sinusitis.
The chances of a maxillary sinus disease occur are 2.77 times higher when a dental root is in contact with the floor of the maxillary sinus 5. Anatomical factors contribute to the proximity between the tooth and the maxillary sinus, such as the alveolar find reported in both the above cases. Normal anatomic proximity between the maxillary molars and the maxillary sinus promotes a more intimate relations-hip between the maxillary sinus floor, the tooth and the buccal environment, especially in UFM 1.
The panoramic x-ray image is used to evaluation of the teeth, the maxillary sinus and their pneumatization. It also allows identification of the dental roots, the displacement of teeth and the presence of strange bodies inside. Despite this, because it is two-dimensional image, the panoramic image has limitations in the diagnosis of maxillary sinusitis, since the radiographic signs are not very specific 8. In both reported cases the panoramic x-ray could not evaluate the normal anatomic proximity between the maxillary molars and the maxillary sinus. Consequently, the proximity between the odontogenic infection and the maxillary sinus could not be seen.
The CBCT exam is thus indicated for a thorough inspection of the maxillary sinus and its relation to the teeth. It is also indicated for the evaluation of a patient with chronic persistent sinusitis 3, especially if it is unilateral or associated with anosmia and/or an unpleasant taste. It should also be included in the differential diagnosis of odontogenic sinusi-tis. In another study, 121 cases of OMS refractory to otorhinolaryngologic surgery were diagnosed. Through clinical odontological examination and the use of CBCT to locate the odontogenic factor, the method provided a definitive diagnosis and facilitated the development of a new plan of treatment 9.
OMS studies point to periodontal disease as one of the most important etiological factors, including caries, root canal infections and dental iatrogenics 9. In one of these studies 9, 35.6% of the cases involved sinus-buccal communication, treated during the intraoperative period, in as the same manner as for Case 2. CBCT is a modality available to dentists which pro-vides images of high spatial resolution and accuracy in the search for apical periodontitis and thickening of the sinus mucosa, compared to the images obtained in 2D, especially in the upper maxillary teeth 8. CBCT images, obtained with an extended field of view, allow evaluation of the airways and mucosal thickening, which has been one of the most frequent incidental findings 10. Odontogenic maxillary sinusitis diagnosis may be complex and, in some situations, even performing a clinical exam and using traditional 2D radiography such as panoramic radiography may not be enough. In these two cases reports the use of Cone Beam Computed Tomography and its 3D reformations pro-vide more accuracy when evaluating the anatomical and pathological factors that can contribute to OMS: the relationship between the maxillary sinus, tooth, periapical and periodontal lesions. CBCT has become an important examination in OMS diagnosis.
In conclusion, these two cases reports of Odontogenic Maxillary Sinusitis was diagnosed exclusively through CBCT, that improved the image de-tails like thickening maxillary sinus mucosa, bugging, expansion and rupture of the maxillary sinus floor, which were not observed on 2D x-rays images. In addition, CBCT contributed to the endodontic and surgical treatment plan due the identification of infectious focus and improved a better anatomical visualization between the affected teeth and the maxillary sinus.