INTRODUCTION
Actinomycosis is a chronic suppurative infection that afects soft tissues 1,2. Cope, in 1938, classified it into three diferent forms: cervicofacial (50%), thoracic (30%) and abdominal (20%) (3). Actinomyces, the etiologic agents of the disease, are anaerobe/microaerophilic, Gram-positive, commensal bacteria, which are found in the oropharynx, gastrointestinal and urogenital tracts 2,4. When these microorganisms reach subcutaneous tissues, especially in immunocompromised patients, they become pathogenic 1. The clinical presentation of this infection can be similar to that of tuberculosis and carcinoma, and therefore, actinomycosis can easily be mistaken for these diseases 3.
The diagnosis of cervicofacial actinomycosis is often delayed, probably because of its low prevalence and unawareness of health care professionals about the pitfalls involved in the diagnosis process. These professionals, especially physicians and dentists, must be aware of its potential occurrence as well as the therapeutic management of the disease. The aim of this work was to review, in the available scientifi c literature, important information regarding the etiopathogenesis, clinical features and treatment of cervicofacial actinomycosis.
Etiopathogenesis
Actinomycosis was described in 1848 by Langenback 5), and in 1878, Israel and Wolf 6 observed and described the sulfur granules in human disease, and defined the anaerobic nature of the microorganism 7. Originally, it was considered of fungal etiology (mycos), in view of the slow growth and filamentous appearance of Actinomyces. Afterwards, it was confirmed that these microorganisms were bacteria 5. Accordingly, the morphology of Actinomyces shows filaments much narrower than fungal hyphae 6 and bacillary forms as well, and reproduction occurs by binary fission instead of spore formation or budding 5,6. Moreover, Actinomyces are killed by antibiotics, such as penicillin and erythromycin, but are not afected by antifungal drugs such as amphotericin B 5.
Actinomycosis is a rare infectious disease caused by various microorganisms of the genus Actinomyces, where Actinomyces israelli is the main etiologic agent in humans. However, A. naeslundii, A. visco-sus, A. odontolyticus, A. meyeri, A. gerencseriae, A. pyogenes, A. georgiae, A. graevenitzii and A. neuii can also be involved in the pathogenesis of the disease 3,7,8. Meanwhile, A. bovis is known to be the causative agent of actinomycosis in cattle but has never been isolated from humans 9.
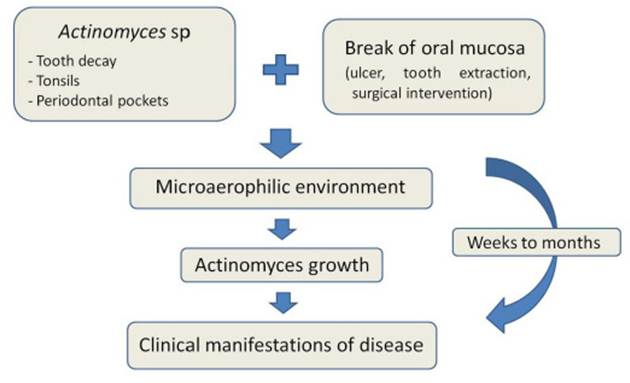
Cervicofacial actinomycosis is the most prevalent form of the disease 10,11. Actinomyces are part of the normal oral microbiota, where they are commensals of periodontal pockets, caries, dental plaque, calculus and gingival crevices 6). Nevertheless, they can become pathogenic by accessing the oral submucosa through an open door. Mucosal breaks play an important role in providing access to a microaerophilic environment favorable for infection. Therefore, factors such as complication of a maxillofacial trauma after surgical interventions and/or dental interventions in patients showing poor oral hygiene or caries can work as predisposing factors (Figure 1) 14,12,14. Actinomycosis occurs almost exclusively by direct invasion, and rarely through hematogenous spread 6.
Epidemiology
Actinomycosis is an endogenous, non-contagious and rare infection 9, which does not have racial predisposition or involvement of geographic factors in its etiopathogenesis 14. However, immunosuppression predisposes to the disease 15. There is slight preference for males, with a male:female ratio of 2.4:1 11. Among females, actinomycosis occurs more often between 11 and 30 years of age 11), whereas it is rare in the pediatric population 16. Lesions are more prevalent in the perimandibular region and seldom involve bone 17. When accessibility to penicillins was restricted, actinomycosis used to be fatal. During that time, mortality rates of up to 62% were reported 18.
Clinical features
Actinomycosis can occur in three diferent forms: acute, subacute or chronic 4. Usually the infection develops silently, showing a solid mass that slowly increases in size and forms many fistulas (Figure 2), which are specific features of the chronic phase 19. The acute phase, however, is less frequent and shows fever, fatigue, malaise and floating edema, reminding an acute dental infection, where pain and trismus can also happen 6,20.

Figure 2 Cervicofacial actinomycosis. Solid mass in mandibular region in a child (a) and in an adult patient (b); the nodule becomes fistulated, with draining pus (c), which can lead to scarring after treatment (d); within the material discharged through the fistulae, it is possible to see the sulfur granules (e, arrow) corresponding to the Actinomyces colonies (f, HE, 400X).
In most cases, signs and symptoms of infection such as fever, sudden cervicofacial pain, erythema, and edema are absent 14. Initially, the lesions show woody consistency, mimicking neoplasm, but with time, fistulas appear in the region. The nodule then assumes the characteristic multifistulated aspect 2. There is spread in a contiguous way, regardless of tissue planes, and there is release of bacteria through the fistulas as sulfur granules17. Regional lymphadenopathy is typically absent, also in more advanced stages 21. Cervicofacial actinomycosis can develop in surrounding tissues of any mandibular or maxilla sites. However, the mandibular region is the most frequent site of infection 6. Some cases can cause central nervous system (CNS) infection (2%) 12 by means of direct extension via facial sinuses, orbits, ear canal and perineural (22), where it is possible for the trigeminal ganglion to be involved via the oval foramen 5.
Diagnosis
Careful evaluation of the clinical features can lead to a proper diagnosis, which has to consider the presence of sulfur granules, as well as the identification of organisms in the examined tissue and positive cultures 13. Diagnostic tests include the following: (a) histopathological examination, especially when it mimics other diseases such as primary or metastatic carcinoma 13; (b) imaging techniques such as computed tomography (CT) 14, ultrasonography 15 and nuclear magnetic resonance, which can help to define the mass characteristics and adjacent soft tissue involvement 14, where CT can show typical cervicofacial lesions appearing as poorly defined and infiltrative soft tissue masses, which can spread to contiguous spaces, along with the appearance of small necrotic areas 13; (c) cytological analysis of fine-needle aspirate, which is the method of choice for the diagnosis of actinomycosis, providing an easy, safe, fast and highly effective method, even though sometimes it might not provide a definitive diagnosis 14).
Cervicofacial actinomycosis can represent a diagnostic dilemma for clinicians because it can mimic other infectious diseases such as tuberculosis (scrofula), abscesses, cysts and neoplasms 2,13,17. Soft tissues often show a woody consistency 2,23, which can lead to a wrong diagnosis of malignancy 2,24. Characteristic lesions develop slowly during weeks to months, giving a bluish or reddish appearance to the region. This presentation is often mistaken for cellulitis, although in fact representing venous congestion. Afterwards, a yellowish-serous exudate containing the characteristic sulfur granules drains onto the skin surface or oral mucosa 6. The infection can spread directly to the adjacent bones and muscles 25.
Sulfur granules consist of colonies of Actinomyces that grossly resemble sulfur grains 13. They are yellowish macroscopic structures firm in consistency and visible to the naked eye (figure 2e), varying from 100 to 1000 μm in diameter. Sometimes they can be scarce or absent, requiring many microscopic sections of the sample collected through the fistula or abscess walls to be identifi ed 5,6. Although strongly suggestive of cervicofacial actinomycosis, sulfur granules are not pathognomonic, as they can be seen in other diseases such as nocardiosis and chromomycosis 2,5,14,26.
Actinomyces shows filamentous or diptheroidal morphology, where the latter forms seem like non-pathogenic diphteroid Propionibacteria and the thin filaments exhibit V or Y ramifications and bacillary or coccoid forms 5. Colonies are visible by light microscopy with hematoxylin-eosin (H&E) 7. Grocott-Gomori-methenamine 5,7, methylene-blue, Gram or periodic acid-Schiff staining (PAS) 5, Methylene-blue, Gram, PAS and Grocott-Gomori staining disclose mycelial ramifications and Gram-positive filaments, which can be mistaken for streptococcus 5. With conventional methods such as Grocott-Gomori and H&E, it is almost impossible to differentiate Actinomyces from Noccardia species 7. Even p-amino-salicylic acid, MacCallen-Goodpasture and Brown-Brenn do not offer any additional sensitivity 6.
The use of specific conjugated fluorescent antibodies allows rapid and highly specific identification of many species of Actinomyces through direct staining even in mixed infections or after formalin fixation 2,5,7. The identification of individual filaments within granulation tissue is an advantage of this technique 7, even though confirmation by means of culture is necessary 2,5.
H&E microscopic examination of an excised mass or tissue biopsy can reveal acute or chronic inflammation with loculation of neutrophils, lymphocytes, plasma cells and macrophages as well as dense fibrous connective tissue. Microcolonies are seen as crowded basophilic masses at the center and eosinophilic at periphery with radiating filamentous arms 15,27, featuring the Splendore Hoeppli phenomenon 28. The number of plasma cells increases with lesion chronicity. Fibrosis can be mild in early infections, whereas chronic cases are associated with intense avascular fibrosis, which impairs even more the identification of Actinomyces colonies 5,6.
Treatment
Cervicofacial actinomycosis treatment requires attention in identifying other pathogens, since the infection tends to be polymicrobial. It is also worth recalling that actinomycosis has a great potential for recurrence and, consequently, may require prolonged treatment 13). Actinomycetes are sensitive to beta-lactams (penicillin G IV), being these agents the first treatment choice 17. The efficacy of the therapy can be related not only to its direct effect on Actinomyces israelli, but also to antimicrobial suppression of the other organisms that are involved in the metabolic ecosystem enabling Actinomyces to flourish. These microorganisms include Actinobacillus actinomycetemcomitans, Bacteroides, Eikenella, and Fusobacterium5.
Penicillin therapy should be intensive, and treatment duration depends on the severity of the case, sometimes lasting as long as 12 months. That is because of the avascular fibrotic walls of the lesions 19,29,30, which maintains the anaerobic environment, stimulating the organisms’ growth 11,31. Depending on disease severity, therapy may consist of high doses of penicillin G IV (10 to 20 million IU/day) for days or weeks, followed by oral penicillin V (2 to 4 g / day) for 3 to 12 months 13,17,32-34.
Actinomyces are in general sensitive to several antibiotics, where penicillin G is the first choice. In case of allergy to it, tetracycline, erythromycin, clindamycin or third-generation cephalosporins can be used 3,14,35,36. It is important to point out that metronidazol, aminoglycosides, aztreonam, sulfamethoxazole-trimethoprim, penicillinase-resistant penicillins such as nafcillin and oxacillin, and cephalexin as well are not active against Actinomyces5,17.
Surgical intervention may be needed if the response to antibiotic therapy is insufcient 2,13, or if there is an extensive area of necrotic tissue or large fistulas 2. It is sometimes indicated for bone curettage, necrotic tissue resection and drainage of extraoral fi s-tulas. When cervicofacial infection is confined, with low intensity and not associated with drainage fistulas, a clinical approach is preferred instead of surgical interventions 2,14. Table 1 summarizes reports in the literature about therapeutic management of cervicofacial actinomycosis.
Table 1 Therapeutic management of cervicofacial actinomycosis
| Anatomic site of the lesion (number of cases) | Drug and dosage | Duration of treatment (months) | Adjuvant treatment | Outcome | Reference |
|---|---|---|---|---|---|
| Between pharynx and epiglottis (n=1) | Amoxicillin 500 mg 8/8h | 3 | None | Remission | Volpi et al. (3) |
| Parotid (n=1) Submandibular (n=1) | Prolonged course of penicillin (W/S) High doses of penicillin (W/S) | W/S W/S | Partial parotidectomy None | Remission Remission | Stewart et al. (13) |
| Parotid (n=1) | Amoxicillin/clavulanate 2000 mg + 200 mg IV 2x/day(5 days); amoxicillin+ clavulanate 875 mg + 125 mg 3x/day (1 month) | 1.16 | Partial parotidectomy | Remission | Lancella et al. (14) |
| Cervicolateral (n=1) | Piperacillinum/tazobactanum 2 g + 0.250 g 3x/day (IV) and betamethasone IV, 4 mg/2 ml/day(6 days); amoxicillin/clavulanate 875 mg + 125 mg 3x/day (1 month) | 1.2 | Selective neck dissection (right side) | Remission | Lancella et al. (14) |
| Mandibular (n=1) | Amoxicillin/clavulanate 875 mg 12/12h | 12 | None | Remission | Smith et al. (17) |
| Parotid (preauricular) (n=1) | Ampicillin IV-sulbactam (4 days); amoxicillin/clavulanate (5 days) | 0.3 | Surgical drainage | Remission | Sudhakar et al. (23) |
| Mandibular (n=6); cheek (n=2); buccal (n=2); infratemporal (n=1); infraorbital (n=1); sublingual (n=1); W/S (n=6) | Penicillin G IV 12 million IU /day + metronidazole IV (1-16 days), followed by oral AB or ceftriaxon 2000 mg/day + clindamycin 600mg 3x/day | 0.2 -4.5 | Incision + drainage and debridement if needed (n=16); None (n=3) | Remission | Moghimi et al. (26) |
| Parotid (n=1) | Crystalline penicillin, 2 million IU, IV 3/3h (1 month); trimethoprim 160 mg/ sulfamethoxazole 800 mg (6 months) | 7 | None | Remission | Dubey et al. (36) |
| Parotid (n=4) | Penicillin G sodium IV 12 million IU/day (1.5 months); penicillin V oral 1000 mg/day (4.5 months) | 6 | None | Remission | Sittitrai et al. (37) |
| Submandibular (n=1) | High doses of penicillin (W/S) | 1 | Surgical excision | Remission | Volante et al. (38) |
W/S= without other specification; AB=antibiotic therapy
DISCUSSION
Actinomyces israelli is a commensal of the normal oral microbiota, which can become pathogenic if oral mucosal integrity is compromised. It is not possible to anticipate the infection, therefore the decision of prescribing antibiotics before tooth extraction, for example, should not be based on the possibility of the patient developing actinomycosis, which is rather unlikely 5). Nevertheless, cases of patients showing late infections after dental treatment as well as recurrent infections after short-course antibiotic therapy should be a warning to the dentist about the possibility of the occurrence of cervicofacial actinomycosis 5,37. Adequate oral hygiene with proper dental plaque control can prevent the disease, since it impairs the growth of Actinomyces in the oral environment 7.
Besides the possibility of actinomycosis mimicking neoplasms, the reverse process is also possible. That is, there are cases reported in the literature of squamous cell carcinomas misdiagnosed as being actinomycosis 40,41. This is a serious concern, since the late diagnosis of this neoplasm drastically impairs its prognosis 40.
Although cervicofacial actinomycosis shows low prevalence, it involves significant morbidity and prolonged treatment. In this context, prevention is the best approach, where basic prophylactic procedures and oral hygiene are capable of preventing the disease 37. On the other hand, in the case of actinomycosis occurrence, it is important to establish a correct and early diagnosis 17, which demands knowledge about its etiopathogenesis and clinical characteristics. In conclusion, cervicofacial actinomycosis is a rare bacterial infection that evolves slowly and often mimics other clinical conditions such as malignancies. The diagnosis is based on clinical features including the sulfur granules, as well as identification of organisms in the examined tissue and positive cultures. Treatment consists in antibiotic therapy and can last up to 12 months in severe cases. Health care professionals’ knowledge about the disease is crucial in a way to promote its prevention, early diagnosis and proper treatment.