Epidemiologic Characteristics and Transmission
In December 2019, a group of individuals diagnosed with pneumonia without etiology were reported in Wuhan, China, and later labeled as severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2) (1-3). The original symptoms of SARS-Cov-2 infection included fever, cough, and shortness of breath within 2 to 14 days after exposure 4. Other symptoms have been added later including such as fatigue, muscle or body aches, headache, loss of taste or smell, chest pain, sore throat, congestion or runny nose, nausea or vomiting, diarrhea and a rash on the skin, or discoloration of fingers or toes. 5
In the following weeks the infection spread to other Asian countries, Europe, North America, South America, and Africa, for which, on March 11, 2020, the World Health Organization (WHO) declared the disease COVID-19 a pandemic 5. As of December 2020; 68,812,210 confirmed cases of COVID-19 were detected worldwide, and 1,567,297 deaths have been reported 6.
The virus is highly contagious and spreads person-to-person through close contact, respiratory droplets, and aerosol particles.
Coronaviruses are part of the Coronaviridae family in the Nidovirales order 7. The outer surface of the virus contains spike-like proteins resembling a crown (corona). These proteins facilitate the link with receptors in the respiratory epithelial cells. In size, SARS-CoV-2 is small (65-125 nm in diameter), holds a single-stranded RNA of 26 to 32 kbs. There are four subgroups of the coronavirus family: alpha (α), beta (β), gamma (γ) and delta (ᵟ) 8.
The transmission of SARS-Cov-2 occurs from asymptomatic, presymptomatic, or symptomatic infected individuals 9. Person-to-person spreading occurs due to close contact with an infected person who is coughing, sneezing, or spreading respiratory droplets, and aerosols. These aerosols can enter the human body via inhalation through the nose or mouth and then go to the lungs 8,10. The angiotensin-converting enzyme 2 (ACE2), in the cells of the lower respiratory tract of humans, acts as a cell receptor for SARS-CoV-2 11,12. Wan et al., identified this receptor-like regulator in a cross-species human-to-human transmission 13. This ACE2 receptor has been identified also in the human oral mucosa cells (14-16), thus the oral cavity could be regarded as susceptible to SARS-CoV-2 infection 14,17,18. The incubation period after infection is 1-14 days, but 3-7 days in most cases. During the incubation time, the infected person is infectious 19,20. The virus has been detected in saliva 28.
Diagnosis and Detection of COVID-19
The clinical and public health needs of the pandemic required rapid and reliable tests to detect persons infected with SARS-CoV-2 29. At present, real-time reverse transcription-polymerase chain reaction (rRT-PCR) on respiratory specimens represents the reference standard test for the detection of SARS-CoV2 infection 27. To perform rRT-PCR, the sample is obtained through a nasopharyngeal swab 17. Sputum and oropharyngeal secretions have been suggested as possible targets for the molecular diagnosis of COVID-19 by rRT-PCR 28. Nasopharyngeal swabs require close contact between tested individuals and healthcare workers who may be at an increased risk of exposure if not donning appropriate barriers. Moreover, these types of specimens may also cause discomfort, and even bleeding in patients with low levels of thrombocytes 27,28.
Saliva has been used as a diagnostic tool for a variety of diseases 24,-32), conditions 36-38, and viral infections 33-35. Some studies have validated saliva as a tool to detect SARS-CoV-2 against (insert the comparison) 16,22,28,39 and reported sensitivity and specificity of X%, and Y%, respectively 28.
As a source of SARCS-CoV-2, saliva has some additional advantages: it remains stable at room temperature for up to 24 hours and up to a week at 4 °C 21. Furthermore, obtaining a saliva sample does not cause discomfort to patients, making it ideal for pediatric patients 22,40, by not requiring nasal swabs 24.
SARS-Cov-2 Transmission to Dental Practitioners
Dental practitioners are at higher risk of infection by SARS-CoV-2 because most dental procedures produce contaminated splatters, droplets, and aerosols 25. This is particularly important when providing care to asymptomatic or presymptomatic patients 17,27. Intraoral imaging is the most common radiographic technique; thus, care should be taken not to stimulate saliva secretion or coughing 54. In their interim recommendations to reduce transmission in dental settings. the U.S. Centers for Disease Control and Prevention suggest the use of extraoral instead of intraoral imaging, along with appropriate personal protection equipment (PPE). However, panoramic radiography and cone-beam computed tomography (CBCT) may expose the individual to higher levels of radiation than a single periapical image 56 or may not be a suitable alternative for intraoral imaging.
Several publications have reported on the radiological characteristics of COVID-19 individuals 41-45, and the recommendations on how to take their images. 46-52. Only one publication has provided specific recommendations for dental radiology 53.
Proposed Appointment Model for Oral-Dental Radiology
In the next section, we provide general guidance on how to devise a radiology appointment. The general recommendation of keeping social distance during the time the patient is in pre-clinical and clinical area as well as wearing mask applies. These recommendations, should be in concordance with institutional and national policies, 57 and communicated to the patient before the appointment 58.
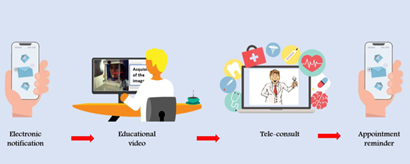
Preappointment (Figure 1)
1. Electronic notification of appointment date and time.
2. If possible, share with the patient informational videos on the radiographic procedures to be used.
3. Tele-consult to screen for symptoms, risk behaviors and potential exposures to COVID-19 follow institutional recommendations on what to ask and how, like the ones CDC recommended:
a. Have you experienced any of the following symptoms in the past 48 hours: (fever or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, diarrhea)
b. Within the past 14 days, have you been in close physical contact (6 feet or closer for a cumulative total of 15 minutes) with: Anyone who is known to have laboratory-confirmed COVID-19? OR Anyone who has any symptoms consistent with COVID-19?
c. Are you isolating or quarantining because you may have been exposed to a person with COVID-19 or are worried that you may be sick with COVID-19?
d. Are you currently waiting on the results of a COVID-19 test?
4. Send a reminder close to the appointment date with information regarding wearing masks and what to do upon arrival. Is common practice by most dental clinics to space the appointments so reduce crowding in the waiting area. Others require the patient to wait outside the office.
5. Scan and go concept: This concept aims to complete all administrative affairs before the clinical procedure 48. Thus, transactions such as payments or others should be handled electronically.
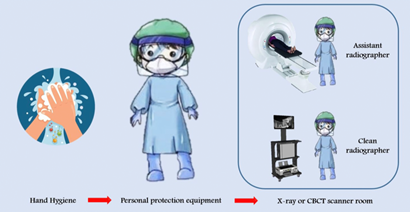
During the appointment (Figure 2)
Health questionnaire and history of potential risks after the teleconsultation. For this step, the same questions from the pre-consult could be used.
Measuring body temperature.
The patient is led to the radiological unit.
Patients and any companion should be wearing masks while in the office and receive appropriate standard radiation protection devices 59. Other recommendations for protecting surfaces in the office apply 60.
5. Use two radiographers: a radiographer assigned to operate the workstation and controls, and an assistant radiographer assigned to interact with the patient during clinical procedures 46,61,62.
6. Patients can mouthwash with very diluted hydrogen peroxide (0.75%) or long-lasting iodine solutions before the procedure, but there is no supporting evidence that these procedures reduce transmission of COVID-19 63.
7. There is no need to remove the mask during extraoral scans.
Post appointment
1. Disinfection of all surfaces: COVID-19 can persist on surfaces for hours or days, depending on the type of surface, temperature, or humidity of the environment 64. Thus, all the essential items in the room i.e. operating consoles such as monitors, keyboards, mouse, chairs, control panel, and exposure buttons or sensors should be covered with waterproof protective material. At the end of the radiological procedure, all covering material should be removed and disposed. Areas that have not been covered must be reprocessed with standard hospital disinfectant: low- or intermediate-level disinfectants, such as iodophor germicidal detergent solution, ethyl alcohol 70% or 75%, or isopropyl alcohol, following the equipment manufacturers' recommendations 46,49,65. Removing non-essential items from the clinical area reduce reprocessing time.
2. The scan room needs to be closed tightly sealed for 15 min to thoroughly ventilate and exchange the room air 60.
3. If necessary, consultation with the patient, family, colleagues should be done by phone or e-consult platforms 50.
4. Practitioners should review periodically the updates on epidemiological, clinical, and infection control information from reputable sources websites.
5. Reporting results from the radiological examination could be done electronically by radiology information system (RIS), or picture archiving and communication system (PACS), as well as an update to the patient via the online portal 46. The practitioner should be aware of legal requirements for sharing personal and clinical information and secure appropriate sign consent from the patient.
All the above is in concurrence with the recommended routine infection prevention and control practices during the COVID-19 pandemic released by the Center for Disease Control and Prevention (CDC) and the World Health Organization (WHO), such as implementing telehealth, screening triage, implement universal source control measures, and physical distance at least 6 feet between people, and performing only elective procedures during increased transmission in the population. 59,60,66
Impacts of COVID-19 on the oral radiology specialty
The original restrictions on clinical practice due to the pandemic affected the oral radiology specialty by reducing encounters to those required under emerging services only. In the medical field, experiences from other countries suggest a 50% to 70% decrease in imaging volume that lasts a minimum of 3-4 months 67. It is still too early to clarify the economic impact on dental radiology practices and services, especially when in most countries dental care has returned close to pre-pandemic figures. The American Dental Association (ADA) predicts that U.S. dental care spending could decline by up to 38 percent in 2020 and 20 percent in 2021 68. The most recent ADA data are encouraging since the modeling predicts that U.S. dental care spending could decline by up to 38 percent in 2020 and 20 percent in 2021. However, it could be expected that dental practices may be affected if additional restrictions are set in response to new outbreaks.
COVID-19 pandemic and its affect on clinical research
There are no reliable reports on the effect of COVID-19 on oral and craniofacial research. However, anecdotal information suggests that most clinical trials were postponed, or have interrupted their protocols in their inability to take direct measurements on participants in research centers or dental schools, due to lockdowns. Researchers have opted for conducting other aspects of their protocols to save time, 46,52,70. but intraoral interventions or measurements were postponed due to the pandemic, including those requiring imaging. Some have predicted loss of scientific productivity for as much as 1 - 2 years as the result of a shutdown 53,70. The effect will be particularly acute in clinical trials, where investigators will deal with missed visits, the need to re-engage existing subjects, having to recruit new subjects, and protocol alterations as reported in the medical field 70.
In the field of radiology, COVID-19-related research has increased to create components for personal protection equipment (PPE) and other devices 70. The need from several countries and healthcare institutions for these alternatives and the subsequent lack of supply might be addressed by the use of three-dimensional (3D) printing. It has become the solution to the shortage of PPE 71, even if none studies are describing the effectiveness.
Final Comments and Conclusions
Further studies are necessary to ascertain the health and economic impact of limiting dental care during COVID-19 restrictions, including oro- and maxilla-facial radiology. The magnitude of the pandemic has stretched the limited available resources and open the field for novel technologies.
Uncertainty as a consequence of the COVID-19 pandemic is demanding the profession to innovate. The most recent data from the U.S. suggest that practices are returning to levels of pre-pandemic busyness. However, new outbreaks will be the norm in the future. If there is anything the profession has learned from this pandemic, is that we were not prepared. It is necessary to invent, adapt, or improve new equipment, protective barriers, and disinfectants that will allow the delivery of dental care under safety standards. Ultimately, it will be the result of cooperation and agreement between the government, dental associations, academic institutions, and individual practitioners which will determine new practice environments, alternative clinical procedures in what we can call the new dentistry in 2021. In this document, we propose some of the procedures for the specialty of oral radiology.