INTRODUCTION
Mouth cancer is considered a public health problem. An estimated 15 190 new cases are expected to occur in the year 2020 affecting 11 180 men and 4 010 women, this being one of the most frequent malignancies in the current population 1,2.
Oncological surgery of the lesion is considered the first treatment option, followed by adjuvant radiotherapy or radiochemotherapy, depending on the stage of the disease. The most common side effects of radiotherapy are: oral, hypopharyngeal and esophageal mucositis, difficulty in chewing and swallowing, hyposalivation, dry mouth, loss of taste, trismus, radiation decay, osteoradionecrosis, among others 3,4. Patients present painful ulcers, dysphagia, odynophagia and difficulties in speaking, which can lead to malnutrition and treatment discontinuation. Odynophagia is characterized by swallowing pain, often requiring diet changes, which directly impacts the patient’s quality of life. Currently, photobiomodulation therapy, using low-level laser therapy is the treatment of choice for oral mucositis 5.
The low-level laser therapy modulates the inflammatory, repairing and analgesic process. This non-invasive and non-drug therapy is able to delay the development of oral mucositis, as well as to attenuate both the severity of the lesions and their duration 6.
Clinical protocols for intraoral photobiomodulation for oral mucositis are consolidated in the literature, but very few reports are available regarding hypopharyngeal mucositis control 7,8.
However, the pharyngeal region is difficult to access intraorally and this is why the light beam is unable to come into direct contact with the injured mucosa of that region, a fact that may reduce the laser therapeutic efficacy. In view of the above, the objective of this study was to propose the use of low- level laser therapy extraoral to treat odynophagia associated with radioinduced hypopharyngeal mucositis.
MATERIAL AND METHODS
This investigation was approved by the ResearchEthics Committee under number CAAE 72989417 0 0000 0121, dated April 9, 2018. The investigation was observational descriptive case series report.
Three patients older than 18 years undergoing oncologic head and neck radiation therapy or radiotherapy associated with chemotherapy (radiation doses equal to or greater than 5000cGy), who exhibited oral and hypopharyngeal mucositis associated with odynophagia, were assessed and voluntarily accepted to undergo this photobiomodulation technique on the bilateral carotid artery trigone and reporting about their perception of pain and odynophagia.
Hypopharyngeal mucositis was determined from the report of pain in the region, associated with odynophagia. In addition to using this technique to treat hypopharyngeal mucositis, patients received conventional photobiomodulation therapy to prevent and treat oral mucositis. The extraoral laser therapy clinical treatment proposed for hypopharyngeal mucositis used a diode laser (Therapy XT DMC®), λ808nm (infra-red), 100mW power, continuous mode, 4J energy and 40 seconds per point, 0.028cm2 spot size.
Information was collected such as: gender, tumor site, irradiated site, type of treatment performed, total radiation dose, number of radiotherapy sessions, at what point in time the radiotherapy laser therapy was started, pain complaints and odynophagia and use of nasoenteral tube. At the end of the treatment, all patients issued a verbal and spontaneous statement about the perception of their symptoms during the photobiomodulation sessions. The statements were recorded and later transcribed in text format.
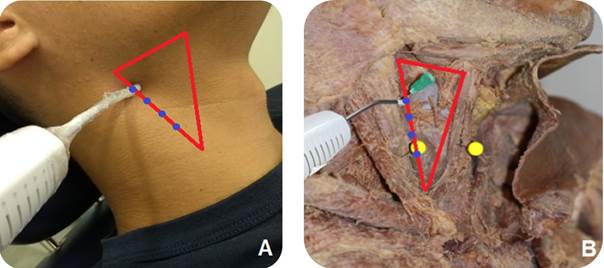
The extraoral application points selected were based on authors’ prior observation in cadavers to determine the region where it is possible to visualize the propagation of the visible red laser beam through the different tissues of the cervical structures (Figure 1). The study of the anatomy of the human cervical region was performed on dissected parts of cadavers (Human Anatomical Theater, Department of Morphology). All the cadavers used in this study were previously prepared using a 10% formaldehyde and glycerol medium. A diode laser (Therapy XT DMC®) was used, at a wavelength of λ660nm (visible red), continuous mode, 100 mW power, 10 seconds per point, 0.028cm2 spot size over all regions of the cervical trigones, time considered sufficient for visual observation of the red light beam passing through the tissues. Through direct observation, the area in which the visible red beam propagated and reached the hypopharynx region to the point of being seen with the naked eye was assessed.
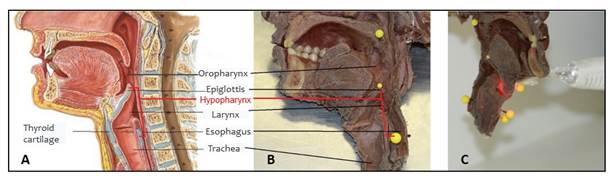
Figure 1 Anatomy of the human cervical region (A and B). Propagation of the visible red laser until reaching the hypopharyngeal mucosa (C).
Based on it, the carotid trigone was considered the best extraoral region for laser application allowing to reach the hypopharyngeal region. The anterior margin of the sternocleidomastoid muscle (SCM), one of the boundaries of the carotid trigone, was used as the most favorable application site, for being more easily clinically identified, through palpation. Thus, the low-level laser therapy was applied, in the clinical phase of the study, in 4 points (4J per point) perpendicularly and in contact with the skin, along the anterior margin of SCM muscle.
RESULTS
The three patients participating in this study were diagnosed with squamous cell carcinoma on the border of the tongue and were treated surgically and with head and neck radiotherapy. As a sequel to treatment, all patients developed oral and hypopharyngeal mucositis, and complained of odynophagia. Table 1 presents information related to patients. Patients 1 and 2, who started oral and hypopharyngeal photobiomodulation on the same day they started radiotherapy, developed oral and hypopharyngeal mucositis, reporting mouth pain and odynophagia; both patients maintained exclusively oral feeding throughout the cancer treatment. Throughout the treatment, both patients reported symptoms improvement in the oral cavity, but only patient 1 reported odynophagia improvement. The maximum score of mucositis they developed was grade 3, according to the classification of Sonis et al., 2004 9.
Table 1 Information of patients undergoing radiotherapy treatment in the head and neck region.
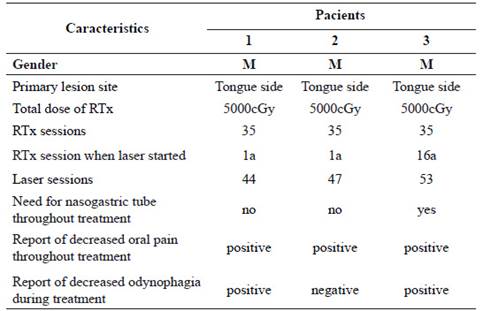
*M=male; cGy=centigrays (radiation measurement unit); RTx=radiotherapy.
Patient 3 was referred to the Hospital Dentistry Center, only when he was already in the sixteenth (16th) radiotherapy session, exhibiting grade 4 oral mucositis, according to the Sonis, et al., 2004 9 classification and using a nasoenteral tube. After performing oral and hypopharyngeal photobiomodulation, the patient reported unmeasured pain improvement both in the oral cavity and in swallowing.
The three patients voluntarily and spontaneously orally reported about their experiences and sensations when being attended by the Hospital Dentistry Center team of dentists. The transcribed reports are presented below: Patient 1: “(...) Mouth sores appeared after one week of radiotherapy, it hurt a lot, I felt a lot of pain when swallowing, I chocked a lot, I always had to drink some water after food intake to be able to swallow. As soon as the laser was applied, I already felt better, it didn’t stop hurting totally, but I managed to eat soon after. The laser applied on my neck helped me a lot with the pain to swallow (...)”. Patient 2: “(...) In the first days of radiotherapy I lost my sense of taste, I already had a sore throat and mouth injuries. In the mouth I didn’t feel much pain, but I felt a lot of pain to swallow, I couldn’t eat properly. I wish there was something penetrating in my throat to relieve the pain, just like the laser has worked into the mouth (...). Patient 3: “(...) I felt pain all over my mouth and pain when swallowing. I couldn’t even rinse my mouth with water, or brush my teeth; I had to use a probe for eating. I started to recover very well after the laser application; with each session I felt better, mainly swallowing (...)”.
The region that allowed the best propagation of the laser beam was the carotid trigone, allowing good access of the red light to the hypopharynx. In this region, during application in cadavers, the visible red laser beam was observed spreading through all muscle and cartilage layers, thus being considered the best extraoral access site for laser application. The laser tip was positioned perpendicularly and in contact with the skin, along the anterior margin of the SCM muscle. The cadaveric anatomical study was important to establish the extraoral location of laser applications. A total of four points was then established, with 1 cm distance between them, following the direction of the SCM muscle along the carotid trigone, for an improved laser beam penetration and better analgesic effect (Figure 2).
DISCUSSION
Mucositis is the most undesirable consequence of radiotherapy or radiochemotherapy treatments 10,11. The low-level laser therapy has important therapeutic properties in the treatment of mucositis. For best results, the laser tip should be positioned as close as possible and perpendicular to the injured tissue 12. In oral mucositis, this is possible due to easier access to the tissues 4,7,8,11,13. In contrast, in hypopharyngeal mucositis, this direct contact between the tip of the laser device and the mucosa is unfeasible.
The carotid trigone has the anterior border of the median portion of the SCM muscle as a posterolateral boundary, the upper belly of the omohyoid muscle as an anteroinferior boundary and the posterior belly of the digastric muscle and stylo-hyoid muscle as an upper limit. In this study, the laser at the visible red wavelength was applied externally along the cervical structures, seeking to observe from which anatomical region the red light would reach the hypopharynx region. Although there is a vast literature on the application of intra-oral laser in oral mucositis, no clinical studies are available on the effects of photobiomodulation therapy in the hypopharyngeal region 3,7,8,13,15,16. However, in animal studies, significant effects have already been observed in the use of extraoral laser in the treatment of oral mucositis 16.
Likewise, no studies were found that evaluate swallowing in a clinical or instrumental way to verify the effect of applying the laser therapy protocol in dysphagia. In the study by Gautam et al., comparing a group submitted to oral laser therapy with a placebo group, the authors found that the need and duration of parenteral nutrition was significantly lower in the group treated with laser to control radiotherapy- induced oral mucositis 17. The authors considered the practice feasible to prevent and treat oral mucositis and minimize pain and dysphagia; however, similar studies that used laser in the hypopharynx region have not been described in the literature. No equipment is available on the market that will allow intraoral laser access to the hypopharynx region.
The laser photons, when crossing a material, can be absorbed or scattered, which can cause attenuation in the light intensity. This is why, a λ range between 600nm and 1200nm is widely used for the treatment of deep tissues (up to ~2cm) 18. The λ808nm diode laser is used in clinical practice for the therapeutic effects on deeper tissues (19, 20, 21).
Other authors, whose studies have evaluated the effect of low-level laser therapy applied extraorally, highlight the lack of investigation reports on the subject covered by our protocol. In addition, dosimetry revealed to be quite complex for these cases 16. In this article, we are suggesting the use of diode laser (Therapy XT DMC), λ808nm, 4 points of 4J each, 1 cm apart, applied perpendicularly along the anterior belly of the SCM muscle, bilaterally. In this way, a total of 32J is applied to the neck skin, in the region of the carotid trigone, and so far it is impossible to know how much of this energy actually reaches the hypopharyngeal mucosa.
The lack of measurable criteria when attending patients, lead us to opt for qualitative analysis through three observational case studies, seeking to understand how each patient understood empirically his individual reality 22, without extrapolating these impressions to a whole group. Despite being a clinical case series report, this report allows an initial analysis of how promising the carotid trigone technique is and can further be studied and improved 23, in an attempt to solve one of the major problems that cancer patients experience during treatment, which is the radio-induced hypopharyngeal mucositis.
Based on the patients’ reports, it is believed that laser therapy targeting the carotid trigone region caused analgesia in the hypopharynx: Patient 1: "As soon as the laser was applied, I already felt improvement; it never stopped hurting totally, but I was able to eat soon after" and patient 3: "I started to recover very well after the laser applications; in each session I felt better, especially to swallow". Although patient 2 did not report improvement in odynophagia, it can be inferred that the laser application contributed to patients 1 and 2 continuing to feed exclusively orally and patient 3 progressing to oral feeding, considering that it is known that, during radiotherapy in the head and neck region, the need to use an alternative feeding route can reach 61% of cases 23, due to pain, weight loss and dysphagia conditions.
The importance of developing a laser application protocol for hypopharyngeal mucositis was also perceived by patient 1: "The laser applied on my neck helped me a lot with the swallowing pain”. Patient 2 reveals that "... I wish there was something that entered my throat to relieve the pain, just as laser has worked out in my mouth".
One of the limitations of this study was the difficulty in measuring the energy that can reach the hypopharyngeal mucosa through the extraoral application of laser therapy. In addition, clinical studies are required to be able to classify the degree of hypopharyngeal mucositis and that better assess the analgesia achieved by this suggested laser therapy protocol in an extraoral region of the carotid trigone. It was concluded that within the limitations of this study, the carotid trigone was defined as the best extraoral region for laser application, in order to extend the benefits of photobiomodulation to the treatment of hypopharyngeal mucositis. Although most patients have reported improvement with the laser application in this region, further studies are needed to gather evidence of laser therapy effects, as well as the best protocols to be used.