INTRODUCTION
Root canal perforations are artificial communications between the root canal and the supporting tissues of the tooth or the oral cavity 1. They can be classified as pathological if they are caused by caries or root resorption, or as iatrogenic if they are produced during root canal treatment 2. The presence of pulp stones, calcification, rotated tooth, extensive caries, misidentification of the root canal, or posts are factors that can hinder access to the root canal and trigger perforations 3. Regarding posts, their magnitude is related to greater dentin excavation 2, which may lead to catastrophic consequences. Theoretically, a perforation into supporting tissues alone might not necessarily cause irreversible inflammation or failure; however,ifthere is bacterial inflammation the healing process will not occur 2,3. Thus, painful conditions, suppurations, abscesses or even fistulas can occur1.Traditionally, various materials have been used to seal perforations, such as calcium hydroxide, amalgam, reinforced zinc oxide cement; however, calcium silicate-based cements, e.g., the mineral trioxide aggregate (MTA) promote a better tissue response 3-5.
The MTA is a bioactive endodontic material that was initially developed in the 90s as a material for sealing lateral perforations 6, and is mainly composed of calcium and silicate elements 7, which set in the presence of humidity 8. MTA has adequate physicochemical properties 9, promotes low cytotoxicity 10, and provides adequate sealing 11. It is important to note that MTA is marketed in 2 forms: gray and white. The white MTA was introduced due to the potential discoloration effects of gray MTA, caused mainly by its radiopacifier, bismuth oxide 12. MTA has been described as an appropriate material for root-end filling, vital pulp therapy, apical barrier formation for teeth with necrotic pulps and open apexes and perforation repair 13.
The present case reports the management of two unfavorable iatrogenic perforations during post placement with mineral trioxide aggregate.
Case 1
An asymptomatic 25-year-old female patient was referred to the endodontics department to evaluate the right mandibular first molar (FDI tooth No. 46). The medical history of the patient was noncontributory. The dental history included a recent root canal treatment and post placement in the affected tooth. The clinical examination showed that there were no sensitivity to percussion or palpation and no extraoral or intraoral swelling. The radiographic examination revealed a radiopaque element in the distal root, which was compatible with metal post, perforating the middle third of the root. The diagnosis was "previously treated" and "normal periapical tissues". The treatment alternatives were discussed together with the patient, who consented to perform the removal of the metal post followed by sealing of perforation and replacement of restoration.
The local anesthesia was administered by oral infiltrationof2%lidocainewith1:100,000adrenaline (Alphacaine, Rio de Janeiro, RJ, Brazil). Then, rubber dam isolation was performed, the previous restoration was removed, the access was obtained, and the metal post was removed using an ultrasonic tip (E12, Helse Ultrasonic, Santa Rosa de Viterbo, SP, Brazil) coupled to an ultrasonic device (MiniEndo, Kerr Endodontics, Brea, CA, USA). A non-bleeding large perforation, withapproximately2-3mmindiameter,wasidentified in the middle third of the distal root. Before sealing, irrigation with 2% chlorhexidine (Maquira, Maringá, PR, Brazil) was performed using a 27G side-vented needle (Endo-Eze Irrigator Tip, Ultradent Products, South Jordan, UT, USA). After drying the perforation site with paper points, a matrix of calcium sulfate mixed with distilled water was placed, which acted as a barrier between bone and tooth. Once set the matrix after approximately 1 minute, the white MTAAngelus (Angelus, Londrina, PR, Brazil) repair cement was placed using an MTA Applicator (Angelus). After 24 h, the cervical and middle thirds of the distal canal were obturated using gutta-percha and AH Plus sealer (Dentsply DeTrey, Konstanz, Germany) using the continuous wave technique. The access cavity was sealed with a glass ionomer cement (Fuji IX GP Fast; GC Corporation, Tokyo, Japan). An indirect resin restoration was placed after adjustment of occlusion and proximal contacts. The 1-month, 1-year and 3-year follow-up showed favorable evolution (Figure 1).
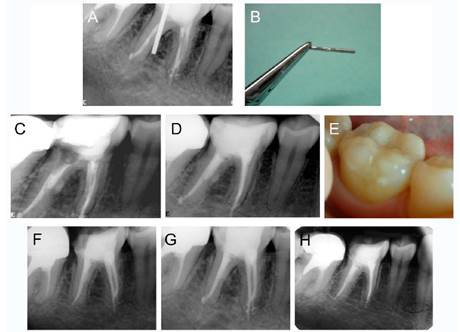
Figure 1 Illustrative images of the management of case 1, tooth 46. (A) Preoperative periapical radiograph. (B) Metal post removed from root canal. (C) Periapical radiograph after application of mineral trioxide aggregate into perforation site. (D) Postoperative periapical radiograph after final restoration. (E) Clinical view of the final restoration. (F) 3-month follow-up. (G) 1-year follow-up. (H) 3-year follow-up.
Case 2
A symptomatic 43-year-old female patient without non-contributory medical history was evaluated at the endodontics department of the Central Hospital of the Peruvian Air Force.
The dental history included a root canal treatment and post placement in the second mandibular premolar (FDI 35 tooth) 3 months ago, a temporary restoration and spontaneous pain in the left mandibular area. The clinical examination showed that there was sensitivity to percussion; however, there was not extraoral or intraoral swelling. The inadequate adaptation of the provisional restoration allowed the leakage of oral fluids into the tooth. The radiographic examination revealed radiopaque line compatible with fiber post, which perforated the middle third of the root, as well as bone loss adjacent to the perforation site.
The diagnosis was previously treated and symptomatic apical periodontitis, so the nonsurgical endodontic treatment, including the removal of the fiber post and sealing the perforation was recommended. The patient consented to perform the procedures.
The local anesthesia was administered by oral infiltration of 2% lidocaine with 1: 100,000 adrenaline (Alphacaine). After absolute isolation of the tooth, the fiber post was removed using an ultrasonic tip (E12, Helse Ultrasonic) coupled to an ultrasonic device (MiniEndo, Kerr Endodontics), which allowed an easy removal with a tweezer. A non-bleeding large perforation, with approximately 2-3mm in diameter, was identified and provisionally sealed with polytetrafluoroethylene (Teflon) tape to allow retreatment. The filling material was removed using the Mtwo retreatment system (VDW, Munich, Germany) using an R25.05 file complemented with Mtwo system (VDW) up to 40.04 file. The irrigation protocol was performed using 2.5% sodium hypochlorite (NaOCl) using a 27G side-vented needle (Endo-Eze Irrigator Tip, Ultradent Products). Once removed the Teflon, a calcium hydroxide dressing was placed in the canal and perforation for 15 days. In the second session, it was observed that the coronary remnant of the tooth had fractured; however, without compromising the sealing of the provisional restoration or the sufficient coronary remnant for the restoration, which allowed to continue the treatment. The calcium hydroxide was removed from the canal, leaving the residual paste in the perforation to act as a matrix for the placement of white MTA Angelus (Angelus) repair material, which was placed using an MTA Applicator (Angelus). The canal was obturated using gutta-percha points and AH Plus sealer (Dentsply DeTrey) using the continuous wave technique. A fiber post was placed immediately, and subsequently, a crown. The 6-month follow-up showed a favorable evolution. The 2-year follow-up showed that another colleague placed a metal post and a metal-ceramic crown.
Although with different prosthetic treatment, the 6-year follow-up showed a favorable evolution and bone neo-formation at the perforation site. (Figure 2).
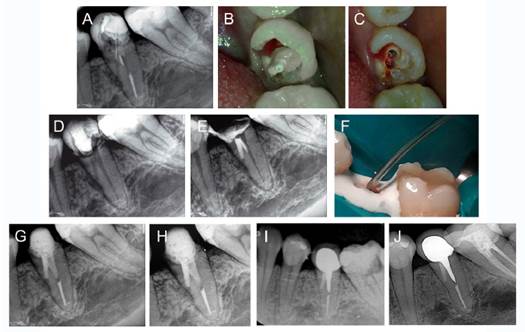
Figure 2 Illustrative images of the management of case 2, tooth 35. (A) Preoperative periapical radiograph. (B) Clinical view of the tooth crown with the fiber post exposed to the oral cavity. (C) Clinical view of tooth crown after fiber post removal. (D) Periapical radiograph after removal of fiber post and filling material. (E) Periapical radiograph showing the coronal tooth fracture and the application of mineral trioxide aggregate (MTA) into perforation site. (F) Clinical view of the application of MTA into perforation site. (G) Postoperative periapical radiograph, after placement of a fiber post (H) 6-month follow-up. (I) 2-year follow-up, after the placement of a metal post and crown for prosthetic reasons. (J) 6-year follow-up.
DISCUSSION
In this report of two cases, the management of unfavorable root perforations using MTA was presented.
Root perforations are complications that have an incidence of approximately 2.3% 14. A study reported that 47% of perforations occur during endodontic treatment, while 53% occur in the prosthetic phase 15. Another study reported that the presence of perforations, either pre-operative or during treatment, significantly affect the outcome of orthograde treatment 16. Additionally, large perforations are associated with higher pathological changes of periodontal tissues 14, as presented in both cases. The failure rate has been reported to be 16% when it is greater than 3mm, and 6% when it is 2-3mm 17. The present case report showed healing and favorable evolution at 3 and 2-year follow-up in case 1 and 2, respectively.
It has been described that three clinical factors are relevant in the prognosis and healing of perforations: location, size and time 2. In both cases, the location factor was favorable since they were in the middle third of the roots. It has been described that the prognosis is worse in the so-called "critical zone", which corresponds to the gingival sulcus and the crestal attachments since greater bacterial contamination can be promoted, generating a periodontal pocket 2. On the other hand, regarding the size factor, in both cases, it was observed that the etiology was a previous post placement, which is considered unfavorable perforation due to the high amount of tissue that is excavated,andthedifficultyofobtaininganadequate sealing 1. In case 2, the time factor aggravated the condition because the temporary restoration was adequately sealed for 3 months, which favored bacterial contamination and subsequent painful symptoms in the patient. Regarding this, it has been described that the faster the sealing, the better the prognosis 2.
The perforations sealing was performed using two different approaches, a single session and two sessions. In case 1, considering that the patient had undergone recent root canal treatment and had an adequate coronal sealing, the perforation was sealed performing a single session approach, which is characterized by the use of a calcium sulfate matrix, which is a resorbable material that sets quickly and serves as a suitable matrix for MTA 18. In addition, the perforation was irrigated with 2% chlorhexidine to avoid that a possible extrusion would have complicated the case. In case 2, considering that the tooth had been contaminated for a long time (3 months), it was decided to place calcium hydroxide in both the canal and the perforation to allow bacterial decontamination. Although calcium hydroxide generates areas of necrosis when it is in direct contact with tissue, it promotes tissue repair and mineralization due to the calcium ions that are released 19. Additionally, calcium hydroxide served as a matrix before the placement of the MTA 3. The use of matrices of calcium hydroxide or calcium sulfate prior to perforation sealing with MTA is based on the fact that MTA Angelus exhibits less sealing when not used with a matrix 11.
Various materials have been used for the repair of perforations, among them MTA 20. The MTA has been used for the repair of perforations due to its adequate physicochemical 9,11 and biological 4,10 properties. Clinical studies have shown that the use of this repair material promotes long-term success of perforation sites regardless of the location factor 20.














