INTRODUCTION
Oral mucocele is a non-infectious reactionary lesion characterized by the accumulation of saliva, which results in increased volume in the affected area. The disease is histologically subdivided into two main categories: mucus extravasation phenomena (MEP) and mucus retention cysts (MRC). MEP arise from trauma and rupture of the minor salivary gland duct, causing extravasation and concentration of saliva in tissues surrounding it, forming a cavity inside soft tissues without epithelial lining, a pseudocyst, which corresponds, on average, to 90% of cases. MRC occurs due to the obstruction of this duct; saliva is surrounded by ductal epithelium, leading to the formation of a true cyst, which occurs in about 10% of cases 1.
Both cases have similar clinical features. Increased smooth surface volume is observed, varying its color and consistency according to the size and depth of the lesion, which is bluish in color, transparent or similar to the mucosa. The size, on average, ranges from 0.3 cm to 2.2 cm. It often regresses spontaneously, but it recurs in most cases 2,3.
For the final diagnosis of mucocele, it is necessary to observe the microscopic characteristics through excisional biopsy. Histopathological examination shows oral cavity filled with amorphous and eosinophilic material, compatible with outpouring of mucin, surrounded by inflammatory cells, mainly foamy macrophages and neutrophils, the vast majority being surrounded by granulation tissue. In the case of MEP, there will not be any type of epithelial lining, whereas in MRC, ductal epithelium lining is observed, making a differential diagnosis with fibrous hyperplasia, lypoma, focal papilloma, vascular lesions or hemangioma 4,5,6.
Mucocele treatment is currently performed through a variety of options: iodine tincture 3; sclerotherapy by injection of pingyangmycin or anhydrous alcohol 7; cryotherapy 8 and micromarsupialization therapy 9. However, scalpel excision is still the most used treatment, even causing greater intraoperative bleeding, post-surgical edema, scarring and considerable risk of causing damage to other ducts of the minor salivary glands close to the lesion 3.
Clinical case
A 27-year-old non-white male patient sought the clinic-school service of the Department of Dentistry, State University of Paraíba (UEPB), complaining of “a lump in the lip”, with no report of parafunctional habits, previous trauma to the region and pain. On intraoral physical examination, a nodule was observed in the internal mucosa region of the exophytic lower lip, sessile, mucosa-like in color, with smooth and whitish surface in the upper region, measuring 2.0 cm in diameter, with smooth and fluctuating consistency on palpation and well-defined contours (Figure 1), without symptoms on palpation, with evolutionary history of approximately three months; the patient did not report systemic diseases.
Under the diagnostic hypothesis of mucocele, the entire lesion was surgically removed after infiltrative local anesthesia with Alphacaine 100® (DFL). Surgical excision was performed using high-power diode laser (Thera Laser Surgery®) with wavelength of 808 nm and power of 2.0 W in continuous mode, under constant aspiration (Figure 2), with duration of 5 min and 30 s. No bleeding was observed during the procedure and there was no need for suture.
Soon after the surgical procedure and during the four subsequent weeks, the patient was submitted to low-power laser therapy (LPLT) with diode laser (Twin Laser ® MMOptics - São Carlos, Brazil), under the following parameters: wavelength (λ) of 660 nm, energy of 1J, power of 40 mW, for 30 seconds of spot irradiation, with spot area of 0.04 cm². The spot was positioned perpendicular to the tissue, touching it.
At the end of each treatment session, the patient’s perception of postoperative pain was assessed using the Visual Analog Scale (VAS), which is an instrument to help measure pain intensity. It consists of a 10-cm line, with “0” representing “no pain” and “10” representing “unbearable pain”, with “1” to “2” being considered“mild pain”, “3” to “7” “moderate pain” and “8” to “9” severe pain. During the immediate postoperative period, the patient reported no pain, scoring “0” on the VAS.
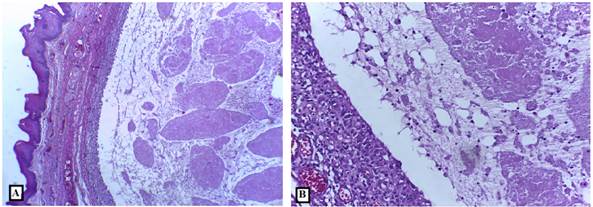
Histopathological analysis showed the presence of cavities containing amorphous and eosinophilic material in the subepithelial region compatible with mucus. Numerous inflammatory cells, including numerous foamy macrophages, were associated with mucus. The lesion area was surrounded by fibrous connective tissue and covered by parakeratinized stratified squamous epithelium, both with normal appearance (Figure 3 (A and B)), and the diagnosis of MEP was established
Source: Direct search. 2019
Figure 3 Photomicrograph demonstrating the presence of cavity containing amorphous and eosinophilic material in its interior and delimited by granulation tissue.
DISCUSSION
Surgical excision with laser, in this case, demonstrated, among the main benefits during the trans-operative period, hemostasis, and consequently better vision of the operative field and reduced surgical time, considering the size of the lesion, which corroborates findings by Vitale et al., 10, and Chinta et al., 11, who in their studies of mucocele removal, used high- power diode laser with parameters similar to those of the present study. In this case and in studies mentioned above, it was found that laser provided very satisfactory hemostasis, with clean and quick excision.
The used surgical technique has a pivotal role at the time of biopsy, during which the sample size and the specimen quality must be considered. Biopsies performed using a cold scalpel blade may cause physical trauma to the sample, e.g., due to tissue crushing caused by inadequate sample clamping, which then leads to distortions in tissue fixation and histological evaluation. In contrast to this, high-power laser can promote burning of the edges of the lesion and contraction of collagen fibers. This can hamper or even make the histological evaluation of the sample impossible 12. Thus, it is recommended that surgical excision using high-power laser should be performed on samples measuring at least 12 mm in diameter, in order to ensure that the thermal damage caused by the laser will not later interfere in the analysis and diagnosis of the lesion 13.
In the present study, the edges of the lesion showed small charred areas . However, this finding did not affect the analysis and diagnosis of the lesion, once the thermal damage was restricted to the edges of the lesion. Such findings were in line with earlier studies conducted by Erbasar et al., 14 and Mathur et al., 15.
In the present case, there was no need for suture, corroborating the study by Concepción et al., 16, who aimed to report the main findings regarding the use of diode laser for the treatment of soft tissue injuries. Among the main information, it was reported that, in none of the cases found, the need for suture was reported.
LPLT was applied soon after surgery and weekly for one month after the surgery, aiming to obtain the photobiomodulating effects of the laser: analgesia, inflammation modulation and tissue repair acceleration, which was achieved due to the absence of edema, moderate pain only on the seventh day and complete healing within 30 days. These results confirm the findings of Ahad et al., 17 and Arshad et al., 18, in which in both studies, it was possible to verify accelerated healing at each patient return and non-existent or very small discomfort. The results of the aforementioned studies differ from the results found by Feitoza et al., 12, who highlighted that the tissue repair process in surgeries performed using high-power laser takes longer since the healing process occurs by second intention, and because there is no approximation of the wounds edges.
During the 14 months since the surgery, no recurrence was observed, corroborating the study by Qafmolla et al., who compared the results of the surgery to remove mucocele in 20 patients, ten using conventional scalpel and ten using diode laser (980 nm, continuous mode, 300 µm optical fiber, 4 W), and verified that cases treated with laser had no recurrence, less pain complaint, no need for medication prescription and less relevant or non-existent scars 19. However, as disadvantages, it was reported that, during healing, there was greater number of patients who complained of unfavorable esthetics compared to the surgical wound. It was also possible to observe that, on average, total repair took longer than in cases performed with scalpel. The authors also highlighted the benefits of surgery using diode laser, such as greater hemostasis, reduced surgical time and elimination of the need for sutures 19.
Thus, it was possible to verify the benefits of high-power laser combined with LPLT in relation to conventional techniques, during the trans and postoperative period, bringing greater comfort to both professional and patient during the procedure, especially during the healing period. However, it is essential to clarify to the patient, before the procedure, that the area operated during the beginning of the healing process may not have an ideal esthetics, which is normal for this type of surgery, being overcome by the clinical and surgical advantages of the application of this technique. The need for more comprehensive studies to prove such observations is also highlighted.
CONCLUSION
The results observed in this clinical case suggest that the treatment of mucocele lesions, with excision using high-power diode laser, associated with LPLT in the postoperative period, is a safe, fast and effective procedure for both professional and patient and presents a favorable postoperative period. In this case, the patient’s perception of post-surgical discomfort and the procedure itself reinforces the idea that this type of protocol should be increasingly investigated in further studies and adopted in clinical practice, aiming to provide another type of treatment for this type of lesion and all benefits that this protocol provides for both professional and patient.

















