INTRODUCTION
Described for the first time by Crawford in 1896, dry socket is currently considered to be the most frequent postoperative complication following a dental extraction, occurring in approximately 1% to 5% of all dental extractions (1, with incidence increasing to 25% to 30% in the extraction of lower third molars 2. Dry socket is the inflammation of the alveolar bone at the site of the extraction, characterized by severe pain and the partial or total lysis of the blood clot. Clinically, there is an increase in the volume of the soft tissue, with areas of erythema, bone exposure, halitosis and, primarily, localized or referred pain 3. The pain and the onset period are the specific clinical symptoms for a correct diagnosis 4. Onset period is day 2 to 4 after surgery 5. While dry socket is a well-known and well-studied pathology, its etiology has yet to be determined precisely, although the suggested cause is the increase in fibrinolytic activity leading to the lysis of the blood clot 3. This increase in activity may result in the direct activation of the plasminogen pathway via the release of activators due to trauma of the bone cells of the alveoli, or in indirect activation initiated by bacteria-secreted activators 6. It is considered to be multifactorial and, over the years, different authors have described possible predisposing factors, amongst them infection and presurgical pain, smoking, use of oral contraceptives, age, sex, the tooth indicated for extraction, the difficulty and trauma generated during the surgery and the use of intraligamentary anesthesia, as well as others (1, 5, 7, 8).
The epidemic of a new disease produced by the SARS-CoV-2 virus, called COVID-19, originated in December 2019 in Wuhan, Hubei Province, China 9. It spread rapidly to other provinces, and then to the rest of the world. On March 11, 2020, the WHO declared it to be a global pandemic, and it became a public health emergency of international concern. In Argentina, preventive mandatory social isolation (PMSI) was established on March 20, 2020, under Decree of Necessity and Urgency 297/2020. Buenos Aires University School of Dentistry (FOUBA) functions normally as a Dental School/Hospital. The PMSI decreed by Argentina’s National Executive Power affected the teaching and healthcare activities of nearly all areas of the hospital, with the Emergency and Patient Orientation Service remaining as the only part of the Institution able to provide dental care to the community of the Metropolitan Area of Buenos Aires (MABA) in Argentina.
The aim of the present study was to evaluate the prevalence of dry socket as a postoperative complication following extraction when the common denominator at the surgical site was acute, intense pain in the immediate preoperative, independently of the etiology which determined its indication, during the PMSI for the COVID-19 pandemic.
MATERIAL AND METHODS
This was a descriptive study, in which 1209 individuals of both sexes and all ages were included. All participants had indication for extraction of permanent teeth and were walk-in patients at the Emergency and Patient Orientation Service of the Buenos Aires University School of Dentistry during the PMSI, from March 20 to June 20, 2020. We included patients with acute, intense pain at the surgical site. All patients were operated by calibrated personnel, using the same treatment process, which consisted of an initial 3-stage protocol: 1 - Diagnostic process of the emergency: including the systematic preparation of a medical record and physical exploration of the patient, as well as additional urgent diagnostic techniques or explorations to initiate treatment urgently and/or the possibility of excluding the process as urgent. 2- The therapeutic process of urgency: consisting of dental extraction with a protocolized technique. 3 - Patient follow-up: subsequent monitoring, including postoperative checks and an adequate comprehensive treatment plan, once the dental urgency had been resolved.
Patient data was recorded on a spreadsheet which was completed by the dentists who provided patient care, all of whom were calibrated in the diagnostic criteria and surgical technique to be used. The variables used in the study were: age, sex, tooth, location of the tooth in the jaw, type of surgery (non-erupted/erupted tooth), smoking, family history of Diabetes Mellitus and Hypertension, use of Oral Contraceptives, and psychiatric medication. All surgical procedures were performed under local anesthesia (4% carticaine hydrochloride with adrenaline 1:100000 [TOTALCAINA FORTE® Microsules Bernabo, Argentina]), and intracrevicular incision with a #15 interchangeable leaf type scalpel (Swamm Morton, Sheffield, England). The mucoperiosteal flap was raised with a round periosteal elevator (Hu-Friedy, Chicago, IL, USA); the exeresis with a straight elevator (Hu-Friedy 303, Chicago, IL, USA) and/or extraction pliers; the curettage of the alveolar cavity and suture with simple stitches with 000 silk (Wego® Foosin Medical Supplies Inc., Ltd. Shandong, China). A local compressive pack was applied to finalize all surgeries. Postsurgical indications were delivered verbally and in writing, with indication for non-steroid anti-inflammatory analgesics during the first 48 hours. Patients were also instructed that, in case of pain at any time, they should call or visit the Emergency Service, where postoperative evaluations would be performed.
Dry socket diagnostic criteria: a diagnosis of dry socket was considered when there was combined total/partial absence of the blood clot during examination and patient reported intense localized or referred pain between postsurgical day 2 and day 5 (5,10.
Treatment of dry socket: in the cases with confirmed diagnosis of dry socket, the treatment was intended to eliminate painful symptoms and promote healing of the alveolar wound. Local treatment involved cleaning the residual alveoli with saline solution until there was clear absence of detritus, followed by the application of Balsam of Peru with Iodinated Gauze inside the bone socket in a self-maintained technique. Said procedure was repeated every 48 hours until signs and symptoms disappeared. Patients were also prescribed analgesics every 8 hours on demand.
The categorical data was described by means of absolute frequencies and percentages with confidence intervals of 95% (CI95), estimated using the score method (11. For comparison of frequencies, the Chi square test was used, with a significance level of 5%. The following software was used: Calc, from Apache OpenOfficeTM v. 4.1.6 12, and InfoStat v. 2020 (13.
This study was approved by the Ethics Committee of the School of Dentistry of the University of Buenos Aires -FOUBA Res. (CD) Nº330/19-01-. All procedures were in agreement with the ethical rules of the institution and the Helsinki Declaration of 1964. The procedure was explained to all patients and all participants signed informed consent.
RESULTS
We studied 1372 dental extractions in 1209 patients. Of the 1209 patients operated, 940 were female (77.8%; CI95: 75.3% to 80.0%) and 269 were male (22.2%; CI95: 20.0% to 24.7%). Patient age range of was 8 to 98 years, with average age 41 years. A total 1372 dental extractions were performed.
Of the surgical patients, 29 were diabetic (2.4%; CI95: 1.7% to 3.4%), 63 had high blood pressure (5.2%; CI95: 4.1% to 6.6%), 30 used psychiatric medication (2.5%; CI95: 1.7% to 3.5%) and 26 had hyporthyroidism (2.2%; IC95: 1.5% a 3.1%): none of them suffered dry socket.
Dry socket was diagnosed in 12 patients (1.0%; CI95: 0.6% to 1.7%), whereas the rest of the patients did not suffer dry socket (99.0%; CI95: 98.3% to 99.4%). According to sex, 0.85% (8 individuals) of males y 1.48 % (4 individuals) of females developed dry socket. Within the sample, the percentages of patients with dry socket varied among the different age groups, although there was no significant association between the presence of dry socket and age group (Chi-square=6.84; df=4; p=0.14) (Table 1).
Table 1 Patients with and without dry socket according to age groups.
* CI: Confidence interval
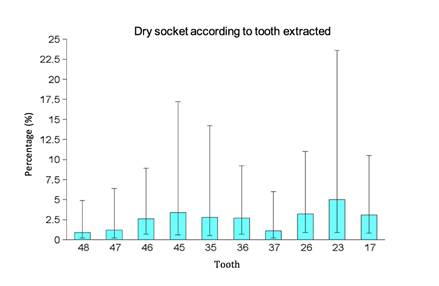
In 1372 dental extractions was diagnosed 14 dry sockets (1.0%; CI95: 0.6% to 1.7%), whereas the rest of the patients did not suffer dry socket (99.0%; CI95: 98.3% to 99.4%), in the rest of extractions there was no dry socket (99, 0%; CI 95: 98,3 to 99,4), this difference was significant (Chi-square = 1316.57; df = 1; p < 0.05). The dry socket cases that were found occurred in the extraction of the following teeth: 48, 47, 46, 45, 35, 36, 37, 26, 23 and 17 (Figure 3). Table 2 show the distribution of these cases. Dry socket was not found after the extraction of other teeth. Of the 1372 dental extractions, 54 were impacted third molars; it should be emphasized that the prevalence of dry socket in these cases was 0%.
Table 2 Extractions with and without dry socket, according to the tooth removed.
* CI: Confidence interval
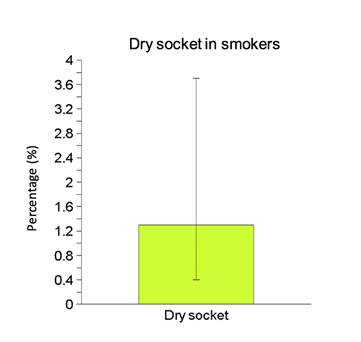
The sample included 237 patients who were smokers (19.6%; CI95: 17.5% to 21.9%). Amongst the smokers, 3 suffered dry socket (1.3%; CI95: 0.4% to 3.7%; Figure 1). Within the 972 non-smokers, 9 experienced dry socket (0.9%; CI95: 0.5% to 1.8%). No significant relationship was found between smoking and presence of dry socket (Chi-square=0.22; df=1; p=0.64).
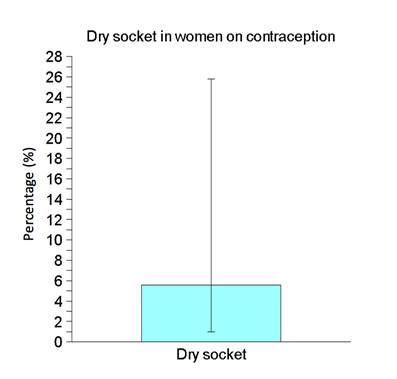
Eighteen patients took oral contraceptives, equivalent to 1.5% of the total of patients treated (CI95: 0.9% to 2.3%), or 6.7% of total of females (CI95: 4.3% to 10.3%). Only one of the 18 women who took oral contraceptives suffered dry socket (5.6%; CI95: 1.0% to 25.8%, Figure 2); and 3 of the 251 women who did not take oral contraceptives did suffer dry socket (1.2%; CI95: 0.4% to 3.5%). This study found no significant association between the use of oral contraceptives and the occurrence of dry socket (Chi-square=2.18; df=1; p=0.14).
DISCUSSION
The results of this study reveal the prevalence of dry socket in the Emergency and Patient Orientation Service of Buenos Aires University School of Dentistry in a total 1372 dental extractions that presented severe pain in the immediate preoperative. The specific cases found in this study were 1.06%, similar to the data reported by other authors 1,5,8 who analyzed this complication without the variable of the presurgical pain.
When considering the surgical extraction of impacted teeth, several of those studies mention an increase of the incidence up to values of 30% 8. It is suggested that this may be caused by an increase in the release of secondary activators in response to alveolar bone trauma, as well as the greater complexity and length of the procedure, the need for administering more anesthesia and consequently, the higher dose of vasoconstrictive drugs (which may affect the healing process by diminishing the blood flow and oxygen tension). As a result of these conditions, there may be an increase in fibrinolysis, promoting the onset of dry socket 5,7. In contrast to this theory, our investigation presented not an increase, but in fact a decrease, reaching values of 0% out of a total 54 dental extractions. Because of the peculiar situation during the PMSI for the COVID-19 pandemic, all the dental extractions were performed by specialized dentists, trained in the area of Maxillofacial Surgery, which might explain the lower prevalence presented in the Emergency and Patients Orientation Service at Buenos Aires University School of Dentistry, as well as the fact that none of the extractions of impacted teeth developed dry socket. This could be related to the fact, reported in many studies, that the experience of the operator is a risk factor for the development of dry socket, given that operators who are beginning in their practice have less training, create greater trauma during the surgery, take longer to do it and possibly need to apply a greater dose of local anesthetic. Therefore, the skill and preparation of the operator must be considered when evaluating the possibility of postoperative dry socket.
With respect to patient sex, there was a slightly higher frequency of dry socket in female patients, coinciding with previous articles by several authors 5,10,14. This is because estrogens can stimulate fibrinolytic activity, generating the lysis of the blood clot and augmenting the risk of dry socket. This occurs in women who are not in the menopausal stage and continue to have high estrogen levels in the different stages of the menstrual cycle 15,16, as well as those who take oral contraceptives, which is the reason why oral contraceptives have been studied as a potential predisposing factor. That effect of contraceptives was established in 2013 17; nonetheless, in our study as well as another previous study (18, there was no significant association between use of contraceptives and presence of dry socket. This difference could be attributed to the low concentration of estrogens present in current oral contraceptives 6.
When considering systemic illnesses (diabetes, hypertension, hypothyroidism and medicated psychiatric conditions) we were unable to determine a relationship between them and the presence of dry socket, as opposed to other studies which established greater frequency of dry socket in patients with diabetes 19, although our findings were in agreement with the results of a previous study (8.
Upon analyzing the extraction site, a higher prevalence of dry socket was found in the mandible, both in our results and in the results of other authors 5,8,11,20. This could be explained by considering that, in opposition to the maxillary, the mandible is a more compact and less irrigated bone, possibly complicating the surgical procedure and the subsequent healing process 5.
Another factor associated to dry socket is patient age, which is directly proportional to the risk of the occurrence of dry socket, as noted by several studies. The potential effect of age could be attributed to the difficulty of the surgery at those ages because of the presence of more compact bone, leading to more traumatic or longer duration of the extraction process in these patients 19. The higher prevalence of dry socket in patients of advanced age may be related to a decrease in the capacity of wound healing and slower metabolism 15. In our study, the average age of the patients with postoperative dry socket was 32 years (matching what other authors have reported as greater prevalence in the 3rd and 4th decades of life 14,20. Nevertheless, in our study, there was no association between age and the probability of the occurrence of dry socket.
Smoking is also present in numerous cases of dry socket. It may cause detachment of the blood clot by the effect of suction and vasoconstriction. The latter can also limit the formation of the clot in the postoperative 7. The presence of nicotine as a component of the cigarette smoke must be taken into account, since it could increase the risk of microvascular occlusion and ischemia in the healing tissue by increasing the adhesivity of the platelets to the vascular walls. The heat inhaled during smoking could alter the healing potential at the surgical site because of its unstable state at high temperatures in the first few postsurgical hours 7. It should be noted that previous studies mention an augmented risk mainly when and if patients smoke during the first 24 hours after the dental extraction (20,21. Our results did not evaluate postoperative smoking. It did evaluate the habit of smoking frequently, but found that it did not play any part in the occurrence of dry socket, as reported by other authors in previous years (10,22.
Intense pain as a preexisting condition to dental extraction had not been studied in depth until this time. The results of the current study, with values of dry socket prevalence similar to or lower than those reported by other authors 2,4-6,8,14, demonstrate that such pain does not increase the frequency of dry socket.
CONCLUSION
Although dry socket is a postoperative complication that causes intense and aching pain for the patient, its prevalence was 1% in procedures performed by dentists with expertise in dento-maxillary surgery. Such prevalence, compared to international statistics, and was not higher when there was pain prior to the dental extraction