INTRODUCTION
Oral diseases are considered a global public health challenge, especially in developing countries with higher public health spending 1. Early childhood caries (ECC) is defined as the presence of decayed, missing, or filled teeth in children under 6 years old. Furthermore, The World Health Organization (WHO) stated that ECC influences children’s health, their families, and in that way, society 2. ECC is also related to nutritional troubles due to difficulty in eating, drinking, and loss of appetite. Other negative manifestations include oral symptoms such as pain and discomfort, sleep disturbances, behavioral changes, word pronunciation problems, and decreased academic performance 3,4.
Malocclusion is a major oral health problem which is the morphological and functional imbalance of the stomatognathic system between bone, muscle, and teeth. This condition generates functional troubles in mastication and deglutition, dental occlusion, and phonation. Additionally, harmful psychological repercussion was reported because of dental aesthetic appearance 5.
Oral health problems during early childhood can have a negative impact on the child's quality of life and also on the family environment. Oral health is part of overall health and it is described in the concept of Oral Health-Related Quality of Life (OHRQoL). It represents the impact of oral conditions on functional, social, and psychological well-being 6.
In Latin America, the limitations of oral health prevention and promotion policies, the inequality in access to health care, and the lack of budget are directly related to the high oral disease rates. Additionally, OHRQoL differs according to socioeconomic status and educational levels 7. Correspondingly, the WHO affirmed that oral ailments and diseases often have a greater impact on poor and vulnerable people 2. This is the case of people from Huancavelica, located in the central Andean region of Peru. Here, a high percentage of the population is living in poverty. According to the 2017 technical report, Huancavelica reached poverty rates of 33.3% and 36.8%, according to the country's poverty threshold. Thereby, people, mainly children, from Huancavelica are considered a vulnerable population 8
Currently, there are several studies evaluating oral diseases/conditions and their relationship with OHRQoL. Nevertheless, the available literature can not be extrapolated to vulnerable individuals. Thus, it is important to conduct research aimed to assess the impact of OHRQoL and oral diseases/conditions focused on vulnerable populations. This study aimed to analyze the factors associated with OHRQoL in preschool children from the Andean community of Paucarbamba, Huancavelica, Peru.
MATERIAL AND METHODS
The observational, correlational, and cross-sectional study was approved by the Ethics Committee of the Regional Hospital of Huancavelica. The sample size was calculated using the formula for estimate a proportion with a 95% confidence interval (Z=1.96), a variance (S2) of 2.25, and a absolute error/precision (e) of 0.28 (data from a previous pilot test). Therefore, a total of at least 111 patients were required. The study was conducted on 120 preschool children from 3 to 5 years old attended at Paucarbamba Health Center, Huancavelica, Peru from January to May 2019. Previously, the parents/caregivers signed informed consent. The inclusion criteria were: Children who assent to participate with the consent of parents and caregivers who speak the Spanish language, which was collected during the anamnesis. Non-cooperative patients and/or patients with systemic diseases, such as anemia and chronic malnutrition, were excluded.
The evaluator (AAHM) was calibrated with an experienced specialist, considered the gold standard (YGTG) for the dmft index variable, obtaining excellent concordance for intra- and inter-examiner (Intraclass Correlation Coefficient = 0.885 and 0.821, respectively). Furthermore, the internal consistency of the Early Childhood Oral Health Impact Scale (ECOHIS) questionnaire was good (Cronbach's Alpha=0.806).
The OHRQoL of the children and their families was evaluated with the ECOHIS questionnaire, which was addressed to the children's guardians. It consists of 13 questions which were divided into four domains for the child impact section: symptoms, function, psychological, self-image, and social interaction; and two domains for the family impact section: parent distress and family function. Questions were measured using Likert scale, with scores of 0 = never, 1 = hardly ever, 2 = occasionally, 3 = often, 4 = very often, 5 = don't know. Total scores can range from 0 to 52, and a higher score indicates a greater impact on quality of life and, consequently, worse OHRQoL 9. The ECOHIS score, which represented the OHRQoL, was the dependent quantitative variable.
The independent variables were sex, age, dmft index, presence of malocclusions, and simplified oral hygiene index (OHI-S).
ECC was represented by the dmft index, which was a quantitative variable. In addition, the severity of ECC was classified according to Hallet et al., in dmft index 0 = healthy, dmft 1-5 = low severity, and dmft ≥ 6 = high severity 10. Malocclusion was considered a qualitative dichotomous variable (presence and absence); however, types of malocclusions were reported: overjet > 3mm, anterior crossbite, anterior open bite, bis to bis bite, and anterior deep bite (overbite > 40%) 11.
OHI-S proposed by Greene and Vermillion using dental plaque revealer (Plac Control®) was recorded on the dental surfaces: 5.5 vestibular (v), 5.1 (v), 6.5 (v), 7.5 lingual (l), 7.1 (v), and 8.5 (l) 12. Furthermore, the OHI-S was considered a quantitative variable and, additionally, was utilized to divide the clinical level of oral hygiene into good (OHI-S: 0.0 - 1.2), regular (OHI-S: 1.3 - 3.0), and bad (OHI-S: 3.1 - 6) 12.
The data obtained were stored and processed using STATA v16. Univariate and bivariate analyses were performed. The ECOHIS score was expressed as mean, median, and confidence intervals (95% CI). Spearman's correlation test was used due to the lack of normality in the OHRQoL (quantitative variable). A multiple linear regression model using the least squares method was used.
RESULTS
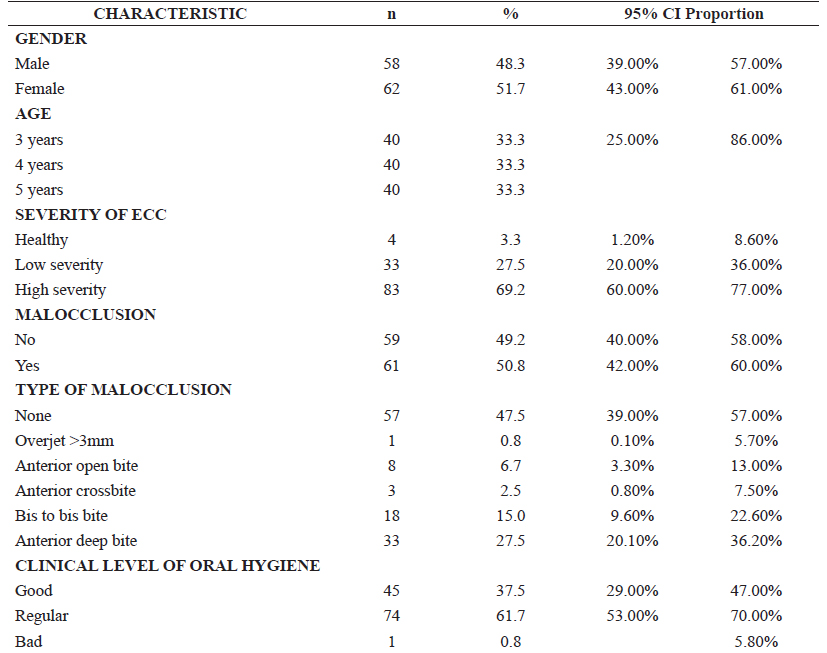
The sample (n=120) was distributed by gender, age, and oral diseases/conditions among patients such as malocclusions, the severity of ECC, and OHI-S. The female sex represented 51.7% of individuals. High severity of ECC was found in 69.2% of the participants. 50.8% of the children had some type of malocclusion and, among them, deep bite (27.5%) and bis to bis bite (15%) represented the highest percentages. The most common clinical level of oral hygiene was regular with 61.7% of patients (Table 1).
Regarding the scores obtained from the ECOHIS questionnaire, no differences (p>0.05) were found among categories grouped by gender, severity of ECC, presence, and type of malocclusion, and clinical level of oral hygiene (Table 2).
Table 2 Bivariate statistics comparing the average scores obtained from the ECOHIS of parents/caregivers of children between 3 and 5 years old by categories of adjustment variables (n=120).
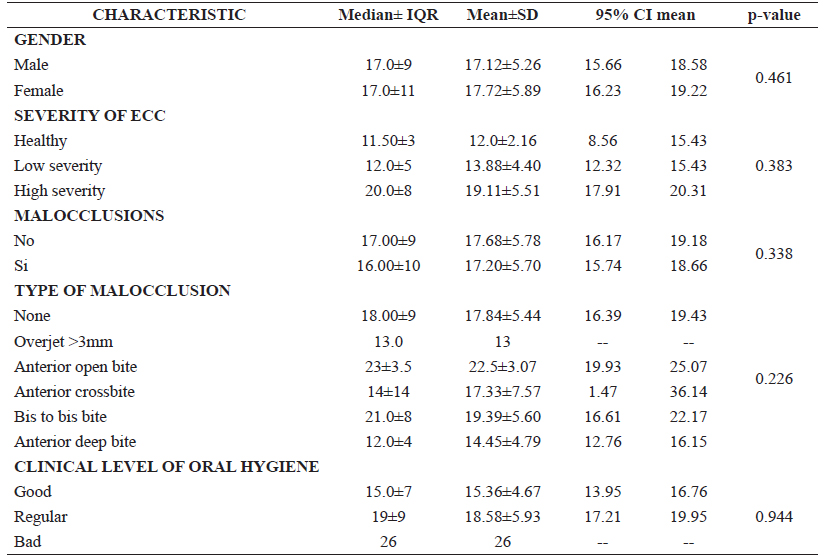
SD: Standard deviation; IQR: Interquartile range
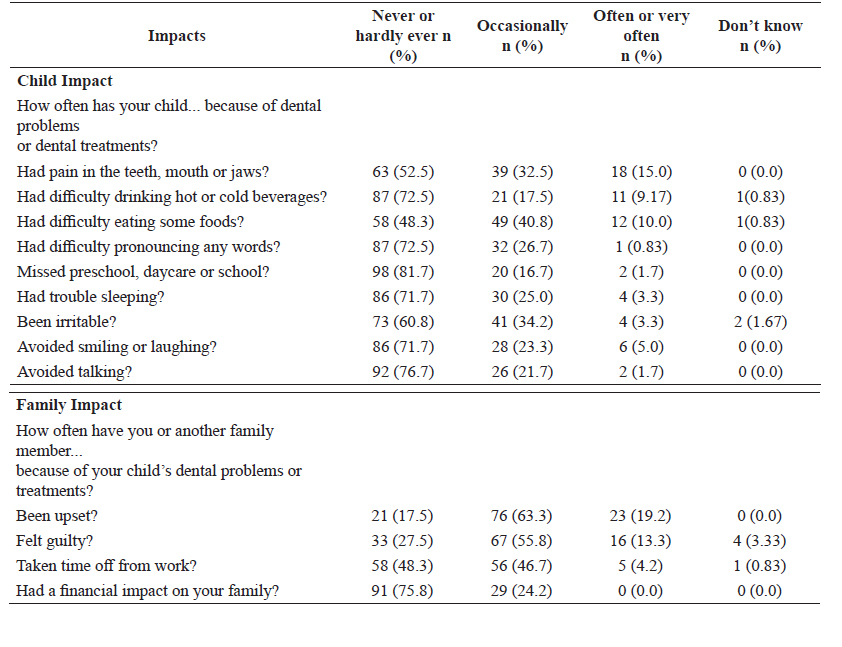
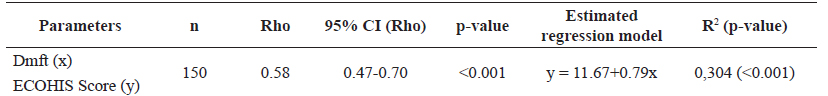
Table 3 displays the responses to each item in the ECOHIS questionnaire, which were divided into the child and family impact assessment and were reported by the caregiver. Table 4 shows that the dmft index values and the ECOHIS score presented a positive and moderately significant relationship (95% CI, rho value: 0.47 - 0.70, p<0.001).
The least squares method for multiple regression considered the contribution of the dmft index as significant (p<0.05) to explain the ECOHIS score. Other variables did not show a significant association with impact on OHRQoL (Table 4). The estimated regression model was ECOHIS Score = 11.67+0.79*dmft, in which for each increase of a unit of dmft index, the ECOHIS score gained 0.79 points. The variability of the obtained score was explained by the dmft in R2=30% (p<0.001).
DISCUSSION
This study analyzed oral health status and its relationship with quality of life in 3- to 5-year-old children and their families from a vulnerable population of the Central Andean area of Peru. It was observed that the ECC can significantly affect children´s OHRQoL owing to its consequences.
OHRQoL was measured using the ECOHIS questionnaire, which was developed by Pahel et al., and the latter demonstrated to have validity, internal consistency, and reliability 9. In addition, the validation and cross-cultural adaptation of this instrument for a population of Peru were established by Lopez et al. 11. Higher ECOHIS scores denote greater oral health impact or poorer OHRQoL. In the present study, the responses of the ECOHIS questionnaire were “never/hardly ever” (59.8%), “occasionally/often/very often” (39.6%), and “don't know” (0.6%); in comparison with the results shown by Pahel et al. of 90.2%, 8.5%, and 1.3% (9); and by Contaldo et al. of 77.7%, 20.8%, and 1.5%, respectively 13. Our findings showed a lower percentage of caregivers who answered "never/hardly ever" and "don't know", and a higher percentage who answered "occasionally/often/very often" compared to the other studies 9,13. This result was probably due to the different impact of dental caries in these Peruvian children or the different number of participants considered here.
The evaluated clinical parameters were the dmft index (ECC), malocclusions, and OHI-S. The prevalence of ECC (96.7%) in preschool children differed from those reported by the Peruvian Ministry of Health (MINSA) (59.1%) (14), probably, because the latter included both urban and rural populations, and here we assessed only rural children. Likewise, here, the ECC was found more frequently than in other studies: Rajab et al. with 76% of Jordanian preschool children 15, Contaldo et al. with 44.8 % of Italian preschool children 13, and compared to other Peruvian children with 76.5% 16. In the aforementioned studies, the dmft index was used. Furthermore, Pesaressi et al. employed the Caries Assessment Spectrum and Treatment (CAST) index in 3-year-old children from Lima, Peru, and a high prevalence was obtained (93.4%) 17. It was similar to our results.
Regarding the malocclusions, Lopez et al. obtained a lower prevalence (6.54%) than the result presented here (50.8%). The diversity of these findings may be due to the heterogeneity of the populations and the sample size of each study. Besides, in the latter study, they only assessed the presence or absence of malocclusion 16). In the present research, we additionally reported the types of malocclusions.
In this investigation, there was no association between the presence of malocclusion and OHRQoL. Similar results were reported by other studies 3,16. On the contrary, Firmino et al. reported that the anterior open bite was positively associated with OHRQoL but with an impact only on the family 18.
Considering oral hygiene, regular clinical level (OHI-S: 1.3 - 3.0) was the most common; contradicting the expected data of greater predisposition of patients with bad oral hygiene (OHI-S: 3.1 - 6), considering the high severity of ECC.
Some systematic reviews demonstrated that lower children’s age and gender (girls vs boys) were associated with a negative impact on OHRQoL among children 19,20. Nevertheless, in the present study, we did not obtain that association.
Overall, the expected results were that all variables (gender, age, dmft, presence of malocclusion, and OHI-S) were directly associated to OHRQoL in this population. The multifactorial analysis, which explained the variability of the ECOHIS score, showed a significant contribution only of the ECC, represented by the dmft index. Accordingly, various studies have shown that the impact on quality of life, using ECOHIS questionnaire, was associated with ECC 3,4,21-23. In addition, one systematic review showed that children with more dental caries were 1.66 times more likely to have poor OHRQoL (OR = 1.66, 95% CI = 1.43, 1.88) 19.
Regarding study limitations, the execution time limited the evaluation of clinical parameters such as the risk of caries, hypomineralization, dental trauma, and another type of tooth structural anomaly. Besides, the difficult geographical access and the lack of resources did not allow the evaluation of other health centers across the Region. Although the majority of the population here were Quechua speakers, most of them speak and/or understand Spanish. Caregivers who did not speak or understand the Spanish language were excluded from the study to avoid response bias.
In conclusion, there was an association between ECC and OHRQoL of the children and their families in an Andean Community in Paucarbamba, Peru. Furthermore, in the present study, there was not found any significant association between gender, age, malocclusion, OHI-S and the OHRQoL.
Considering that ECC impacted negatively on OHRQoL, better health promotion and prevention strategies are necessary, in order to achieve a real improvement in the quality of life of this vulnerable population. Reorganization of primary oral health care, expansion and qualification of specialized care, qualification of teachers and children caregivers regarding oral health education, and evaluate the feasibility of adding fluoride in the daily diet could be some of the possible solutions based on other national health policy 2,24,25
Finally, further studies should consider other factors such as geographic accessibility, poverty rates, educational level, and limited access to health information. Currently, there is no cross-cultural adaptation and validation of the ECOHIS questionnaire to the Quechua language and we strongly believe that future studies should center on that. In addition, more longitudinal clinical studies focused on vulnerable populations such as the one analyzed in this study are needed.