INTRODUCTION
Aneurysmal Bone Cysts (ABC) are uncommon, intraosseous, benign conditions that mostly affect the mandible's posterior region and ascending branch but can also affect the head and neck 1,2. The World Health Organization (WHO) describes it as an expanding lesion with septa made of connective tissue, multinucleated giant cells, and osteoid tissue, as well as blood gaps of various diameters 1-3.
The etiopathogenesis of aneurysmal bone cysts is highly debated, and according to the majority of reports, trauma history is the primary causative factor, followed by vascular abnormalities 3 and other factors. The same causative factors 4,5 are not present. ABC in the jaws can present radiographic variations, making it difficult to interpret the initial image exams that will guide the planning and subsequent treatment because there is a lack of specificity in the clinical and radiographic appearance 1,5.
The majority of research focuses on describing clinical cases that discuss clinical, radiological, and potential treatments in general 2,3. Since only 1% to 2% of ABC of the jaws have reports detailed in the literature, few studies reports and correlate a specific pattern of image inspection, such as Computed Tomography (CT), to close an accurate diagnosis with more precision and recommend a workable treatment strategy 4.
Although establishing a standard for the clinical status and behavior of a disease is made easier by studying the pathogenic process, it is feasible to approach a model that makes recommendations by looking at the cases recorded in recent years. The goal of this study was to analyze the available literature in this area to determine which imaging exams are most frequently requested and their characteristics.
MATERIAL AND METHODS
The review question “What are the most requested imaging exams in the management of Aneurysmal Bone Cyst?” was established and the PECO strategy (Population, Exposition, Comparison and Outcome) were defined as: P - patients with ABC; E - 2D and/or 3D imaging exams such as CT, Cone-Beam Computed Tomography and Magnetic resonance imaging and panoramic radiography C - not applicable; and O - efficacy of imaging exams in the diagnosis and treatment of ABC.
We searched the databases PubMed, Web of Science, and Scopus. A search/study strategy was carried out with Boolean operators (OR/AND) and the keywords used were: “Aneurysmal Bone Cysts”, “Jaws” and “Imaging diagnostic”. The following search/study strategy was applied to the databases: (Bone Cysts, Aneurysmal OR Aneurysmal Bone Cysts OR Bone Cyst, Aneurysmal OR Cyst, Aneurysmal Bone OR Cysts, Aneurysmal Bone) AND (Maxilla OR Maxillae OR Maxillary Bone OR Mandible OR Jaw OR Jaws) AND (Radiological OR Imaging diagnostic OR Panoramic Radiography OR intraoral radiography OR Cone-Beam Computerized Tomography OR Computerized Tomography).
Selection criteria
Studies that were written in both Portuguese and English were included. The last ten years (2010 to 2020) were the only years that were considered for the article selection. Case reports or case series of ABC in the mandible or maxilla were included in the papers, along with details on the initial clinical signs, imaging tests, and ultimate diagnosis. Case reports that lacked details regarding the conduction, lacked ABC confirmation, or were written in a language other than English or Portuguese were disregarded.
A narrative data synthesis was performed for this review, and the following data from the included studies were collected: authors, year of publication, clinical features, what type of imaging exam was used to identify the lesion, whether another complementary imaging exam was performed, treatment of choice, recurrence, and follow-up time.
RESULTS
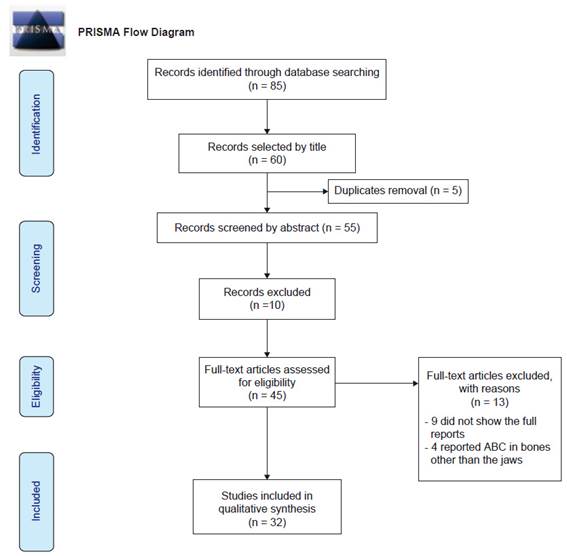
The literature search showed 85 articles, of which 58 were chosen by title and sent to the EndNote platform. 45 of the 55 abstracts were chosen for the full-text reading after the duplicates were eliminated. Nine of them omitted the entirety of the reports, and four of them reported ABC in bones other than the jaws. 32 articles were therefore included in this review. Case reports and case series were considered in this review. The PRISMA flow chart in Fig. 1 displays the outcomes. Table 1 presents a summary of the research and its conclusions.
Table 1 Summary of the studies.
| Study | Age/ Gender | Location | Clinical features | First choice of imaging exam | Complement imaging exame | Treatment of choice | Follow-up | Recurrence |
|---|---|---|---|---|---|---|---|---|
| Álvarez-Martínez et al. | 27/M | Mandible | Edema | PR | CT | Curettage | 2 years | No |
| Arango-Fernandez et al. | 8/M | Mandible | Edema | PR | None | Curettage and resection after the recurrence | 1.6 years | Yes |
| Baldo et al. | 7/F | Mandible | None | PR | CT | Embolization | 3 years | No |
| Behal et al. | 40/F | Mandible | Edema | PR | CT | Surgical resection | Not reported | Not reported |
| Bhandari et al. | 17/M | Mandible | Edema | PR | CT | Surgical resection | 3 years | No |
| Costa de Freitas et al. | 6/M | Mandible | Pain | CT | MRI | Bone marrow injection | 5 years | No |
| Devi et al. | 27/M | Mandible | Edema | PR | CT | Curettage | 1 year | No |
| Gabric et al. | 11/F | Mandible | Edema | PR | CT | Curettage and resection after the recurrence | 1.6 years | Yes |
| Hebbale et al. | 10/F | Mandible | Edema | PR | CT | Curettage | Not reported | No |
| Henriques et al. | 13/F | Maxillae | None | PR | None | Curettage | Not reported | Yes |
| 13/F | Mandible | Edema | PR | None | Curettage | Not reported | Yes | |
| 33/F | Mandible | None | PR | None | Curettage | Not reported | No | |
| 17/M | Mandible | Edema | PR | None | Curettage | Not reported | No | |
| 14/F | Maxillae | None | PR | None | Curettage | Not reported | No | |
| 5/F | Mandible | None | PR | None | Curettage | Not reported | No | |
| 11/M | Mandible | None | PR | None | Curettage | Not reported | No | |
| 12/F | Mandible | Edema | PR | None | Curettage | Not reported | No | |
| 11/M | Mandible | None | PR | None | Curettage | Not reported | No | |
| Kilic et al. | 3/M | Mandible | Edema | CT | None | Surgical resection | Not reported | Not reported |
| Lee | 38/F | Maxillae | Edema | CT | MRI | Surgical resection | 1.3. year | No |
| Li et al. | 24/F | Mandible | Nasal obstruction | CT | None | Radiotherapy and surgical resection | 9 months | No |
| Marchetti | 15/F | Mandible | Edema and Pain | PR | None | Curettage | 1 year | Yes |
| 40/M | Mandible | Edema | PR | CT | Curettage and resection after the recurrence | 5 years | Yes | |
| 47/M | Mandible | Edema | PR | CT | Curettage | 1 year | No | |
| McMullen | 14/F | Maxillae | Edema and paresthesia | CT | MRI | Surgical resection | 2 months | No |
| Möller et al. | 14/M | Maxillae | Edema | PR | CT, MRI | Curettage | Not reported | Not reported |
| Omami et al. | 33/F | Mandible | Edema | PR | CBCT, MRI | Embolization and surgical resection | Not reported | Not reported |
| Parashari et al. | 11/M | Mandible | Edema | MRI | None | Surgical resection | Not reported | Not reported |
| Rațiu et al. | 73/F | Mandible | Pain | Periapical | PR, CBCT | Curettage | Not reported | Not reported |
| Saad et al. | 40/M | Maxillae | None | PR | CBCT, MRI | Curettage | 2 years | No |
| Santana Santos et al. | 42/F | Mandible | Edema | PR | CT | Surgical resection | 5 years | No |
| Sarode et al. | 10/M | Maxillae | Edema | PR | CT | Surgical resection | 3 years | No |
| Seo-Young et al. | 9/F | Mandible | Edema | PR | CT | Embolization and curettage | 5.7 years | No |
| Smolka, W. et al | 16/F | Maxillae | Edema and Pain | PR | CT, MRI | Surgical resection | 7 months | No |
| Arora et al. | 6/F | Mandible | Edema | CT | None | Curettage | Not reported | Not reported |
| Triantafillidou et al. | 17/F | Maxillae | Edema | PR | None | Curettage and resection after the recurence | 17 years | Yes |
| 18/F | Maxillae | Edema | PR | CT | Curettage | 8 years | Yes | |
| 21/M | Maxillae | Edema | PR | CT | Surgical resection | 6 years | No | |
| 35/F | Mandible | Edema | PR | None | Curettage | 5 years | No | |
| 28/F | Mandible | Edema | PR | None | Curettage | 4 years | No | |
| 32/M | Mandible | Edema | PR | None | Curettage | 2 years | No | |
| Urs et al. | 50/M | Mandible | Edema | PR | None | curettage | 1.5 year | No |
| 35/M | Mandible | Edema | PR | None | Curettage | 1.5 year | No | |
| 10/F | Maxillae | Edema and pain | PR | None | Curettage | 1.5 year | No | |
| 13/F | Mandible | Edema | PR | None | Curettage | 1.5 year | No | |
| 10/M | Mandible | Edema | PR | None | Curettage | 1.5 year | No | |
| 14/F | Mandible | Edema and pain | PR | CT | Surgical resection | 1.5 year | No | |
| 13/F | Mandible | Edema | PR | None | Curettage | 1.5 year | No | |
| Westbury et al. | 17/F | Mandible | Edema and pain | PR | MRI, US, CT | Surgical resection | 7 months | No |
| Woo et al. | 27/F | Mandible | Edema and pain | PR | None | Curettage | 6 months | No |
| Yeom et al. | 32/F | Mandible | none | PR | CBCT | Curettage | 1 year | No |
| Zadik et al. | 37/F | Mandible | Edema | PR | CBCT | Surgical resection | 5 years | No |
| Ziang et al. | 19/F | Mandible | Edema | PR | CT | Curettage and resection after the recurrence | 6 months | Yes |
Notes: M (male), F (female), PR (panoramic radiography), CT (computed tomography), MRI (Magnetic resonance imaging), US (ultrasound), CBCT (cone-beam computed tomography).
A total of 53 cases were included, of which 20 (37.7%) were male and 33 were female (62.3%); the ages were divided into 0-10 (11 cases - 20.8%), 11-20 (21 cases - 39.6%), 21-30 (6 cases - 11.3%), 31-40 (11 cases - 20.8%) and >40 (4 cases - 7.5%) (Table 2); 41 of the cases reported occurred in the mandible (77.4%) and 12 in the maxillae (22.6%). The edema appeared in 34 cases (64.2%), 6 cases (11.3%) had edema and pain, only 2 cases (3.8%) had pain involved, 1 case (1.9%) had edema and paresthesia, 1 case (1.9%) had a nasal obstruction, and 9 cases (16.9%) were without symptoms (Table 3).
Table 2 Patients characteristics.
| Features | Number of patients | % |
|---|---|---|
| Male | 20 | 37.7% |
| Female | 33 | 62.3% |
| Age (0-10) | 11 | 20.8% |
| Age (11-20) | 21 | 39.6% |
| Age (21-30) | 6 | 11.3% |
| Age (31-40) | 11 | 20.8% |
| Age (>40) | 4 | 7.5% |
Table 3 Clinical features.
| Clinical features | Number of patients | % |
|---|---|---|
| Located in mandible | 41 | 77.4% |
| Located in maxillae | 11 | 22.6% |
| Edema | 34 | 64.2% |
| Pain | 2 | 3.8% |
| Edema and pain | 6 | 11.3% |
| Edema and paresthesia | 1 | 1.9% |
| Nasal obstruction | 1 | 1.9% |
| No symptoms | 9 | 16.9% |
Panoramic radiography (PR) was the primary imaging exam needed to analyze the lesion, accounting for 45 (84.9%) of the cases, while only 6 (11.3%) patients selected computerized tomography (CT) as their first exam of choice. Additionally, periapical radiographs (1.9%) and MRIs were performed in 1 case each in 1.9% of the instances (Table 4). In PR, 26 claimed to be a multilocular lesion, while 14 reported a unilocular lesion; 13 of the instances did not specify the characteristics. To assess the extent of the lesions as well as their behavior, such as fluid levels, which may be observed using Magnetic resonance imaging (MRI), 23 (43.4%) of the cases that initially underwent the PR required a supplemental imaging exam. Thus, 2 instances wanted CBCT, 2 cases requested CBCT and MRI, 2 cases requested CT and MRI, and only 1 case requested three complimentary exams (CT, MRI, and US). Of these cases, 16 sought CT as a second exam. The other 22 instances that called for initial panoramic radiography opted not to have any additional testing. Three of the six cases where CT was sought as part of the initial evaluation in terms of 3D images requested an MRI as an additional test. In the one instance where periapical radiography was used as the initial examination, CBCT and PR were sought as further tests. In every single CT case (100%), the lesion was described as osteolytic with fluid levels and cortical expansion.
Table 4 First choice of imaging exam
| Exam | Number of cases | % |
|---|---|---|
| Panoramic Radiograph | 45 | 84.9% |
| CT | 6 | 11.3% |
| MRI | 1 | 1.9% |
| Periapical | 1 | 1,9% |
Each case's ABC therapies are unique, primarily due to the size of the lesion. Although embolization is a modality that has only recently been described in the literature, only 1 case chose to perform it exclusively, while the other 2 cases chose to use it before the open surgery, ensuring a lower risk of excessive bleeding (Table 5). In 35 cases (66%) curettage was the treatment of choice, while 13 cases (24.5%) chose to go with resection of the part involved. However, resection was required in five cases where recurrence occurred following curettage. Additionally, one patient chose radiotherapy to reduce the size of the lesion and ensure complete excision because it happened to be too large.
Table 5 Treatment of choice.
| Treatment | Number of cases | % |
|---|---|---|
| Curettage | 35 | 66% |
| Resection | 13 | 24.5% |
| Exclusive Embolization | 1 | 1.9% |
| Bone marrow injection | 1 | 1.9% |
| Radiotherapy | 1 | 1.9% |
| Embolization + Curretage or Surgical Resection | 2 | 3.8% |
In 17 cases (32%), the follow-up time was not reported. In 36 cases (68%), the follow-up period was documented, with means ranging from 34.1 to 37.2 months (median 18 months). Nine cases (16.9%) of curettage patients from the studied articles showed recurrence after 6 months to 17 years of follow-up, and five of these cases only underwent surgical planning by PR. In addition, four instances initially asked for a complimentary PR and CT exam. However, in 7 cases (13.2%), it was not stated whether the lesion had returned or not.
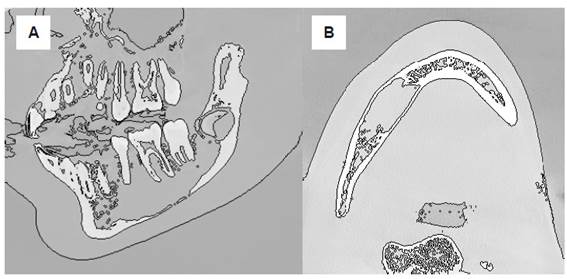
Histopathological investigation confirmed all instances, and 10 (18.8%) were associated with other lesions such as Juvenile Ossifying Fibroma, Fibrous Dysplasia, and other Fibro-osseous lesions. Figure 2 illustrates the features of an ABC in young patient.
DISCUSSION
Because of their unpredictable presentation, aneurysmal bone cysts (ABC) are frequently referred to as mysterious lesions 1-11. There are case reports of asymptomatic lesions discovered during a routine radiography check as well as aggressive, quickly growing masses that cause edema and pain that can be found in the literature. Since the clinical manifestations and radiographic tests cannot explain the ABC hypothesis, a biopsy should be required to confirm the diagnosis 12-16. Because it is less invasive (fine needle) and, even though it does not provide enough information to confirm an ABC lesion, the fine-needle aspiration biopsy (FNAB) is typically the method of choice in cystic lesions of unknown origin 15.
The primary method used to investigate oral and maxillofacial diseases is a panoramic radiograph. ABC is typically described as a multiple or single radiolucent lesion with distinct margins and hardly noticeable cortical enlargement. Other cystic lesions that are common to the maxillary complex, such as single bone cysts, central giant cell lesions, and keratocytes 14, may have the same characteristics. It can be sufficient to establish a firm diagnosis of ABC when combined with the clinical data and biopsy findings. However, other imaging modalities, such as computed tomography (CT) and magnetic resonance imaging (MRI), can aid in the diagnosis process by revealing the density of the lesion and fluid-fluid levels, which can help avoid surprises in the cystic cavity during lesion management, such as extensive bleeding 14,16.
An ABC in CT is characterized by a hypodense lesion with definite outlines, resembling an "eggshell," and it is frequently easy to discern an extension of the cortex of the neighboring bone, septa, fluid levels, or even vascularization on severe lesions. Since patients with indications and symptoms consistent with osteolytic lesions on face bones are brought to hospitals, the CT exam is the most reported exam after panoramic radiography. However, because of its lower dosage of radiation and less expensive equipment, Cone Beam Computed Tomography (CBCT) should be the referring technique in situations of oral and maxillofacial diseases. Furthermore, some studies have found that gray values acquired by CBCT are higher than gray values obtained by conventional CT of the same location, suggesting that it may be more convenient than multislice computed tomography for the examination of bone abnormalities of the jaws such as cysts or tumors 17.
CT can help throughout treatment in addition to greatly assisting in the diagnosis of an ABC. Despite its etiopathogenic and radiographic similarities with a solitary bone cyst (SBC), the management of ABC is not conservative. While the SBC can be preserved via routine follow-ups and addressed with exploratory surgery, the ABC can grow aggressively, leading to pathological fractures and vascular problems. Curettage is known as an incomplete form of treatment since it frequently results in recurrence, particularly when the position of the lesion precludes a complete operation and there are concerns from medical professionals regarding the nerves around the cyst. Further, several authors have found success using CT to guide the procedure due to its size and position, ensuring clear margins, limiting nerve or microvascular injury, and yet building a 3D model for the costochondral graft 15,18.
It is possible to see the vascular components of the ABC with advanced imaging tests like MRI, ultrasound, and angiography, after which one can select less invasive procedures like embolization or even more cutting-edge ones like bone marrow injection. In cases where embolization was the initial treatment, MRI, CBCT and MRI, or simply CT, were employed. Although understanding the function of the cyst's vascular component cannot ensure treatment success, it can help prevent mistakes like excessive bleeding during surgery.
Sclerotherapy, which is typically applied to long bones, is one of the minimally invasive treatments that have been used. A 7-year-old girl with an ABC in her mandible underwent percutaneous embolization, and Baldo et al., 2019, reported the results of a 3-year follow-up. All the permanent teeth included in the therapy have remained healthy so far. The CT was nevertheless necessary to comprehend how the sclerotic agent operated on the post-operative patient. Additionally, an innovative, minimally invasive option to treat ABC may involve injecting autologous bone marrow, according to a recent study 11. There was successful therapy with a 5-year follow-up without recurrence after investigating the cyst using CT, RMI, and angiography. Again, an uneventful post-op was only achievable with the assurance of a 3D imaging evaluation 11.
CONCLUSION
One weakness of this study is that some instances did not specify the period of follow-up or whether there was recurrence, making it impossible to identify a pattern about care (from diagnosis to therapy) vs. outcome. This type of information is essential for further research. Although a 3D imaging scan provides the surgeon with a better picture of the extent of the lesion, it cannot guarantee that it is sufficient to avoid recurrence, as there have been situations where surgical planning established using CT or MRI recurred. Even if these exams provide a 3-dimensional awareness of the lesion's limitations, the experience of the professional who will evaluate the exam and perform the operation may be the key to avoiding recurrence.