INTRODUCTION
Bell's palsy (BP) is a disorder affecting the lower motor neuron associated with the facial nerve. Individuals afflicted with this condition experience unilateral facial paralysis and a reduced ability to taste on the anterior part of the tongue. The incidence of BP is estimated at between 15 and 30 new cases per year per 100,000 individuals, predominantly affecting young and middle-aged adults aged 15 to 40 years 1
BP is diagnosed clinically and assessed using the House-Brackmann (HB) scale, a standardized tool that measures the extent of nerve damage in facial palsy from I, indicating normal function, to VI, which represents total paralysis 2 Corticosteroid therapy, possibly combined with antiviral medications, along with physical therapy, acupuncture, massage, and neuromuscular facilitation are commonly employed treatments for BP 3 Low-level light therapy (LLLT) is also mentioned in the literature as a treatment method 4 The effectiveness of LLLT, and with or without alternative therapies has been discussed in the literature due to its modulating action, non-invasiveness, painlessness, and lack of adverse effects 5 However, there is little relevant evidence to consider LLLT effective in improving BP, requiring further study.
This study aimed to report three clinical cases where LLLT was used as an adjuvant treatment for BP. Concurrently, a literature review was conducted that included published cases of BP treated with LLLT to analyze the laser-based protocols and their respective efficacies.
CASES PRESENTATION
This study and the following case reports were conducted at the Stomatology Clinic of the Bauru School of Dentistry, University of São Paulo.
Case 1
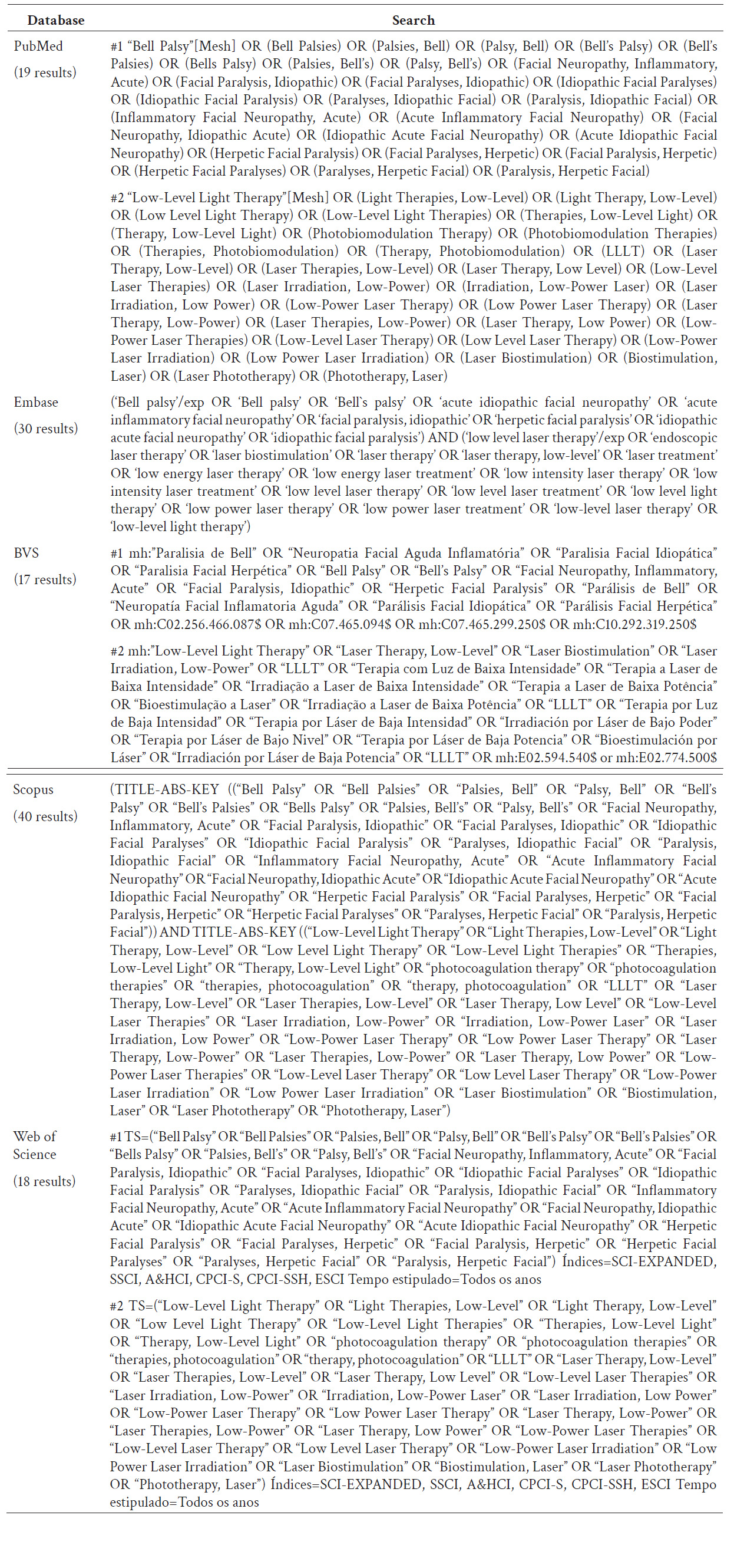
A 52-year-old Brazilian Caucasian woman, exhibiting right-sided facial paralysis, was diagnosed with BP one week prior to her evaluation and is currently under the care of a neurologist. Her medical history includes gastritis and stress, and she has used acyclovir for 7 days and Alendronato® for 1 year due to pain upon manipulation of the sternocleidomastoid muscle, ipsilateral to the BP. She reported using prednisone 20 mg, Velija®, lubricating eye drops, omeprazole 20 mg, and Nevrix®. On an extraoral physical examination, she presented with facial paralysis on the right side (figure 1A), with the paralysis ipsilateral to the labial protrusion (figure 1B), elevation of the eyebrows (figure 1C), and incomplete closure of the right eye (figure 1D). This presentation was compatible with the diagnosis of BP, which was classified as grade V (severe dysfunction) according to the HB scale. The intraoral physical examination showed no changes.
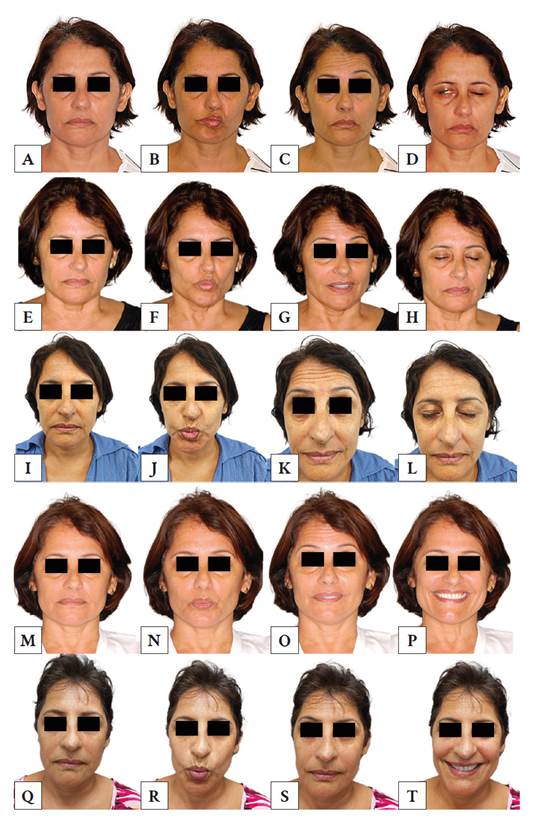
Figure 1 Clinical evolution of Bell’s palsy treated with low-level light therapy. First session: facial asymmetry at rest (A), labial protrusion (B), eyebrow elevation (C), and partial occlusion of the right eyelid (D). Third session: partial improvement of right lip paralysis due to labial protrusion (F), improvement in eyebrow elevation (G), and complete eyelid occlusion (H). Fourth session: significant improvement in facial asymmetry at rest (I), lip protrusion (J), and eyebrow asymmetry (simultaneous elevation) (K). Sixth session: more symmetrical profile and improvement in the disproportionate lip protrusion (N). Seventh session (last): significant improvement in all facial expressions, greater symmetry at rest (Q), and improvement in lip protrusion (R), eyebrow elevation (S), and smile (T).
In view of the diagnosis of BP, the adjuvant therapeutic approach to medical treatment consisted of LLLT (780 nm; 70 mW; 157.5 J/cm2; E = 9 J; t = 1 minute and 30 seconds), using the Twin Laser device (MM Optics, São Carlos, SP, Brazil), applied along the path of the facial nerve on the right side of the face. The next day, the patient returned for the second LLLT session with no complaints and no clinical signs of improvement in facial asymmetry. However, from the third session onwards, signs of muscle movement recovery appeared, such as a reduction in the inclination of the lips to the left upon labial protrusion (figure 1F), more symmetrical eyebrow elevation (figure 1G), and complete eyelid occlusion (figure 1H).
A total of seven LLLT sessions were carried out over 21 days, with intervals between sessions ranging from 1 to 7 days. Initially, the patient reported sensations of tingling, jerking, and shock during LLLT application. During the fifth session, she experienced needling sensations in the pre-auricular region. In the sixth session, she reported pain upon palpation of the temporalis, masseter, and sternocleidomastoid muscles, accompanied by a severe headache on the right side; Alginic® was administered by the neurologist.
In the last consultation, the patient was no longer using prednisone, had no complaints, and was satisfied with the results, as seen in figure 1 (Q, R, S, and T). Consequently, this led to significant improvements in her facial function and aesthetics. Therefore, after treatment, BP was reclassified as grade II, indicating mild dysfunction according to the HB scale.
Case 2
A 37-year-old Brazilian Caucasian man, an artisan with a previous diagnosis of BP, reported visiting the emergency room three months prior to the study due to tingling in his tongue, pain in the occipito-parietal region, and a headache. He was later diagnosed with BP on the right side, possibly related to stress and heat shock. He reported having the first episode 10 years earlier, achieving complete remission after the treatment was completed.
His medical history revealed a mercury allergy and a testicular tumor resection 10 years earlier, which was why he was continuously treated with 1 g of finasteride, topical minoxidil, and Silimalon®. For the treatment of BP, he received acyclovir 400 mg, prednisone 20 mg, and three intramuscular doses of vitamin B12. He was also undergoing physical therapy, acupuncture, and electrical stimulation therapy, without any significant recovery in facial expressions.
During the extraoral physical examination, facial paralysis was observed on the right side, showing facial asymmetry at rest (figure 2A), immobility of the lips and eyelid when smiling (figure 2B), and incomplete occlusion of the eyelids (figure 2C). This presentation was consistent with a diagnosis of BP grade V, according to the HB scale. The intraoral physical examination revealed a traumatic ulcer of approximately 2 mm on the lower lip.
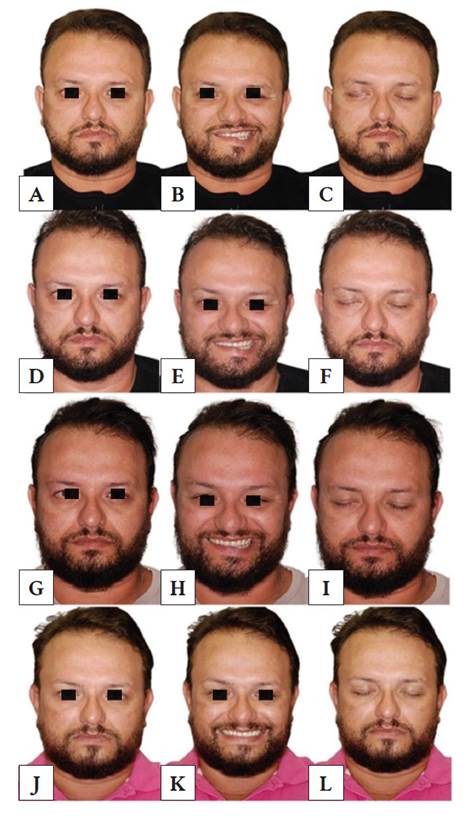
Figure 2 Clinical evolution of Bell’s palsy treated with low-level light therapy. First session: facial asymmetry at rest, as seen by the depression of the labial commissure on the right side when compared to the left (A), labial and right eyelid immobility when smiling (B), and incomplete occlusion of the right eyelid (C). Seventh session: partial improvement at rest (D) and complete occlusion of the right eyelid (F). Nineteenth session: improvement in labial and eyelid asymmetry on the right side when smiling (H), as compared with the left side and previous sessions. Twenty-fourth session (last): significant improvement in all facial expressions at rest (J), smiling (K), and occlusion of the eyelid (L).
The treatment consisted of 24 LLLT sessions (780 nm; 70 mW; 105 J/cm2; E = 9 J; t = 1 minute - Twin Laser device, MM Optics, São Carlos, SP, Brazil) along the path of the facial nerve as an adjuvant treatment for BP. These sessions were conducted over a period of 4 months with intervals of 2 to 3 days between sessions in the first month, ranging between 2, 4, and 5 days in the second month, and between 4, 5, 7, 8, 14, and 29 days in the last 2 months.
In light of the progress of BP by the seventh session, Etna® was prescribed for 30 days as an adjuvant to LLLT. During the 19th session, the patient returned, complaining of xerophthalmia, and was referred for evaluation and ophthalmological management. Upon returning for the 20th session of LLLT, the patient no longer complained of xerophthalmia but reported sensations of jerking, tingling, and itching during the laser applications, which persisted until the final session.
In his final consultation, the patient reported satisfaction with the treatment, which significantly improved his facial function and aesthetics, as observed in figure 2 (J, K and L). He progressed from BP grade V to grade II, characterized as mild dysfunction, according to the HB scale.
Case 3
A 40-year-old Brazilian Caucasian man sought medical attention for right-sided facial paralysis. He visited the emergency room and later saw an otolaryngologist five days prior. Audiometry was performed, confirming the diagnosis of BP, likely triggered by an intense period of stress. His medical history included the use of Benerva®, Prednisone, Acyclovir, Lacrima® Plus, and Elitezan®, as recommended by the otolaryngologist.
During the extraoral physical examination, he exhibited hemifacial paralysis, immobility of the nose and lips, and difficulty closing the right eye, with noticeable asymmetry even at rest. He reported a lack of sensitivity on the right side, as seen in figure 3 (A, B, C, and D). This presentation was consistent with a diagnosis of BP grade V, according to the HB scale. The intraoral physical examination showed no changes.
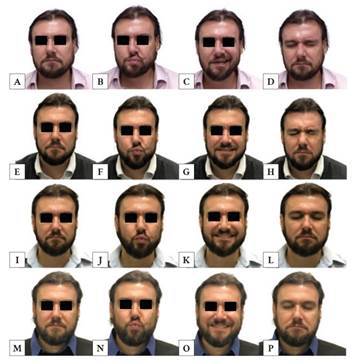
Figure 3 Clinical evolution of Bell’s palsy treated with low-level light therapy. First session: facial asymmetry at rest (A), labial protrusion (B), smiling (C), and difficult occlusion of the right eyelid (D). Fourth session: slight improvement of right lip paralysis due to labial protrusion (F), slight improvement in smiling (G), and complete eyelid occlusion (H). Sixth session: significant improvement in facial asymmetry at rest (I), lip protrusion (J), smiling (K), and complete eyelid occlusion (L). Eighth session (last): Complete improvement in all facial expressions like symmetry at rest (M), in lip protrusion (N), smile (O), and eyelid occlusion (P).
The adjuvant therapy consisted of LLLT (780 nm; 70 mW; 157.5 J/cm2; E = 9 J; t = 1 minute and 30 seconds - Twin Laser device, MM Optics, São Carlos, SP, Brazil) along the path of the facial nerve on the right side of the face. This protocol was administered twice a week for 1.5 months. In the second session, the patient reported experiencing a severe headache over the past 2 days, which improved with the use of Neosaldina®.
After the 6th session of LLLT, the patient reported significant improvements in taste, swallowing capacity, speech, and eye closure (figure 3 I, J, K, and L), with no further headaches reported and continued improvement in facial movements. By the end of 8 sessions of LLLT, all symptoms had completely disappeared, and there was full regression of BP signs (figure 3 M, N, O, and P). The patient progressed from BP grade V to grade I, indicating normal facial nerve function, according to the HB scale.
COMPARATIVE ANALYSIS OF PUBLISHED CASES OF BP TREATED WITH LLLT
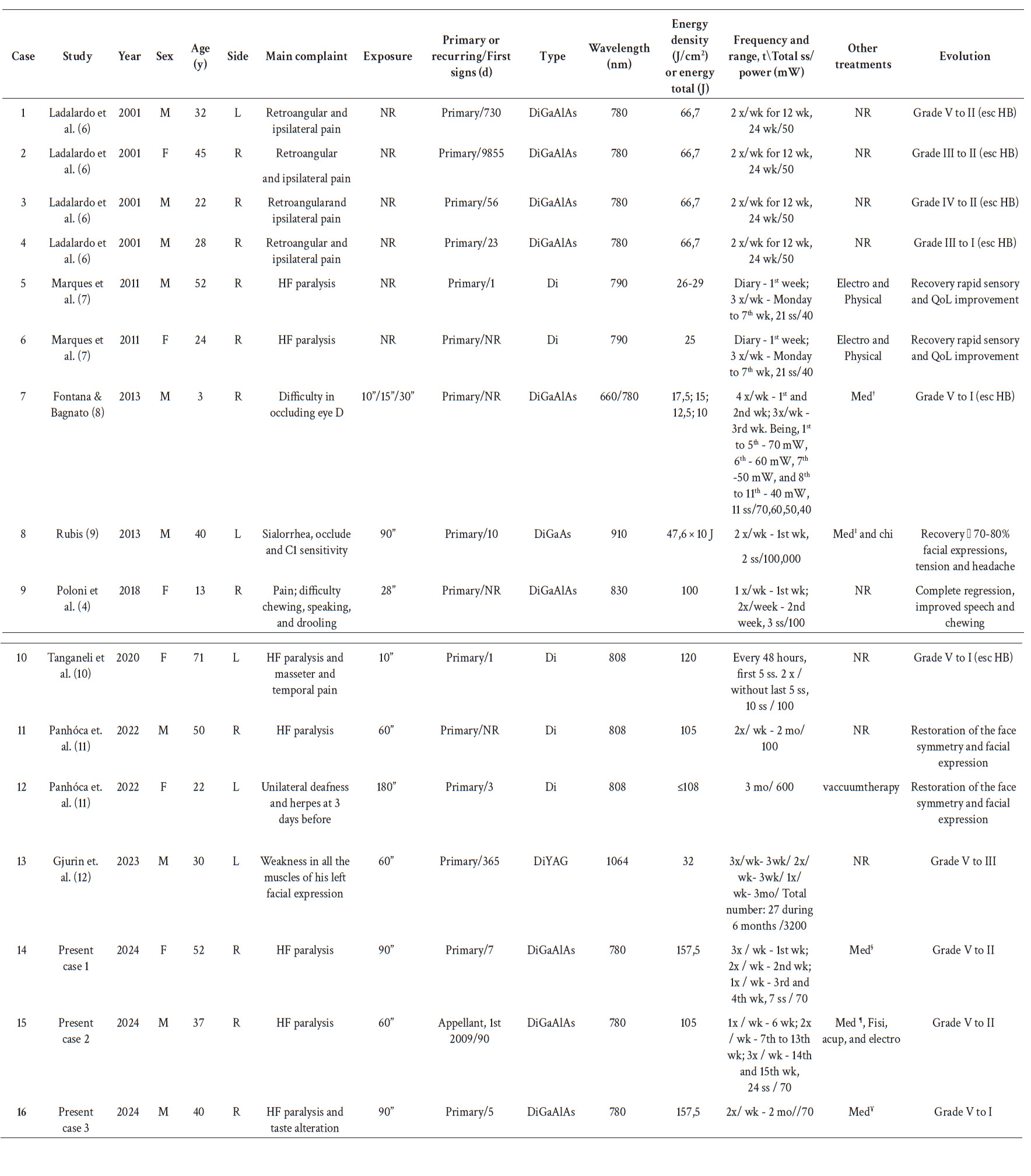
After conducting the case reports, a literature review was undertaken to correlate published clinical cases of individuals with BP treated with LLLT with those treated by our group. The review encompassed studies without restrictions on year and language and was conducted across multiple databases, including PubMed/Medline, Embase (via Elsevier), Virtual Health Library (BVS, by its Spanish acronym), Scopus, and Web of Science. Each database was searched using a specific strategy outlined in the table 1.
The inclusion criteria for selecting studies comprised case reports and case series of individuals with BP treated with LLLT, either alone or in combination with other treatments. Studies were included if they diagnosed patients with BP and reported outcomes in terms of facial nerve functional recovery. Exclusion criteria consisted of studies without full-text access and those lacking clear outcome measures related to facial nerve function. Using the EndNote Web® tool (Clarivate, London, UK), duplicate studies were removed, resulting in the selection of 44 studies for full reading. Of these, 8 articles met the inclusion criteria (4, 612) (figure 4).
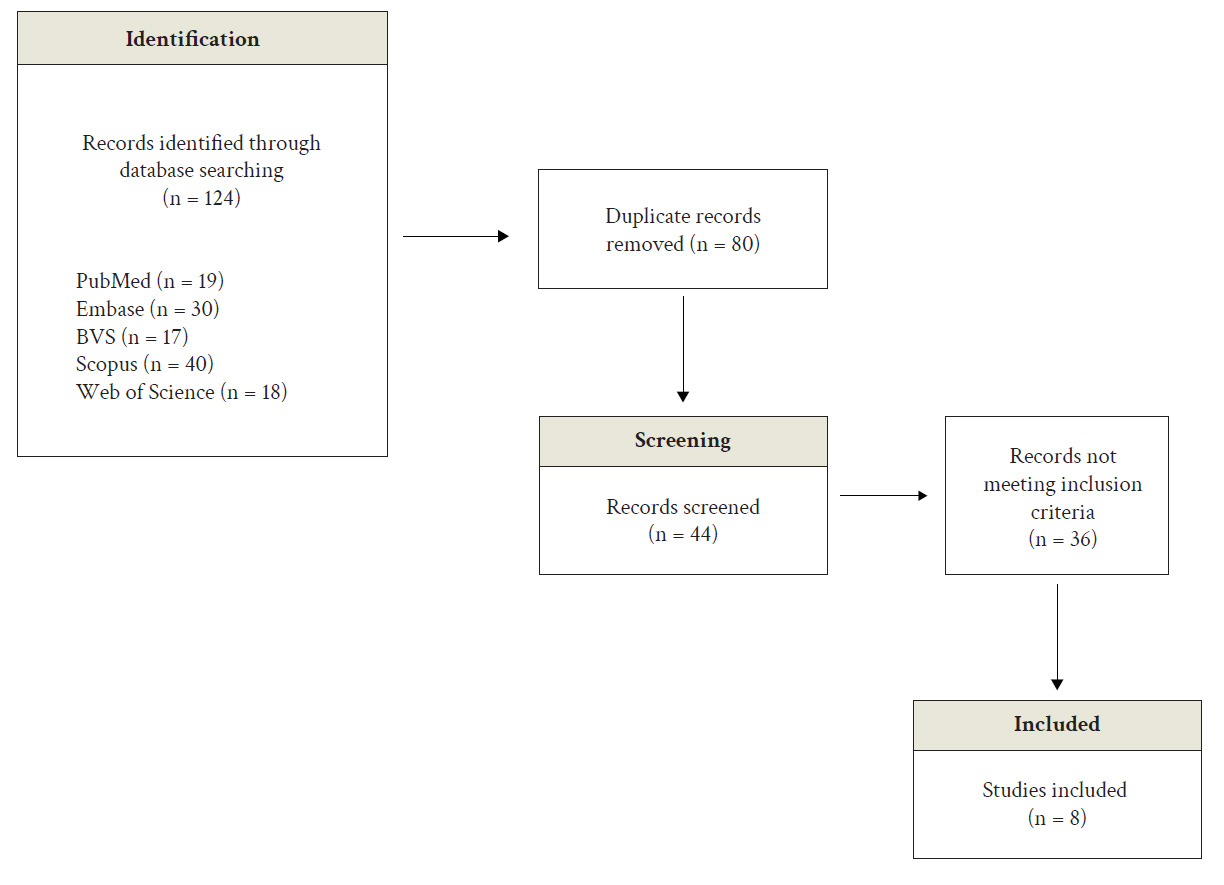
Figure 4 Selection of published case reports of Bell's Palsy treated with low-level light therapy (updated on 04/24/2024).
The data from these studies, along with the current report, are presented in table 2. An update to the search was conducted on April 24, 2024.
DISCUSSION
LLLT is a non-invasive, non-thermal phototherapy method that employs laser light to treat specific body tissues, preventing cell death, reducing inflammation, and promoting cellular regeneration. Operating at the cellular level, LLLT induces significant biochemical changes, activates angiogenesis, stimulates tissue proliferation, and accelerates wound healing 5 Additionally, LLLT provides analgesic benefits triggered by the release of endorphins, and it exhibits a potent anti-inflammatory effect through the reduction of cytokines such as interleukin-1 and tumor necrosis factor, thereby aiding neural repair 13 Furthermore, as a painless, well-tolerated procedure without associated side effects, LLLT is considered an effective therapeutic option, particularly in the treatment of conditions like BP 3
Studies have shown positive results using LLLT as a treatment for BP, either exclusively or combined with other forms of treatment, such as chiropractic care, electrotherapy, physiotherapy, and drug treatment with corticosteroids, antivirals, vitamin B, and other medications (4, 14, 15). This was observed in the three cases treated by our group, where there was a significant recovery of facial expressions with LLLT in addition to acyclovir, prednisone, Nevrix®, vitamin B12, Etna®, physiotherapy, acupuncture, and electrical stimulation therapy.
When reviewing the literature in search of cases of BP treated with LLLT with or without other therapies, 13 were found and added to the three treated by our group, totaling 16 cases (Table 2). It was observed that BP affected individuals aged between 3 and 71 years, as corroborated by other studies (1, 14). However, other studies have shown a higher incidence of BP among adults between 40 and 50 years of age. In this study, most of the patients were under 40 years of age, aligning with the findings of Magazi et al. 16 which noted a higher incidence of BP in individuals under 30 years of age.
Some studies have reported a higher prevalence of BP in men, while others found no distinction between sexes (1, 17). In our review, most of the cases (10 out of 16) were male. Regarding the signs, hemifacial palsy on the right side was the most common, corresponding with what has been reported in other studies. The main complaints, paralysis and/or pain, manifested in most cases. The incapacity of eyelid occlusion was present in six individuals, including the cases treated by our group. Symptoms also included difficulty in chewing and drooling, which are complaints commonly found in individuals with BP 2
The etiology of BP is primarily idiopathic but may include factors such as acute exposure to cold weather, herpetic viral infection, nerve ischemia, and inflammation 18 In some clinical cases identified by our group, a possible viral etiology was noted, along with a relationship with heat shock and an association with stress.
The diagnosis of BP is primarily made through a comprehensive clinical evaluation, which may include the use of supplementary imaging to rule out other causes of facial paralysis, as assessed by the HB scale. In all the cases reviewed, the diagnosis was obtained by clinical examination, but only ten were rated by the HB score. Of these, seven exhibited severe dysfunction (Grade V) (70%), two displayed moderate dysfunction (Grade III) (20%), and one showed moderately severe dysfunction (Grade IV) (10%). This contrasts with findings from another study, where the distribution was 27% at Grade IV, 18% at Grade III, and 17% at Grade V 1
A study indicates that corticosteroid injections in acute idiopathic inflammatory facial paralysis achieve only partial motor recovery after six months, demonstrating minimal to moderate clinical effectiveness 19 In addition, prolonged corticosteroid use in these patients can cause systemic adverse effects, such as hyperglycemia and changes in adrenal gland function, among other effects that may limit their use in patients with decompensated diabetes, for example 19
The literature review observed a reduction in the duration of BP treatment when using LLLT as an adjuvant to medication, as the primary BP cases required fewer sessions (between two and seven sessions) compared to most cases treated with LLLT alone. Additionally, even in the case of recurrent BP where medications were combined with LLLT, the same number of sessions (24 sessions) was necessary, similar to cases treated solely with LLLT (Table 2).
At the end of treatment, five individuals still had mild dysfunction, including two from the cases treated by our group. Among the other cases in this review, seven had complete regression of paralysis, while the remaining cases achieved rapid sensory recovery and notable improvements in facial function and aesthetics. This reinforces that LLLT, as an adjunct to other therapies for BP, leads to significant recovery of facial expressions in a short period of time (15, 19).
Although there is no specific protocol for LLLT in BP, the use of diode lasers, specifically Gallium-Aluminum-Arsenide (GaAlAs) and Gallium-Arsenide (GaAs) diodes, has proven effective. These lasers operate within a wavelength range of 660 to 910 nm, with a power ranging from 40 to 100 mW, and an energy density of 10 to 157.5 J/cm2. Treatments, varying from 2 to 24 sessions, were effective in treating BP in all the cases described in this review (Table 2).
Regaining facial expressions is crucial for improving well-being, achieving satisfactory aesthetics, and enhancing social interactions. Additionally, neural recovery in cases of BP leads to the restoration of vital facial functions such as speaking, swallowing, sucking, and chewing. In our cases, we observed that LLLT effectively restored facial expressions and functions, enhanced aesthetics, and facilitated the individuals' quick return to social interactions.
This study has several inherent limitations typical of case reports, including the small sample size, the absence of a control group, and the variability in individual responses to photobiomodulation treatment. Additionally, the lack of a standardized protocol for LLLT application in patients with BP complicates direct comparisons with other studies. However, this study also has significant strengths. The inclusion of cases with varying degrees of severity and treatment responses provides a comprehensive view of potential clinical variations. Furthermore, the detailed follow-up of patients and rigorous documentation of procedures and outcomes offer a robust foundation for future research.
We decided to complement our case report with a literature review to provide a broader context and validate our findings. The review allowed us to compare our results with those obtained by other researchers, highlighting the consistency and effectiveness of photobiomodulation as an adjuvant therapy for BP. This combined approach strengthens the credibility of our results and contributes to the body of evidence on the use of LLLT in the treatment of BP.
CONCLUSIONS
In conclusion, this case series highlights the promising role of LLLT as a supportive treatment for BP. We observed significant improvements in facial function, aesthetics, and overall wellbeing in our patients, suggesting that LLLT can effectively promote nerve recovery and enhance quality of life. More extensive, randomized controlled trials are needed to establish standardized treatment protocols and further validate our findings. Nonetheless, our results add to the growing evidence that LLLT is a valuable adjunctive therapy for BP and merits further exploration.