Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Gastroenterología del Perú
versión impresa ISSN 1022-5129
Rev. gastroenterol. Perú v.32 n.3 Lima jul./set. 2012
REPORTE DE CASOS
EUS-Guided access to dorsal pancreatic duct in a patient with pancreas divisum
Everson L. A. Artifon, Mariana S. V. Frazão, Flávio Coelho Ferreira, José Pinhata Otoch
Gastrointestinal Endoscopy Unit - University of São Paulo, Sao Paulo, Brazil.
RESUMEN
Se reporta un caso de acceso del conducto pancreatico dorsal por medio de ayuda de ultrasonografía endoscópica en un paciente con cuadro de Páncreas divisum que producía sintomas dolorosos; y que no fué posible su abordaje por PCRE.
PALABRAS CLAVE: Páncreas divisum, Ultrasonografía endoscópica, Tratamiento.
ABSTRACT
Case report of pancreas divisum dorsal pancreatic duct access with endoscopic ultrasonography help to relief pain in a patient with not possible access by PCRE.
KEY WORDS: Pancreas Divisum, Endoscopic Ultrasonography, therapy.
INTRODUCTION
Pancreas divisum is the most common congenital pancreatic anatomical variant, usually asymptomatic, occurring in approximately 7% of the autopsies (range 1% - 14%).1
It is usually asymptomatic, therefore the treatment (endoscopic or surgical) is indicated in symptomatic patients after thorough investigation and ruling out other causes of pancreatic type abdominal pain and acute pancreatitis.2,3
Our objective is to demonstrate a novel technique of EUS-guided access to dorsal pancreatic duct in a patient with pancreas divisum with previous history of acute pancreatitis.
CASE REPORT
We present here a 32 year-old male with many episodes of acute pancreatitis in the last eight years and no history of biliary stones, previous surgery or biliary manipulation. Magnetic resonance cholangiopancreatography demonstrated showed a normal biliary tree and a dilated noncommunication of the dorsal and central ducts with independent drainage sites. As the access through endoscopic retrograde cholangiopancreatography (ERCP) was not possible due to technical difficulty it was used the alternative access through endoscopic ultrasound (EUS).
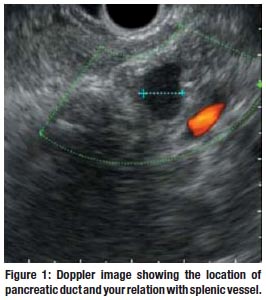
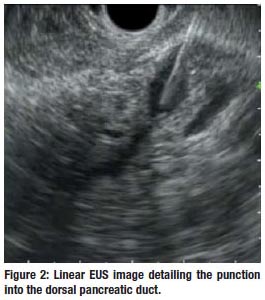
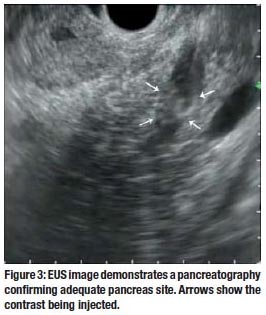
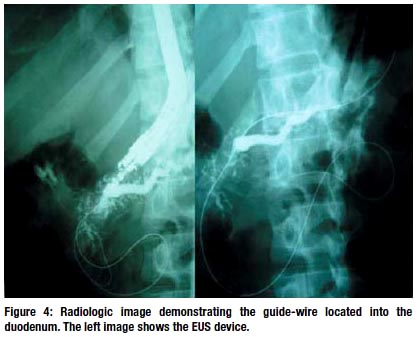
The EUS image showed hiperechoic spots in the pancreatic parenchyma and dilated dorsal pancreatic duct. EUS guided puncture with a 19G needle, while using doppler to avoid vascular damaged, was realized. It is important that the dorsal pancreatic duct is in an obliquous position on the opposite side of the probe. Contrast was injected to confirm adequate puncture site and appears as shifting hiperechoic images by the EUS view. Then a 0,035-inch guidewire was passed through the minor papilla and positioned deeply into the duodenal lumen. A 8,5 Fr plastic stent was located into pancreatic duct to achieve pancreatic drainage, antegradely.
No immediate or late complications were observed in 8 months of follow up. The laboratory exams demonstrated to be normal after the procedure.
DISCUSSION
Pancreas divisum is a congenital anomaly developed by a failure of fusion of the ventral and dorsal buds during the embryonic period. Therefore, the drainage of these glands are made separately in the duodenum.2
Patients with mild symptoms can be managed con servatively. However, those with recurrent acute pancreatictis, chronic pancreatitis or pancreatic-type abdominal pain may require treatment that focuses on decompression and drainage of the dorsal duct, performed endoscopically or surgically.3
Both therapies are effective in reducing episodes of acute pancreatitis and pain relief in approximately 80% of patients. Lower rates of response occur in cases of chronic pancreatitis and pancreatic pain (70% and 55% respectively).3
RCP is the standard procedure for the decompression of the pancreatic duct but may fail in about 10% of the cases due to previous surgery that changes the gastrointestinal tract, malignant gastroduodenal obstruction, intra or peridiverticular papilla, pancreas divisum, among others.4 However, the identification and puncture of the pancreatic duct can be achieved by endoscopic ultrasound and may allow access and passage of guidewire and therapy of pancreatic duct and duodenal papilla.5-7
Wiersema et al initially described EUS-guided access to the pancreatic duct. Access to the pancreas was performed in a patient submitted to gastrectomy with Billroth II reconstruction. Transgastric puncture was achived resulting in a pancreatography that diagnosed pancreas divisum.8
he present case demonstrates the feasibility of a new technique in which we can reach the dilated dorsal pancreatic duct by EUS guidance in a case with previous failed minor papilla retrograde cannulation. The option should be presented and discussed with the family and surgeons before beginning the procedure.
REFERENCES
1. SMANIO T. Proposed nomenclature and classification of the human pancreatic ducts and duodenal papillae: study based on 200 post mortems. Int Surg. 1969; 52:125-134.
2. QUEST L, LOMBARD M. Pancreas divisum: opinio divisa. Gut 2000; 47: 317–319.
3. ALEMPIJEVIC T, STIMEC B, KOVACEVIC N. Anatomical features of the minor duodenal papilla in pancreas divisum. Surg Radiol Anat 2006; 28: 620–624.
4. LEHMAN GA, SHERMAN S. Diagnosis and therapy of pancreas divisum. Gastrointest Endosc Clin N Am. 1998;8:55-77.
5. SUGA T, NAGAKAWA T, MIYAKAWA H, et al. Clinical features of patients with pancreas divisum. Dig Endosc. 1994;6:80-86.
6. SAOWAROS V. Pancreas divisum: incidence and clinical evaluation in Thai patients. J Med Assoc Thai. 1992;75:692-696.
7. MOREIRA VF, MERONO E, LEDO L, et al. Incomplete pancreas divisum. Gastrointest Endosc. 1991;37:104-107.
8. JACOB L, GEENEN JE, CATALANO MF et al. Clinical presentation and shortterm outcome of endoscopic therapy of patients with symptomatic incomplete pancreas divisum. Gastrointest Endosc 1999; 49: 53–57.













