Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Gastroenterología del Perú
versión impresa ISSN 1022-5129
Rev. gastroenterol. Perú vol.35 no.3 Lima jul. 2015
Artículos Originales
Biliary transpapillary endoscopic balloon dilation for treating choledocholithiasis
Dilatación endoscópica biliar transpapilar con balón para el tratamiento de la colédoco litiasis
Lubia B. Daniel1a, Gabriel M. Favaro1a, Tiago F.V. Filho1a, Marco A. B. Cunha2b, Dayse S. P. Aparício2b, Ricardo S. Uemura2b, Carlos K. Furuya Jr 2b, Everson L. A. Artifon2c
1 Hospital Ana Costa. Santos, Sao Paulo, Brasil.
2 Digestive Endoscopy Service, Hospital Ana Costa. Santos, Sao Paulo, Brazil.
a Endoscopy trainee; b Attending physician; c Head
ABSTRACT
Objective: To evaluate the efficacy and safety of transpapillary papilloplasty in patients with choledocholithiasis. Materials and methods: All endoscopic retrograde cholangiopancreatography (ERCP) procedures performed at Hospital Ana Costa, in the city of Santos, Brazil, over the last five years were retrospectively evaluated using the hospital’s information database. The success of the procedure and complications due to residual calculi, pancreatitis, bleeding and perforation were evaluated. Results: From January 2010 to May 2014, 1860 ERCP procedures were performed. Fifty-five patients were evaluated here. Their ages ranged from 12 to 98 years (mean, 66.3; standard deviation, 19.34; median, 71). Thirty-two patients (58.2%) were women. Sixteen (29.1%) presented giant choledocholithiasis, with calculi larger than 12 mm. Twenty-seven (49.1%) had multiple choledocholithiasis. Conclusion: In view of the therapeutic efficacy and low complication rate among our patients, we can conclude that endoscopic papilloplasty is a safe and effective method for endoscopic treatment of choledocolithiasis in selected cases.
Key words: Calculi; Choledocholithiasis; Sphincterotomy, endoscopic (source: MeSH NLM).
RESUMEN
Objetivo: Evaluar la eficacia y seguridad de la papiloplastía trnaspapilar en la colédoco litiasis. Material y métodos: Todas las colangoipancreatografías retrogradas endoscópicas (CPRE) realizadas en el Hospital Ana Costa en la ciudad de Santos Brasil, en los últimos cinco años fueron evaluadas retrospectivamente usando la base de datos del hospital. El éxito y las complicaciones del procedimiento debido a cálculos residuales, pancreatitis, sangrados y perforación fueron estudiados. Resultados: De enero del 2010 a mayo del 2014, se realizaron 1860 CPREs. Se estudiaron 55 pacientes, cuyas edades fluctuaron entre 12 a 98 años con una media de 66,3 y desviación estándar de 19,34. Treinta dos pacientes fueron mujeres (58,2%). 16 (29,1%) tuvieron litiasis coledociana gigante con cálculos mayores de 12 mm y veintisiete (49,1%) tuvieron litiasis múltiple. Conclusión: En vista de la eficacia y la poca frecuencia de complicaciones entre nuestros pacientes podemos concluir que la papilotomía endoscópica es un método seguro y efectivo para el tratamiento de la coledocolitiasis en casos seleccionados.
Palabras clave: Cálculos; Coledocolitiasis; Esfinterotomía endoscópica (fuente: DeCS BIREME).
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) has become one of the most important techniques for treating gallstones. Endoscopic balloon dilatation of the duodenal papilla was developed as a complementary method for treating choledocolithiasis in order to diminish the risk of acute complications caused by minor trauma of the biliary sphincter.
TBalloon sphincteroplasty was originally conceived for extracting calculi, while common bile duct (CBD) minimized the damage to the sphincter of Oddi. However, the disadvantage of balloon sphincteroplasty in relation to sphincterotomy is the more limited size of the papillary opening. Approximately 10% of calculi are difficult to remove using the conventional technique and, for these patients, mechanical lithotripsy is generally the next step (1-3). However, mechanical lithotripsy is slow and has the potential to cause damage to the site of the sphincterotomy or to the bile duct. Moreover, complications may be caused through the impact of the basket in picking up the calculus.
Furthermore, the fragments of the calculus that remain after mechanical lithotripsy may act as a niche for recurrence of the calculus. Mechanical lithotripsy is thus one of the risk factors for recurrent gallstones after endoscopic extraction of the calculus (4). The main aim of balloon dilatation is to avoid having to use mechanical lithotripsy to remove giant calculi from the common bile duct (CBD), so as to reduce the complications that might be related to mechanical lithotripsy.
Ersoz et al. (5) were the first to report using sphincterotomy followed by balloon sphincteroplasty with a large-diameter balloon (12-20 mm) as an alternative technique for dealing with gallstones that are difficult to remove by means of conventional methods. Complete recovery of the calculus without mechanical lithotripsy was achieved in 54 (93.1%) of these authors’ 58 patients, while the calculus was cleared out by means of mechanical lithotripsy in four (6.9%) of the patients. Complications occurred in nine patients (15.5%), including two (3.4%) with mild pancreatitis.
Several studies have now been conducted using sphincterotomy plus balloon dilatation for giant calculi that were considered to be difficult to deal with (6-11).
The complication rates have ranged from 0% to 8.3%, with pancreatitis in 0% to 4.5% of the cases. In most of the previous studies using sphincterotomy plus balloon dilatation to remove giant calculi from the common bile duct (CBD) (6-11), the authors suggested that this technique might be associated with lower risk of pancreatitis. They argued that sphincterotomy prior to balloon dilatation might result in separation between the pancreas and the orifices of the bile ducts, thereby possibly guiding the direction of the balloon towards the bile duct rather than towards the pancreas, during the balloon dilatation.
The aim of our study was to evaluate the efficacy and safety of transpapillary papilloplasty in patients with choledocolithiasis.
MATERIALS AND METHODS
A retrospective study was conducted on all ERCP procedures that were conducted at Hospital Ana Costa, in Santos, Brazil, over the last five years. This was done by means of gathering information from the institution’s database. Between January 2010 and May 2014, 1860 ERCP procedures were performed and a diagnosis of choledocolithiasis was made in the great majority of these cases.
Over this period, 57 papilloplasty procedures were performed. Of these, two were excluded because an alternative biliary access had been used, with external biliary drainage via a transparietal-hepatic route.
The inclusion criteria used for performing papilloplasty was as follows: 1) giant calculi; 2) multiple calculi; 3) peridiverticular papilla; 4) coagulation disorders; and 5) pediatric patients.
The imperative condition for performing papilloplasty was that there needed to be homogenous dilatation of the bile duct, i.e. without craniocaudal disproportion. All the examinations were performed by a single endoscopist (ELAA). A Pentax EPK-1000 video duodenoscope was used. All the patients were subjected to sedation, under supervision by an anesthesiologist.
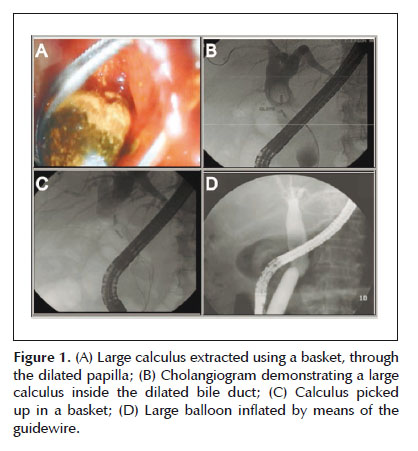
Cannulation of the bile duct was performed using a sphincterotome and a guidewire (Jagwire 0.035F). After cannulation, cholangiography was performed to make the diagnosis, followed by tactical papillotomy i.e. papillotomy of one third of the maximum (broad) papillotomy, with the intention of separating the bile duct from the pancreatic duct and directing the positioning of the balloon in the bile duct. The diameter of the balloon was chosen in accordance with the caliber of the distal bile duct (12 to 18 mm). Hydrostatic dilatation was then performed until the "belt" had disappeared, with a pressure of 3 to 7 atm. The bile ducts were swept to remove the calculi, sometimes preceded by mechanical lithotripsy, which was done in six patients. In the patients whose bile ducts were not completely cleared, it was decided that a plastic biliary prosthesis should be introduced (seven cases). In four patients with hemorrhage following papilloplasty, it was decided that a self-expanding metal prosthesis should be introduced, which successfully controlled the bleeding.
Statistical analysis
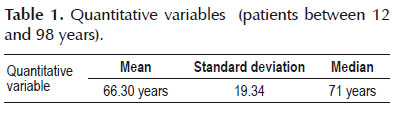
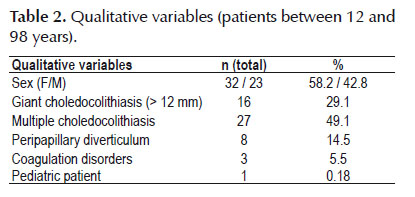
Firstly, all of the variables were analyzed descriptively. For the quantitative variables, this analysis was done by means of observation of the minimum and maximum values and calculation of the means, standard deviations and medians. For the qualitative variables, the absolute and relative frequencies were calculated.
To compare the means of the two groups, Student’s t test was used. To test the homogeneity between the proportions, the chi-square or Fisher exact test was used (Fisher test when the expected frequency was less than 5). The significance level used for the tests was 5%.
RESULTS
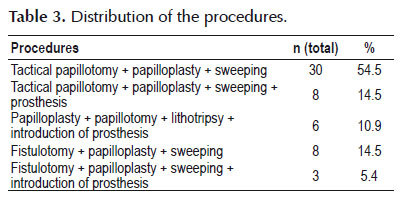
Fifty-five patients who were operated between January 2010 and May 2014 were evaluated. Their ages ranged from 12 to 98 years (mean of 66.30 years, with standard deviation of 19.34 years and median of 71 years). Thirty-two patients (58.2%) were female. Sixteen (29.1%) presented giant choledocolithiasis, with calculi of sizes greater than 12 mm (Figure 1). Twenty-seven (49.1%) had multiple choledocolithiasis. The majority (n=30; 54.5%) underwent papillotomy with papilloplasty and biliary sweeping. Other portions of these patients underwent the following: papillotomy + papilloplasty + sweeping + prosthesis (n=8; 14.5%); papilloplasty + papillotomy + lithotripsy + introduction of prosthesis (n=6; 10.9%); fistulotomy + papilloplasty + sweeping (n=8; 14.5%); and fistulotomy + papilloplasty + sweeping + introduction of prosthesis (n=3; 5.4%).
The patients whose calculi were not completely removed underwent new endoscopic procedures 30 days later. On this occasion, the prosthesis and the residual calculi were removed.
Among the patients for whom a metal prosthesis was used as a means for achieving hemostasis, this prosthesis was removed two weeks later, without intercurrences, including in the patient who developed retroduodenal perforation.
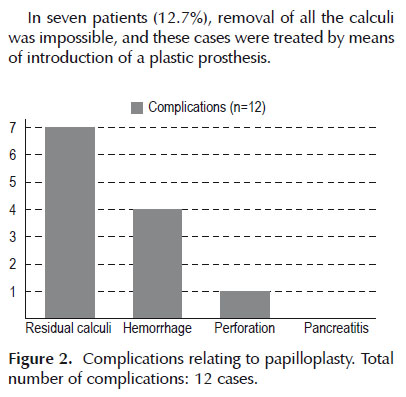
Complications occurred in 21.8% of the cases (n=12), (Figure 2) and these consisted of four cases of episodes of hemorrhage subsequent to papilloplasty (7.2%), one case of perforation (1.8%) and seven cases of residual calculi (12.7%). The cases of hemorrhage were treated by means of introduction of a metal prosthesis, and in one case this was done in association with injection of adrenaline. There was one case of retropneumoperitoneal perforation, which was treated clinically through successfully using a partially covered self-expanding metal prosthesis, antibiotic therapy and fasting. There were no cases of pancreatitis.
In seven patients (12.7%), removal of all the calculi was impossible, and these cases were treated by means of introduction of a plastic prosthesis.
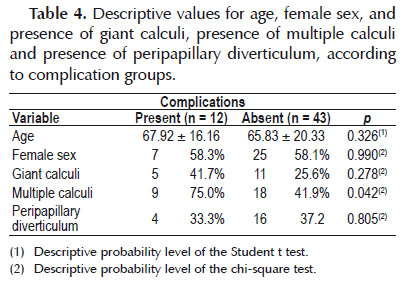
Table 4 presents a comparison between the groups according to the presence or absence of complications (hemorrhage and residual calculi). It can be seen that the groups did not present any significant differences in relation to age, gender, presence of giant calculi or presence of peripapillary diverticulum. However, the group with multiple calculi presented a significantly greater percentage of complications, in comparison with the other groups.
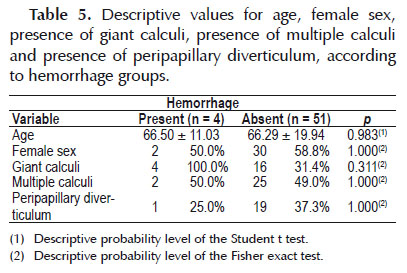
In relation to the complication of hemorrhage, there were no statistically significant differences in relation to the variables studied, as shown in Table 5.
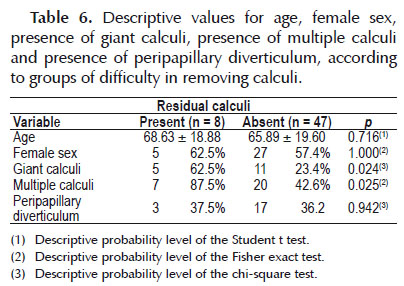
In relation to the difficulty in clearing residual calculi from the bile duct, it was observed that the groups did not present any significant differences in relation to age, sex or presence of peripapillary diverticulum. However, in the groups of patients with giant calculi and multiple calculi, there were statistically significant differences, as shown in Tabla 6.
DISCUSSION
Endoscopic sphincterotomy is the therapy typically used for the extraction of stones in the CBD, but this technique has many early complications, including bleeding, pancreatitis, and perforation (12,13). The sphincterotomy causes permanent loss of function of sphincter of Oddi, allowing exposure of the biliary tree for bacterial colonization and chronic inflammation. The ballooned dilatation offers the advantage of avoiding bleeding and perforation, once this procedure does not make cuts in the duodenal papilla, also avoiding permanent damage to the biliary sphincter.
The most common and most feared complication after performing the ERCP is acute pancreatitis. The incidence of acute pancreatitis after ERCP varies according to literature, from 1% to 13.5% and some authors report the occurrence of severe forms, with a mortality of up to 27% of these cases (14,15). In this study, acute pancreatitis was not observed.
Currently, balloon dilation is considered an alternative to endoscopic sphincterotomy in some high-risk patients, especially those at higher risk for bleeding or perforation. Although the dilation with balloon singly is associated with a high risk of pancreatitis, than the papillotomy singly, the dilatation with a balloon of large diameter after tactical papillotomy, doesn’t appear to be associated with a high rate of pancreatitis.
The dilatation with a balloon of large diameter after tactic papillotomy, appears to be a safe and effective technique in the context of calculus in the bile duct that are difficult to extract with the use of conventional techniques and papillotomy.
It should be estimated size of the bile duct, the size and the amount of calculus, the shape and size of the papilla and the papilla’s presence in intra or peridiverticular position.
Once that, the use of a larger balloon may tear the sphincter and also the bile duct, possibly resulting in bleeding and perforation, it is recommended a balloon similar or smaller, in diameter, than the diameter of the distal bile duct. The maximum transverse diameter of calculus and the proportion between the balloon and the calculus tend to affect the success or failure of the complete removal of the calculus through the dilation with balloon of large diameter.
The comorbidities of the patient and the presence of coagulopathy or the need for anticoagulation seem to favor the use of the dilatation and not of papilotomy.
Conclusion
In view of the therapeutic efficacy and low complication rate among our patients, we can conclude that endoscopic papilloplasty is a safe and effective method for endoscopic treatment of choledocolithiasis in selected cases.
Conflicts of interest: none.
Funding sources: none.
REFERENCES
1. Binmoeller KF, Bruckner M, Thonke F, Soehendra N. Treatment of difficult bile duct stones using mechanical, electrohydraulic and extracorporeal shock wave lithotripsy. Endoscopy. 1993;25(3):201-6. [ Links ]
2. Cipolletta L, Costamagna G, Bianco MA, Rotondano G, Piscopo R, Mutignani M, et al. Endoscopic mechanical lithotripsy of difficult common bile duct stones. Br J Surg. 1997;84(10):1407-9. [ Links ]
3. Binmoeller KF, Schafer TW. Endoscopic management of bile duct stones. J Clin Gastroenterol. 2001;32(2):106-18. [ Links ]
4. Ando T, Tsuyuguchi T, Okugawa T, Saito M, Ishihara T, Yamaguchi T, et al. Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut. 2003;52(1):116-21. [ Links ]
5. Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57(2):156-9. [ Links ]
6. Heo JH, Kang DH, Jung HJ, Kwon DS, An JK, Kim BS, et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66(4):720-6. [ Links ]
7. Maydeo A, Bhandari S. Balloon sphincteroplasty for removing difficult bile duct stones. Endoscopy. 2007;39(11):958-61. [ Links ]
8. Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy . World J Gastroenterol. 2007;13(15):2179-82. [ Links ]
9. Attasaranya S, Cheon YK, Vittal H, Howell DA, Wakelin DE, Cunningham JT, et al. Large-diameter biliary orifice balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest Endosc. 2008;67(7):1046-52. [ Links ]
10. Bang S, Kim MH, Park JY, Park SW, Song SY, Chung JB. Endoscopic papillary balloon dilation with large balloon after limited sphincterotomy for retrieval of choledocholithiasis. Yonsei Med J. 2006;47(6):805-10. [ Links ]
11. Kim TH, Oh HJ, Lee JY, Sohn YW. Can a small endoscopic sphincterotomy plus a large-balloon dilation reduce the use of mechanical lithotripsy in patients with large bile duct stones? Surg Endosc. 2011;25(10):3330-7. [ Links ]
12. Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335(13):909-18. [ Links ]
13. Ikeda S, Tanaka M, Matsumoto S, Yoshimoto H, Itoh H. Endoscopic sphincterotomy: long-term results in 408 patients with complete follow-up. Endoscopy. 1988;20(1):13-7. [ Links ]
14. Pitchumoni CS, Patel NM, Shah P. Factors influencing mortality in acute pancreatitis: can we alter them? J Clin Gastroenterol. 2005;39(9):798-814. [ Links ]
15. Fung AS, Tsiotos GG, Sarr MG. ERCP- induced acutenecrotizing pancreatitis: is it a more severe disease? Pancreas. 1997;15(3):217-21. [ Links ]
Correspondence: Lubia B. Daniel
Rua Pedro Américo 60, 11075-400. Santos, SP, Brazil.
E-mail: lubiabonini@hotmail.com
Recibido: 08-02-2015
Aprobado: 30-04-2015