Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de Gastroenterología del Perú
Print version ISSN 1022-5129
Rev. gastroenterol. Perú vol.35 no.3 Lima July 2015
Reportes de Caso
Acute respiratory distress syndrome due to Clostridium difficile colitis: a case report and review of the literature
Síndrome de distress respiratorio agudo debido a colitis por Clostridium difficile: reporte de caso y revisión de la literatura
Jean A. Donet1a, Joseph J. Laconti1a, Jose A. Morillas2, Jodie A. Barkin3a, Jamie S. Barkin3ab
1 Department of Medicine, Leonard M. Miller School of Medicine, University of Miami. Miami, Florida, USA.
2 Department of Medicine, School of Medicine, Universidad Nacional de Trujillo. Trujillo, Perú.
3 Division of Gastroenterology, Department of Medicine, Leonard M. Miller School of Medicine, University of Miami. Miami, Florida, USA.
a MD; b MACG
ABSTRACT
Clostridium difficile is a major cause of antibiotic-associated diarrhea. We report a patient with complicated Clostridium difficile infection (CDI) who developed rapidly progressive acute respiratory distress syndrome (ARDS), for which CDI was the only identifiable source. CDI should be considered in the differential diagnosis for anyone with diarrhea who presents ARDS, especially in high-risk groups such as the elderly, hospitalized patients, or those who have had a history of CDI.
Key words: Clostridium difficile; Colitis; Respiratory distress syndrome, acute (fuente: DeCS BIREME).
RESUMEN
El Clostridium difficile es una de las causas más frecuentes de diarreas asociadas a antibióticos. Reportamos un paciente con infección por Clostridium difficile complicada (CDI) que desarrolló rápida y progresivamente un síndrome de distress respiratorio agudo (ARDS), del cual el CDI fue la fuente única identificable. El CDI debe considerarse en el diagnóstico diferencial de cualquier persona con diarrea que presenta ARDS, especialmente en los grupos de alto riesgo como los ancianos, pacientes hospitalizados o aquellos que han tenido historia precia de DCI.
Palabras clave: Infecciones por Clostridium; Síndrome de dificultad respiratoria aguda (source: MeSH NLM).
INTRODUCTION
Clostridium difficile is a major cause of antibiotic-associated diarrhea. It is the leading cause of hospital admissions and death from gastroenteritis; however, only rarely has Clostridium difficile been reported to cause severe extra-intestinal complications (1). is the most common cause of antibiotic-associated diarrhea (2). Rates of CDI have been increasing since 2000, and these are becoming more severe, refractory to standard therapy, and more likely to relapse than previously observed (2). A factor is development of new, more virulent strains and a widespread use of broad-spectrum antibiotics (3). CDI can cause a wide range of disease, from asymptomatic carrier states, to mild diarrhea, to pseudomembranous colitis, and to fulminant systemic disease. The occurrence of severe systemic complications such as sepsis, multiple organ dysfunction syndrome (MODS), and acute respiratory distress syndrome (ARDS) caused by CDI is rare, and only has been reported in few cases associated with high mortality (4). The aim of this case report is to present a patient with a history of recurrent CDI that developed ARDS with CDI as the only identifiable cause, while his CDI was clinically improving.
CASE REPORT
A 60 year-old Hispanic man, with history of recurrent CDI, hypertension and hepatitis C, presented to the emergency department, complaining of three days of diffuse abdominal pain, progressive diarrhea and non-bilious vomiting. He had three prior episodes of CDI-related colitis during the prior 12 months treated with medication regimens including oral and intravenous (IV) metronidazole, oral vancomycin and probiotics.
Physical exam revealed fever (38.4°C), mild abdominal distension with diffuse tenderness, and hyperactive bowel sounds, but no rebound tenderness or guarding. Initial laboratory values that were abnormal included leukocytosis with a left shift (WBC 19,000, neutrophils 90%), a lactate of 2.3 mmol/l, and mild acute kidney injury (Creatinine 1.3g/dl, BUN:Cr Ratio 20g/dl). Stool studies were positive for CDI via loop mediated isothermal amplification assay for C. difficile toxin B. The patient was started on vancomycin 125 mg PO every 6 hours and metronidazole 500 mg IV every 8 hours for moderate-severe CDI.
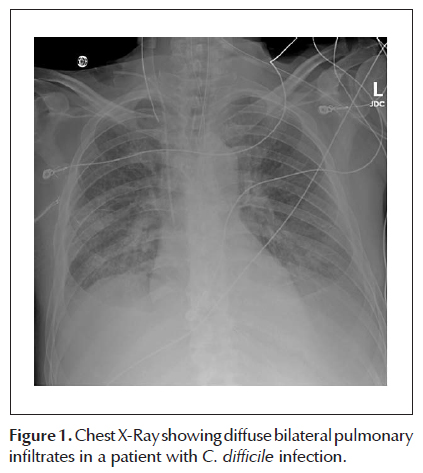
Clinically, his abdominal pain improved, nausea and vomiting abated, and diarrhea decreased. Despite initial clinical improvement, 72 hours after admission, the patient developed acute delirium, fever, profound hypoxemia (O2 Sat 68% on room air; ABG 7.43/23.7/62.2), and required intubation. Chest radiograph (Figure 1) at this time showed diffuse bilateral alveolar infiltrates with pleural effusions, consistent with acute respiratory distress syndrome (ARDS). He was empirically treated with broad-spectrum antibiotics including IV vancomycin and piperacillin/tazobactam. An echocardiogram was unremarkable. CT of the abdomen showed diffuse colitis without colonic dilation, and no free air or ascites. CT of the chest showed small bilateral pleural effusions, with overlying atelectasis, and diffuse airspace opacities throughout the lungs consistent with ARDS (Figure 2). Blood, urine, stool, and broncho-alveolar lavage (BAL) cultures remained negative. BAL studies were consistent with ARDS.
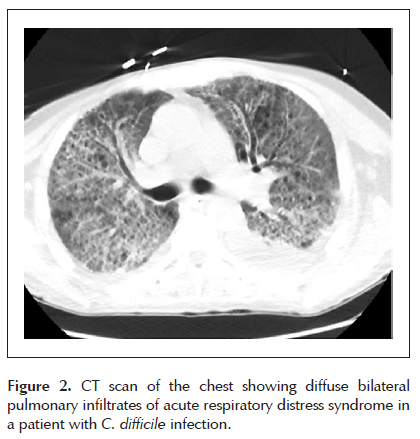
CDI-related colitis was the only identified primary source of the systemic inflammatory response, and antibiotics were subsequently narrowed to oral vancomycin and IV metronidazole for the confirmed CDI. In the following days, the patient’s diarrhea, respiratory status, and bilateral infiltrates seen on CT scan improved, and the patient was extubated and subsequently discharged home.
DISCUSSION
The clinical presentation of CDI is notoriously unpredictable (3). Most patients are asymptomatic carriers, but the severity of C. difficile colitis ranges from mild cases to toxic megacolon with perforation and rarely may result in a variety of severe systemic complications (3,5). Several mechanisms for increased disease severity have been proposed, including the emergence of more virulent strains with higher levels of bacterial toxins A and B (7), and a delay in the diagnosis, especially when the lag time between antibiotic ingestion and diarrhea is unclear (normally variable between 2-10 weeks) (6). Patients can also present with non-classical CDI symptomatology, which may include extra-intestinal and systemic complications such as ascites (7), pleural effusions (7), hepatic abscess (8), and renal failure (9). This sort of presentation may make it difficult for physicians to identify the origin of the complication if CDI is not considered early in the patient’s course.
The occurrence of systemic CDI with severe complications such as sepsis and multiple organ dysfunction syndrome (MODS) is rare (10). In the very few case reports of CDI and MODS, the mortality rates were as high as 24% (11). Host factors appeared to be related to a more severe presentation are advanced age over 65 (12), malnutrition, hypogammaglobulinemia, inflammatory bowel disease (13), bowel ischemia, chronic liver disease (14), organ transplant recipients (solid organ and hematopoietic), on-going malignancy or chemotherapy, and chronic steroid use (14).
There are only two prior reports of CDI causing ARDS in the literature. Our patient, with a history of recurrent CDI, presented with criteria of a moderate-severe complicated episode of colitis (5), received prompt and appropriate treatment with antibiotics, initially clinically improved, and then rapidly developed ARDS. Similarly, Jacob et al. described a patient with C. difficile colitis that progressed after days of antibiotic therapy and clinical improvement to develop hemodynamic deterioration and ARDS requiring intubation and ICU management (5). Conversely, Possamai et al. presented a 66 year-old cirrhotic woman with CDI who progressed to septic shock and ARDS; however as the authors hypothesized, the rapid deterioration of her clinical status was likely due to a delay in the diagnosis of CDI (15).
Eckel (16) suggested a mechanism for severe sepsis in a patient with recurrent CDI to be the disruption of the gastrointestinal barrier secondary to chronic local inflammation by C. difficile toxins. Even though C. difficile is a noninvasive bacterium producing most of its pathogenicity by toxins that cause colonic mucosal injury and inflammation (5), there are reports of extra-intestinal CDI causing bacteremia, osteomyelitis, visceral abscess, empyema, reactive arthritis, pyelonephritis, prosthetic joint infections, and skin and soft tissue infections. Other mechanism proposed, based on animal studies, is the translocation of Toxins TcdA and TcdB, which can reach the circulation and cause a pro-systemic inflammatory response (16). Further, given that mortality from ARDS can be up to 40%, prompt identification and early treatment of CDI may be the most valuable means of improving survival (4).
Conclusion
The occurrence of ARDS in a patient with clinically improving CDI is rare. While a thorough investigation as to the cause of these syndromes is paramount, we must be aware that CDI can result in this complication. In critically ill patients, prompt identification of possible CDI, as the inciting etiology is imperative for early therapeutic interventions to prevent severe systemic reactions and minimize morbidity and mortality.
Disclosures
Author contributions: J. Donet performed the literature review, wrote the initial manuscript, and performed editions. J. Laconti and J. Morillas assisted with writing the initial manuscript, and performed revisions. J.A. Barkin performed revisions and assisted editing the drafts, and provided expert opinion. J.S. Barkin revised the final draft, provided expert opinion, and is the guarantor of this article.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
REFERENCES [ Links ]
2. Rupnik M, Wilcox MH, Gerding DN. Clostridium difficile infection: new developments in epidemiology and pathogenesis. Nat Rev Microbiol. 2009;7(7):526-36. [ Links ]
3. Kelly CP, LaMont JT. Clostridium difficile more difficult than ever. N Engl J Med. 2008;359(18):1932-40. [ Links ]
4. Jacob SS, Sebastian JC, Hiorns D, Jacob S, Mukerjee PK. Clostridium difficile and acute respiratory distress syndrome. Heart Lung. 2004;33(4):265-8. [ Links ]
5. Surawicz CM, Brandt LJ, Binion DG, Ananthakrishnan AN, Curry SR, Gilligan PH, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108(4):478-98. [ Links ]
6. Henrich TJ, Krakower D, Bitton A, Yokoe DS. Clinical risk factors for severe Clostridium difficile-associated disease. Emerg Infect Dis. 2009;15(3):415-22. [ Links ]
7. Tsourous GI, Raftopoulos LG, Kafe EE, Manoleris EK, Makaritsis KP, Pinis SG. A case of pseudomembranous colitis presenting with massive ascites. Eur J Intern Med. 2007;18(4):328-30. [ Links ]
8. Sakurai T, Hajiro K, Takakuwa H, Nishi A, Aihara M, Chiba T. Liver abscess caused by Clostridium difficile. Scand J Infect Dis. 2001;33(1):69-70. [ Links ]
9. Cunney RJ, Magee C, McNamara E, Smyth EG, Walshe J. Clostridium difficile colitis associated with chronic renal failure. Nephrol Dial Transplant. 1998;13(11):2842-6. [ Links ]
10. Dobson G, Hickey C, Trinder J. Clostridium difficile colitis causing toxic megacolon, severe sepsis and multiple organ dysfunction syndrome. Intensive Care Med. 2003;29(6):1030. [ Links ]
11. Aas J, Gessert CE, Bakken JS. Recurrent Clostridium difficile colitis: case series involving 18 patients treated with donor stool administered via a nasogastric tube. Clin Infect Dis. 2003;36(5):580-5. [ Links ]
12. Pépin J, Valiquette L, Cossette B. Mortality attributable to nosocomial Clostridium difficile-associated disease during an epidemic caused by a hypervirulent strain in Quebec. CMAJ. 2005;173(9):1037-42. [ Links ]
13. Ananthakrishnan AN, Issa M, Binion DG. Clostridium difficile and inflammatory bowel disease. Gastroenterol Clin North Am. 2009;38(4):711-28. [ Links ]
14. Vanjak D, Girault G, Branger C, Rufat P, Valla DC, Fantin B. Risk factors for Clostridium difficile infection in a hepatology ward. Infect Control Hosp Epidemiol. 2007;28(2):202-4. [ Links ]
15. Possamai C, Corbanese U, Possamai G, Casagrande L, Farinea C. Multiple organ failure due to Clostridium difficile sepsis. A case report. Minerva Anestesiol. 1997;63(6):205-7. [ Links ]
16. Eckel F, Huber W, Weiss W, Lersch C. Recurrent pseudomembranous colitis as a cause of recurrent severe sepsis. Z Gastroenterol. 2002;40(4):255-8. [ Links ]
Recibido: 21-01-2015;
Aprobado: 12-05-2015













