Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de Gastroenterología del Perú
Print version ISSN 1022-5129
Rev. gastroenterol. Perú vol.36 no.4 Lima Oct./Dec. 2016
ARTÍCULOS ORIGINALES
Guide wire-assisted cannulation versus conventional contrast to prevent pancreatitis. A systematic review and meta-analysis based on randomized control trials
Canulación asistida por alambre guía versus contraste convencional para prevenir la pancreatitis. Una revisión sistemática y meta-análisis basados en ensayos aleatorios controlados
Eduardo T.H. De Moura1, Eduardo G.H. De Moura1, Wanderley Bernardo1, Spencer Cheng1, Andre Kondo1, Diogo T.H. De Moura1, Jose Bravo1, Everson L.A. Artifon1
1 Gastrointestinal Endoscopy Unit, University of São Paulo Medical School. São Paulo, Brazil.
ABSTRACT
Objective: Through this systematic review and meta-analysis, we aim to clarify the differences between these two techniques, thus improving primary success cannulation and reducing complications during endoscopic retrograde cholangiopancreatography, primarily pancreatitis. Methods: A comprehensive search was conducted to search for data available up until June2015from the most important databases available in the health field: EMBASE, MEDLINE (via PubMed), Cochrane, LILACS and CENTRAL (via BVS), SCOPUS, the CAPES database (Brazil), and gray literature. Results: Nine randomized clinical trialsincluding2583 people were selected from20,198 studies for meta-analysis. Choledocholithiasis had been diagnosed in mostly (63.8%) of the patients, who were aged an average of 63.15 years. In those patients treated using the guide wire-assisted cannulation technique, provided a significantly lower instance of pancreatitis (RD=0.03; 95% CI: 0.01-0.05; I2= 45%) and greater primary success cannulation (RD=0.07; 95% CI: 0.03-0.12; I2=12%) than conventional contrast cannulation. Conclusions: The guide wire-assisted technique, when compared to the conventional contrast technique, reduces the risk of pancreatitis and increases primary success cannulation rate. Thus, guide wire-assisted cannulation appears to be the most appropriate first-line cannulation technique.
Keywords: Catheterization; Cholangiopancreatography, endoscopic retrograde; Pancreatitis; Meta-analysis (source: MeSH NLM).
RESUMEN
Objetivo: A través de esta revisión sistemática y meta-análisis, nuestro objetivo es aclarar las diferencias entre estas dos técnicas, mejorando así la canulación de éxito primario y reducir las complicaciones durante la colangiopancreatografía retrógrada endoscópica, principalmente la pancreatitis. Métodos: Una búsqueda exhaustiva se realizó para buscar datos disponibles hasta junio de 2015, desde las bases de datos más importantes disponibles en el campo de la salud: EMBASE, MEDLINE (vía PubMed), Cochrane, LILACS y CENTRAL (a través de la BVS), SCOPUS, la base de datos CAPES (Brasil), y la literatura gris. Resultados: Nueve ensayos clínicos aleatorios incluyendo 2583 personas fueron seleccionados de 20198 estudios de meta- análisis. Coledocolitiasis había sido diagnosticada en su mayoría (63,8%) de los pacientes, que tenían entre un promedio de 63,15 años. En los pacientes tratados con la técnica de canulación guiada, proporcionado una instancia significativamente menor de pancreatitis (RD=0,03; IC del 95%: 0,01-0,05; I2=45%) y una mayor canalización de éxito primario (RD=0,07; IC del 95%: 0,03-0.12; I2=12%) que la canulación por contraste. Conclusiones: La técnica canulación con alambre guía, en comparación a la técnica de contraste convencional, reduce el riesgo de pancreatitis y aumenta la tasa de canulación con éxito primario. Por lo tanto, canulación con alambre guía parece ser la técnica de canulación de primera línea y la más adecuada.
Palabras clave: Cateterismo; Pancreatocolangiografía retrógrada endoscópica; Pancreatitis; Metanálisis (fuente: DeCS BIREME).
INTRODUCTION
Nowadays, endoscopic retrograde cholangiopancreatography (ERCP) is one of the most important endoscopic procedures. However, cannulation techniques are still controversial (1).
Two types of cannulation techniques are routinely used in current practice: guide wire-assisted (GW) cannulation and conventional contrast (CC) cannulation. Several randomized clinical trials (RCT) had demonstrated that guide wire-assisted cannulation increases the primary success cannulation and reduces the risk of pancreatitis compared to conventional contrast cannulation.
However, some recently papers (2-4) published from Japan suggest that the use of guidewire is a significant risk factor for pancreatitis.
Since its first description in 1968, endoscopic retrograde cholangiopancreatography (ERCP) has become an established modality for the diagnosis and treatment of pancreaticobiliary disorders (5). Over the years, it has evolved from a purely diagnostic to a primarily therapeutic procedure and is considered one of the most important endoscopic procedures. Nowadays, around 500,000 ERCPs are performed annually in the USA with adverse event rates between 4% and 10%, and mortality between 0.05% and 1% (6).
Acute pancreatitis is one of the most common serious adverse events of ERCP and has an incidence rate between 5% and 10%, except in high-risk populations, where it is up to 25% (7). Many risks factors for pancreatitis were identified, such as: sphincter of Oddi dysfunction, periampullary diverticulum, recurrent pancreatitis, youth female sex, history of pancreatitis, difficult cannulation, pancreatic sphincterotomy, inadvertently letting the guidewire enter the pancreatic duct, multiple injections of the pancreatic duct, endoscopist’s expertise, and trainee involvement in cannulation (8). To reduce pancreatitis rates, new materials and accessories are being developed daily.
The latest meta-analysis regarding GW and CC cannulation, published in February 2013 of F. Tse et al. (9), demonstrated that GW cannulation was associated with a lower pancreatitis rate and a higher initial cannulation success rate. It included twelve randomized controlled trials (RCT).
However, that meta-analysis had some limitations.
Firstly, they used RCT’s abstract papers mixing then with RCT’s fully text which prevents an appropriate critical evaluation of the studies, for example: randomization and blinding.
Secondly, they mixed non-crossover studies with crossover studies, by mixing different study designs in one meta-analysis reduces the value of the meta- analysis because mixing techniques will cause a loss in statistical power difference in the overall efficacy of the intervention and an inability to distinguish charitable or noxious effects related to the intervention.
In addition, the crossover technique does not preserve the original allocation of patients, preventing a proper comparison between techniques.
Thirdly, the quality of the selected studies is questionable, such as: they used a study which the patient follows up loss was greater than 20%.
Finally, some results shown in his meta-analyses have un acceptable heterogeneities of 85%, which does not support an adequate evidence.
Even though, respecting the last systematic review and meta-analysis of about these theme we performed a new meta-analysis using only RCT’s and non-crossover studies to eventually reach a new conclusion comparing techniques for cannulation of the common bile duct, preventing complications such as pancreatitis.
To compare GW cannulation and CC cannulation of the common bile duct during ERCP for the prevention of pancreatitis and primary success cannulation.
METHODS
Protocol and Registration
This meta-analysis has been registered in PROSPERO (10) international prospective register of systematic review by the number CRD42015015445.
Eligibility criteria
All RCT’s comparing GW and CC cannulation techniques in patients who needed ERCP and who had an intact papilla of Vater. These sources of information and databases were assessed: EMBASE, MEDLINE (via PubMed), Cochrane, LILACS and CENTRAL (via BVS), SCOPUS, CAPES database (Brazil), and gray literature. Any outcome from any date of publication until October 2014, with any number of subjects was considered. Publications were accepted in any format, language, or publication status. The bases were assessed using the Jadad scale (11), and meta-analysis was conducted through the RevMan 5 software (12).
Search strategies
See Appendix 1.
Study selection
Initially, studies were excluded because information in the title or abstract does not allow the comparison between GW and CC cannulation. Furthermore, the abstracts and full articles were assessed and excluded if proven not to be a RCT or if the comparison was not between GW and CC cannulation. Also, some studies were previews of later ones, and were excluded after confirmation.
Data collection process
Data was extracted from all the databases and information sources mentioned by two independent authors, confirming the same eligible final studies. The eligible studies were confronted after both authors completed their searches.
Data items
The pancreatitis outcome was defined as abdominal pain after more than 24 hours post-ERCP and amylase greater than 3x, except in Lella et al. (13), where it was abdominal pain after more than 24 hours. Initial cannulation success was defined as successful cholangiography in selective bile duct cannulation with the cannulation time, pancreatic duct cannulations, and pancreatic duct injections ranging between the studies.
Risk of bias in individual studies
Biases were individually assessed through the Jadad scale (11), a tool used to assess the quality of an RCT through evaluation of blinding, randomization, and losses. We also assessed other biases such as intention to treat analysis (ITT), sample calculation, cross-over, and veiled allocation.
Likewise, we assessed the description of the study (procedure descriptions, techniques used, number of people included, inclusion criteria, exclusion criteria, patient characteristics, comparisons made, patient follow-up, outcomes assessed, size of the effect identified, and whether the study was funded), validity of the study (whether the study followed all the above criteria, whether patient characteristics of different groups were similar, whether the only difference between the groups was the treatment under investigation, whether outcomes were measured in an appropriate and valid way, whether the percentage of loss was lower than 20%, and whether the study was conducted in more than one place, and the overall assessment of the study (if studies were comparable between them and whether it considered if the clinical effect was obtained as a result of intervention).
Summary measure
The difference was calculated in risk differences for dichotomic variables using the Cochrane–Mantel– Haenszel (CMH) test with a 95% confidence interval.
Synthesis of results
RevMan 5 software (12) was used for meta-analysis of initial cannulation success and risk of pancreatitis.
Heterogeneity was evaluated, when possible and necessary, below 50% using a sensitivity analysis. Analyses of all parameters influenced by variability in the data were performed to estimate reliability of results.
The uncertainties derived from sampling errors were analyzed from intervals reliably applied to the result of the study. Sensitivity analyses were used to reduce heterogeneity arising from publication bias, which was used to define the works that result in disparities between effects and sample sizes.
Risk of bias across the studies
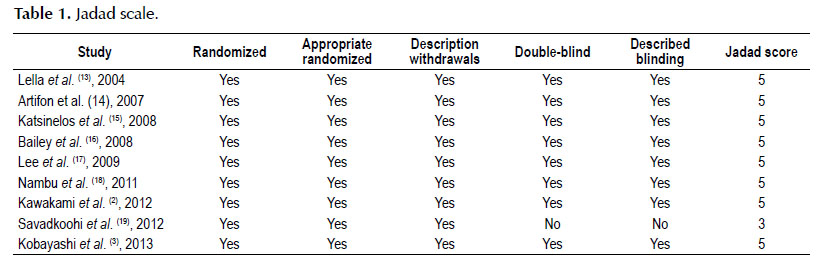
The risk of bias was related using a funnel plot (publication bias), heterogeneity, and analysis of the global biases of individual study as shown in the Jadad score (Table 1).
Additional analyses
Sensitivity analyses were evaluated for pancreatitis rate and initial cannulation success.
RESULTS
Study selection
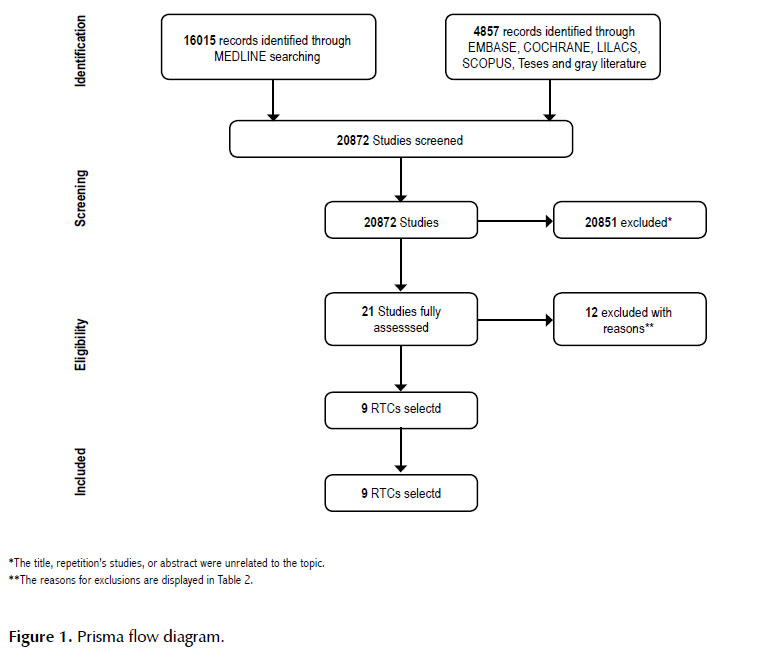
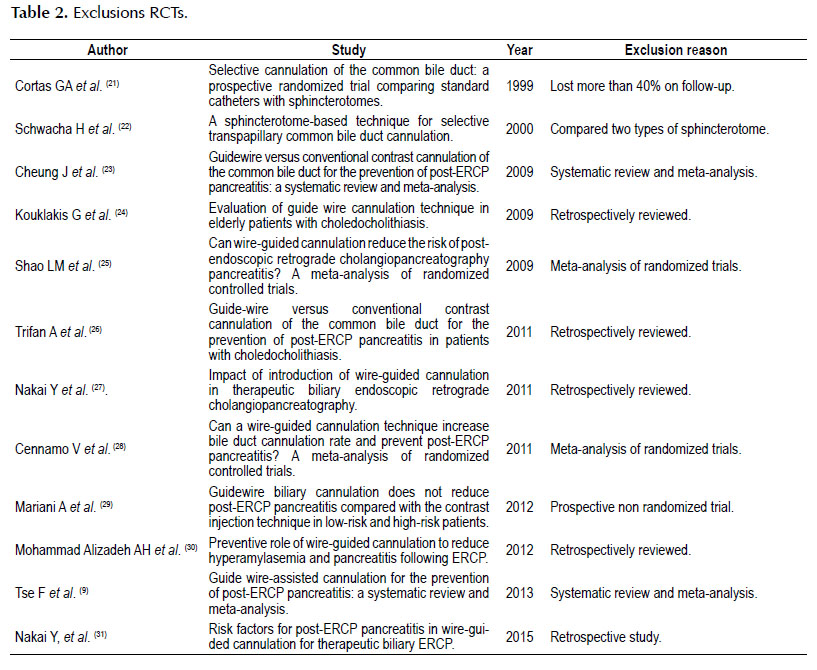
There were 20,872 studies found by the initial search, of which 20,851 were excluded through title, repetition, and/or abstract (Figure 1) (20). Twenty-one studies were fully assessed, of which twelve were excluded (Table 2).
Study characteristics
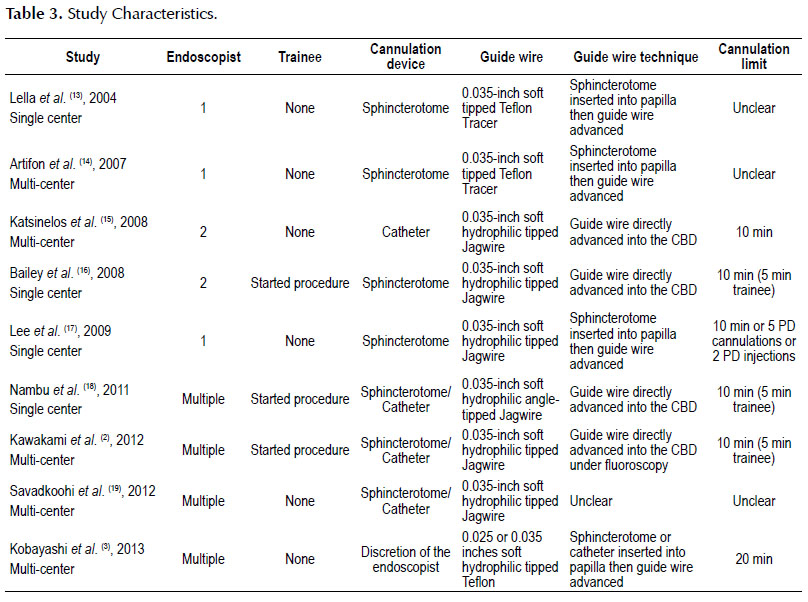
Table 3 shows the characteristics of the included studies. All 9 studies were "non-crossover" RCTs. The number of participants per trial ranged from 143 to 413, totaling of 2,583. All studies included patients with intact papilla who required ERCP for pancreatobiliary diseases.
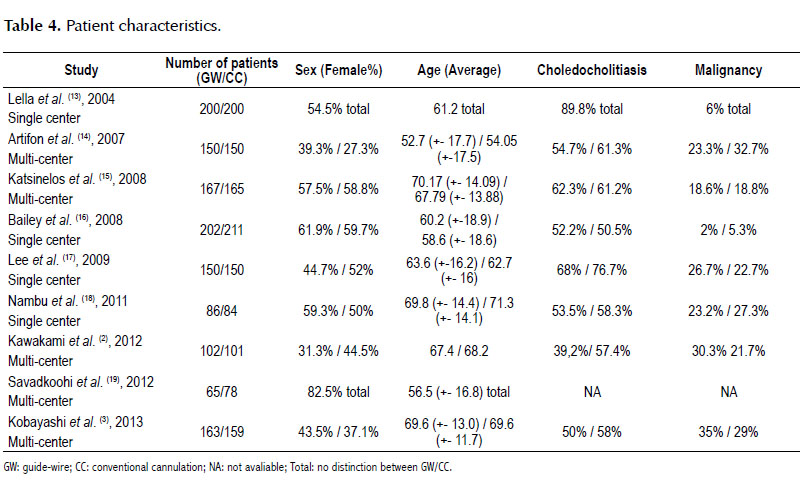
Patient characteristics are shown in Table 4.
Risk of bias within studies
All the studies scored 5 on the Jadad scale, except Savadkoohi et al. (19) which scored 3, because all studies were described as randomized, the randomization methods were described in an appropriate way, all were double-blinded using a described and appropriated method, and all had descriptions about their withdrawals.
The studies (13,14,19) did not always give strict specifications about the cannulation limit criteria and the cannulation device used. Some of them (2,16,18) described trainees starting the procedure, and one study (3) used different sizes of guide-wire in the same study. Kawakami et al. (2) used a 15-degree BOAD, which is used only in certain centers in Japan.
Results of individual studies
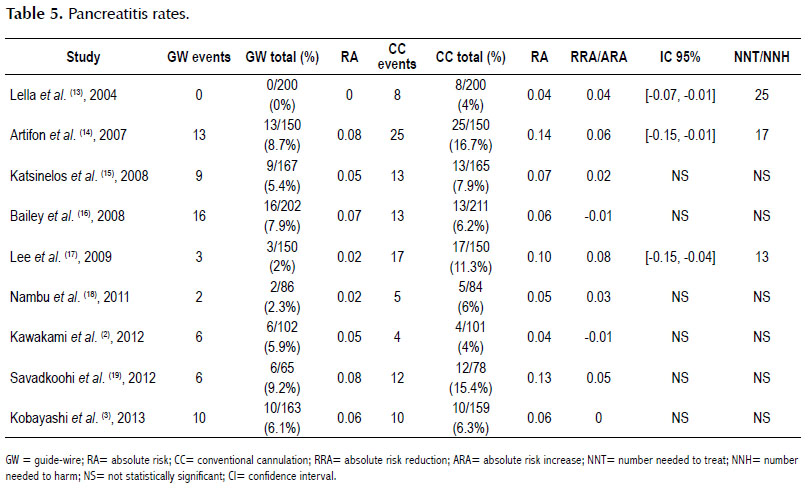
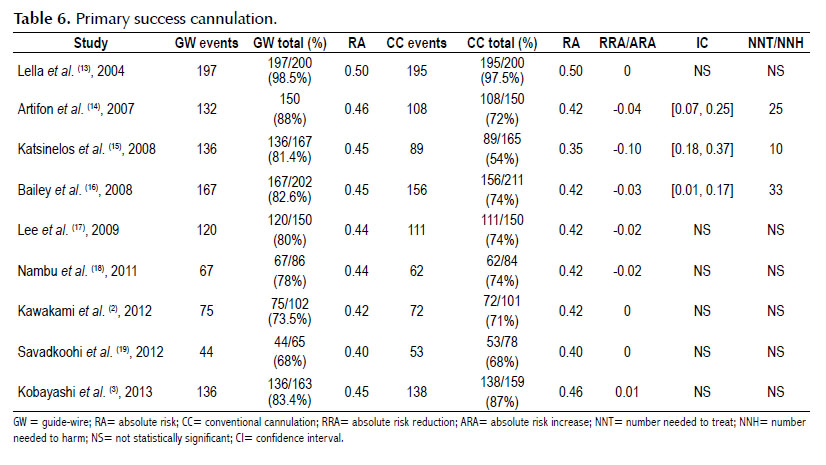
All studies had extractable information (32) about pancreatitis rates (Table 5) and primary success cannulation (Table 6).
Synthesis of results
Quantitative outcomes:
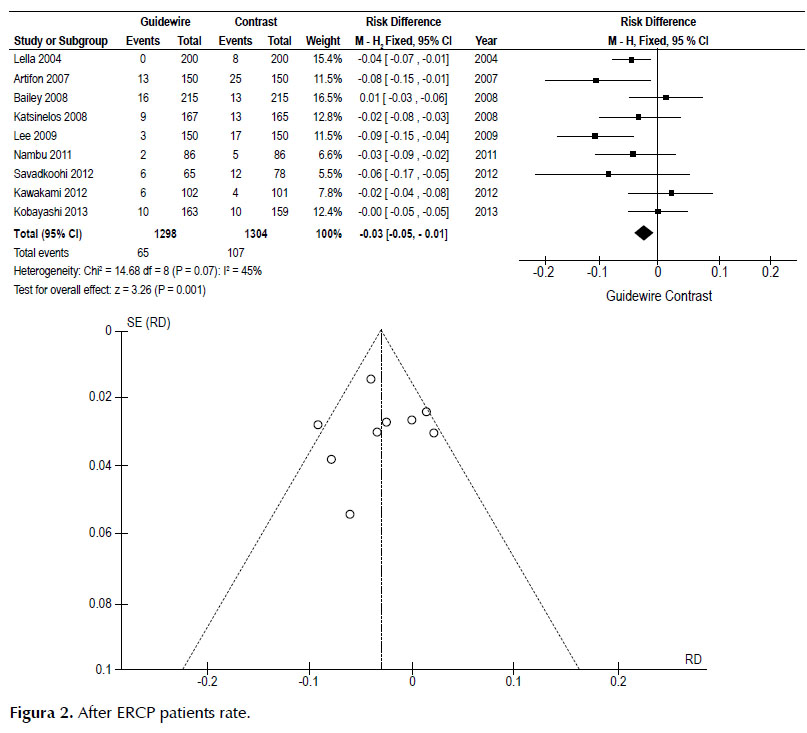
The pancreatitis rate was 3% lower in the GW group, and NNT was 33. Sensitivity analysis showed heterogeneity of 45%. Figure 2.
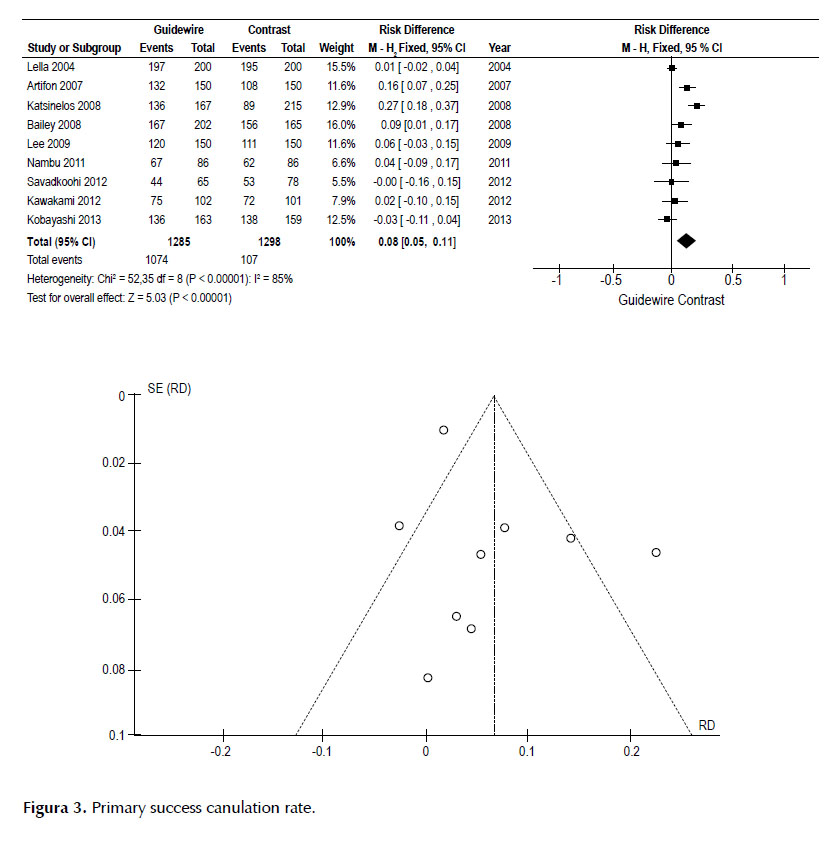
Primary success cannulation was 8% higher in the GW group, and NNT was 13, but the sensitivity analysis had an unacceptable heterogeneity of 85%. Figure 3.
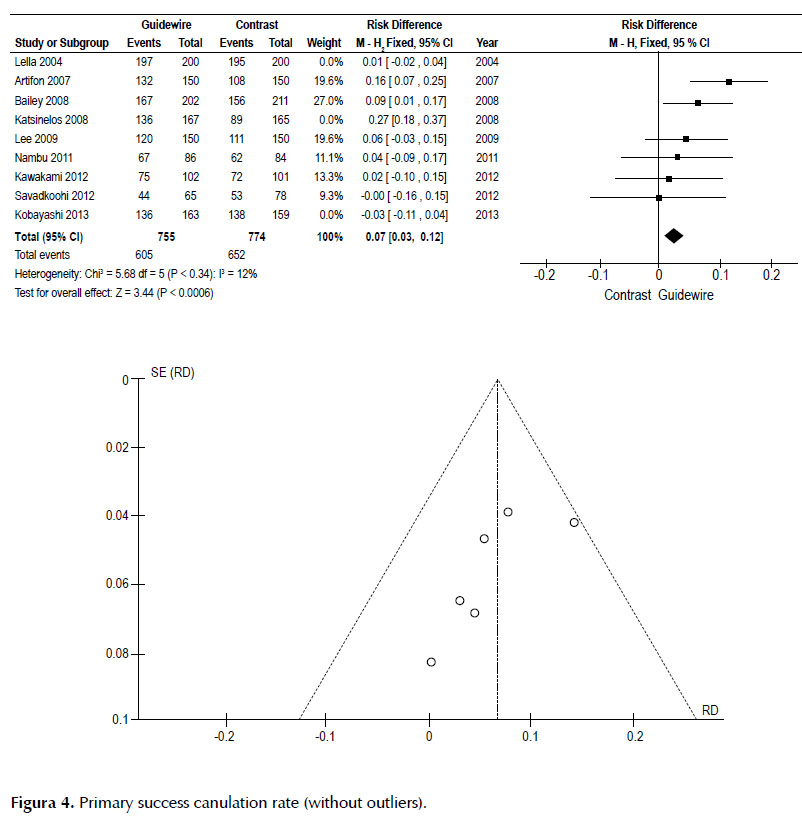
Once outliers were removed (3,13,15), (Kobayashi 2013, Lella 2004 and Katsinelos 2008), primary success cannulation, was 7% higher in the GW group, and NNT was 14witha heterogeneity of 12%. Figure 4.
Risk of bias across studies
Pancreatitis definitions varied from study to study, but they always considered, at least, patients with abdominal pain more than 24 hours post-ERCP and amylase greater than 3x. The definitions of initial cannulation success also varied between the studies. There was also bias regarding the different types of guide-wires (0.0035 inch soft tipped, 0.035 inch soft hydrophilic, with a loop in the tip, 0.035 angle-tipped, or 0.025 inch soft tipped), sphincterotomes, catheters, and duodenoscopes (with 15-degree BOAD or standard duodenoscopes) used in the studies.
Therefore, the pancreatitis rate, seen in the funnel plot, shows that Lee et al. (17) is outside the curve. This is explained by the population presence in the study; it was a low-risk cohort. Just 7/300 (2.33%) of the patients had suspected dysfunction of the sphincter of Oddy and 217/300 (72.3%) had choledocholithiasis.
Furthermore, initial cannulation success, seen in the funnel plot, shows that three RCT’s (3,13,15), were outside the curve, causing a heterogeneity of 85%. This can be explained because two of them (13,15) are extremely favored GW, and one (3) extremely favored CC, with significant discrepancies compared to other studies. Because of these huge discrepancies and losing a significant statistical difference, we withdrew these studies to have an acceptable heterogeneity, assuring that all studies remaining had homogeneous and reliable data.
Some bias across the studies (13,14,19) was introduced in that strict specifications about the cannulation limit criteria and the cannulation devices were not always given. Some of them (2,16,18) allowed a trainee to start the procedure. One study (3) used different sizes of guide-wire in the same study, and in another study (2) a 15-degree BOAD that is only used in some centers in Japan were used.
DISCUSSION
Over the years, several mechanisms have been postulated to explain why GW prevents pancreatitis. For example: inadvertent contrast injection into the pancreatic duct, facilitating selective biliary cannulation and limiting papillary trauma (33). Although, inadvertent guide wire insertion into the pancreatic duct can cause an increase in pancreatitis rate.
This meta-analysis shows that GW reduced PEP and increased initial cannulation success compared to CC.
Firstly, we must not forget that primary success cannulationis probably the most important step in ERCP because this will reduce cannulation attempts, precut sphincterotomy, use of fistulation, and inadvertent insertion into the pancreatic duct, preventing injury to the papilla.
Secondly, preventing contact to the papilla will not cause a lot of edema in the papilla, which a lot of papers affirm is the main cause of pancreatitis’s development in ERCP.
However, some recent Japanese center’s RCTs (2,3,4), suggests that introduction of the guidewire in the pancreatic duct is a risk factor for pancreatitis and that opacification of the pancreatic duct is not a risk factor for pancreatitis. This may lead some to conclude that the use, in general, of the guidewire can be a risk factor for pancreatitis.
Japanese centers result differ in that they have 15-degree BOAD duodenoscopes, and they believe that the angulation of the duodenoscope did not require the bow-up function of the sphincterotome, making it easy to adjust to the axis of the bile duct, not requiring the guidewire to facilitate primary success cannulation (34).
Unfortunately, these duodenoscopes are found only in Japan, and it is not possible to perform RCTs with them and also to use in our clinical practice or elsewhere in the world (35).
In addition, we disagree when F. Tse et al. (9), categorized these RCT’s, such as: Bailey AA et al. (16), Katsinelos P et al. (15), Kobayashi G et al. (3), Nambu T et al. (18) and Kawakami H et al. (2), such as crossover studies, because they clearly have database to be categorized as non-crossover studies and we also find a new RCT’s Savadkoohi et al. (19) that they did not select.
Differently, from the last systematic review and meta- analysis about these theme, we did not select abstract’s papers Mangiavillano B et al. (36), Apostolopoulos P et al. (37) and Mangiavillano B et al. (38) just fully text and we did not use RCT’s Cortas GA et al. (21), which the patient follow up loss was greater than 20%.
Beyond the vast equipment and materials available these days, new devices and methods are still necessary for further improvements in ERCP. Our objective of providing decision support in performing routine ERCP’s, should improve initial cannulation success and reduce pancreatitis. However, we believe new RCT’s and meta-analyses should be performed so that decisions about which new techniques of cannulation (i.e., double-guidewire cannulation, placement of a pancreatic stent, precut sphincterotome, or kindle knife access) should be used in cases of difficult cannulation.
Finally, we believe that the use of the guidewire to start ERCP should be encouraged to reduce the morbidity of the procedure and to reach primary cannulation success, but it is unacceptable to suppose that the procedure should be performed with either technique alone.
Limitations
Only pancreatitis rates and initial cannulation success rates were meta-analyzed because there were insufficient data in the studies about precut sphincterotomy, inadvertent pancreatic duct manipulation, pancreatic duct stent, and use of medications to prevent pancreatitis. The number of patients included varied greatly between studies, and some studies used only an experienced endoscopist for performing the procedures while others involved trainees.
Other complications such as bleeding, perforation, and infections had similar rates between the studies. Unfortunately, there were insufficient data to perform meta-analyses. Moreover, various types of guide-wires were used in single studies and various duodenoscopes were used between studies.
Another important limitation is the way and velocity in which the contrasts were injected during a CC cannulation. In some studies, doctors were the only ones injecting the contrast. In others, trainees and nurses injected the contrast with variable speeds.
Conclusions
Guide wire-assisted cannulation was associated with a significantly lower pancreatitis rates and higher primary success cannulation rates compared to CC.
Funding sources: The study was funded by Gastrointestinal Endoscopy Unit, Hospital das Clinicas, University of Sao Paulo Medical School.
REFERENCES
1. Baron TH. Endoscopic retrograde cholangiopancreatography. Endoscopy. 2010;42:938-43. [ Links ]
2. Kawakami H, Maguchi H, Mukai T, Hayashi T, Sasaki T, Isayama H, et al. A multicenter, prospective, randomized study of selective bile duct cannulation performed by multiple endoscopists: the BIDMEN study. Gastrointest Endosc. 2012;75(2):362-72. [ Links ]
3. Kobayashi G, Fujita N, Imaizumi K, Irisawa A, Suzuki M, Murakami A, et al. Wire-guided biliary cannulation technique does not reduce the risk of post-ERCP pancreatitis: multicenter randomized controlled trial. Dig Endosc. 2013;25(3):295-302. [ Links ]
4. Nakai Y, Isayama H, Sasahira N, Kogure H, Sasaki T, Yamamoto N, et al. Risk factors for post-ERCP pancreatitis in wire-guided cannulation for therapeutic biliary ERCP. Gastrointest Endosc. 2015;81(1):119-26. [ Links ]
5. Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37(3):383-93. [ Links ]
6. Coelho-Prabhu N, Shah ND, Van Houten H, Kamath PS, Baron TH. Endoscopic retrograde cholangiopancreatography: utilisation and outcomes in a 10-year population- based cohort. BMJ Open. 2013;3(5). doi: 10.1136/ bmjopen-2013-002689. [ Links ]
7. Navaneethan U, Konjeti R, Venkatesh PG, Sanaka MR, Parsi MA. Early precut sphincterotomy and the risk of endoscopic retrograde cholangiopancreatography related complications: an updated meta-analysis. World J Gastrointest Endosc. 2014;6(5):200-8. [ Links ]
8. Freeman ML, Guda NM. Prevention of post-ERCP pancreatitis: a comprehensive review. Gastrointest Endosc. 2004;59(7):845-64. [ Links ]
9. Tse F, Yuan Y, Moayyedi P, Leontiadis GI. Guide wire-assisted cannulation for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Endoscopy. 2013;45(8):605-18. [ Links ]
10. PROSPERO Centre for Reviews and Dissemination [Internet]. York, UK: University of York [cited 2016-02-11]. Available from: http://www.crd.york.ac.uk/PROSPERO/ [ Links ]
11. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1-12. [ Links ]
12. (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. Available in: http://tech.cochrane.org/revman [ Links ]
13. Lella F, Bagnolo F, Colombo E, Bonassi U. A simple way of avoiding post-ERCP pancreatitis. Gastrointest Endosc. 2004;59(7):830-4. [ Links ]
14. Artifon EL, Sakai P, Cunha JE, Halwan B, Ishioka S, Kumar A. Guidewire cannulation reduces risk of post-ERCP pancreatitis and facilitates bile duct cannulation. Am J Gastroenterol. 2007;102(10):2147-53. [ Links ]
15. Katsinelos P, Paroutoglou G, Kountouras J, Chatzimavroudis G, Zavos C, Pilpilidis I, et al. A comparative study of standard ERCP catheter and hydrophilic guide wire in the selective cannulation of the common bile duct. Endoscopy. 2008;404)302-7. [ Links ]
16. Bailey AA, Bourke MJ, Williams SJ, Walsh PR, Murray MA, Lee EY, et al. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post- ERCP pancreatitis. Endoscopy. 2008;40(4):296-301. [ Links ]
17. Lee TH, Park do H, Park JY, Kim EO, Lee YS, Park JH, et al. Can wire-guided cannulation prevent post-ERCP pancreatitis? A prospective randomized trial. Gastrointest Endosc. 2009;69(3 Pt 1):444-9. [ Links ]
18. Nambu T, Ukita T, Shigoka H, Omuta S, Maetani I. Wire- guided selective cannulation of the bile duct with a sphincterotome: a prospective randomized comparative study with the standard method. Scand J Gastroenterol. 2011;46(1):109-15. [ Links ]
19. Savadkoohi S, Shokri J, Savadkoohi H. Evaluation of guidewire cannulation in reduced risk of post – ERCP pancreatitis and facilitated bile duct cannulation. Caspian J Intern Med. 2012;3(1):368-71. [ Links ]
20. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1-34. [ Links ]
21. Cortas GA, Mehta SN, Abraham NS, Barkun AN. Selectivecannulation of the common bile duct: a prospectiverandomizedtrialcomparing standard catheters with sphincterotomes. Gastrointest Endosc. 1999;50(6):775-9. [ Links ]
22. Schwacha H, Allgaier HP, Deibert P, Olschewski M, Allgaier U, Blum HE.Asphincterotome-based technique for selective transpapillary common bile duct cannulation. Gastrointest Endosc. 2000;52(3):387-91. [ Links ]
23. Cheung J, Tsoi KK, Quan WL, Lau JY, Sung JJ. Guidewire versus conventional contrast cannulation of the common bile duct for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Gastrointest Endosc. 2009;70(6):1211-9. [ Links ]
24. Kouklakis G, Gatopoulou A, Lirantzopoulos N, Efraimidou E, Manolas K. Evaluation of guide wire cannulation technique in elderly patients with choledocholithiasis. J Gastrointestin Liver Dis. 2009;18(2):185-8. [ Links ]
25. Shao LM, Chen QY, Chen MY, Cai JT. Can wire-guided cannulation reduce the risk of post-endoscopic retrograde cholangiopancreatography pancreatitis? A meta-analysis of randomized controlled trials. J Gastroenterol Hepatol. 2009;24(11):1710-5. [ Links ]
26. Trifan A, Sfarti C, Cretu M, Cojocariu C, Hutanasu C, Singeap AM, et al. Guide-wire versus conventional contrast cannulation of the common bile duct for the prevention of post-ERCP pancreatitis in patients with choledocholithiasis.J Gastrointestin Liver Dis. 2011;20(2):149-52. [ Links ]
27. Nakai Y, Isayama H, Tsujino T, Sasahira N, Hirano K, Kogure H, et al. Impact of introduction of wire-guided cannulation in therapeutic biliary endoscopic retrograde cholangiopancreatography. J Gastroenterol Hepatol. 2011;26(10):1552-8. [ Links ]
28. Cennamo V, Fuccio L, Zagari RM, Eusebi LH, Ceroni L, Laterza L, et al. Can a wire-guided cannulation technique increase bile duct cannulation rate and prevent post-ERCP pancreatitis?: A meta-analysis of randomized controlled trials.Am J Gastroenterol. 2009;104:2343-50. [ Links ]
29. Mariani A, Giussani A, Di Leo M, Testoni S, Testoni PA. Guidewire biliary cannulation does not reduce post-ERCP pancreatitis compared with the contrast injection technique in low-risk and high-risk patients. Gastrointest Endosc. 2012;75(2):339-46. [ Links ]
30. Mohammad Alizadeh AH, Afzali ES, Zafar Doagoo S, Mousavi M, Mirsattari D, Shahnazi A, et al. Preventive role of wire-guided cannulation to reduce hyperamylasemia and pancreatitis following endoscopic retrograde cholangiopancreatography. Diagn Ther Endosc. 2012;2012:821376.doi: 10.1155/2012/821376 [ Links ]
31. Nakai Y, Isayama H, Sasahira N, Kogure H, Sasaki T, Yamamoto N, et al. Risk factors for post-ERCP pancreatitis in wire-guided cannulation for therapeutic biliary ERCP. Gastrointest Endosc. 2015;81(1):119-26. [ Links ]
32. Centre for Evidence-Based Medicine [Internet]. Oxford: CEBM; c2016 [cited 2016-02-11]. Available from: http://www.cebm.net/catmaker-ebm-calculators/ [ Links ]
33. Fuccio L, Cennamo V. Wire-guided biliary cannulation should be considered to be standard practice. Endoscopy. 2010;42(3):239. [ Links ]
34. Kawakami H, Maguchi H, Hayashi T, Yanagawa N, Chiba A, Hisai H, et al. A prospective randomized controlled multicenter trial of duodenoscopes with 5 degrees and 15 degrees backward-oblique angle using wire-guided cannulation: effects on selective cannulation of the common bile duct in endoscopic retrograde cholangiopancreatography. J Gastroenterol. 2009;44(11):1140-6. [ Links ]
35. Kawakami H, Isayama H, Maguchi H, Kuwatani M, Kawakubo K, Kudo T, et al. Is wire-guided selective bile duct cannulation effective for prevention of post-ERCP pancreatitis by all endoscopists? Endoscopy. 2014;46(2):163. [ Links ]
36. Mangiavillano B, Mariani A, Giussani A, et al. Guidewire assisted cannulation of the papilla of Vater to reduce the risk of post-ERCP pancreatitis: a prospective randomised study [abstract]. Endoscopy. 2007;39:A373 [ Links ]
37. Apostolopoulos P, Alexandrakis G, Liatsos C, et al. Guide wire-assisted selective access to the common bile duct could prevent post-ERCP pancreatitis [abstract]. Endoscopy. 2005;37:A278 [ Links ]
38. Mangiavillano B, Mangano M, Limido E, et al. Preliminary results on the comparison of loop-tip COOK MEDICAL® Wire vs traditional endoscopic technique cannulation in the prevention of post-ERCP pancreatitis and biliary tree access in high-risk patients [abstract]. Endoscopy. 2011;43:A86.
Correpondence:
Eduardo Turiani Hourneaux de Moura, MD Av: Dr. Enéas de Carvalho de Aguiar,255
E-mail: duduthmoura@gmail.com
APPENDIX 1
Search strategies: appendix 1 MEDLINE strategy [stratified by Population (P), Intervention (I) and Comparison (C)]: P: (Disease, Biliary Tract OR Diseases, Biliary Tract OR Bile Duct Disease OR Diseases, Bile Duct OR Bile Duct Neoplasm OR Neoplasms, Bile Duct OR Bile Duct Cancer OR Bile Duct Cancers OR Cancer of the Bile Duct OR Cancer of Bile Duct OR Common Bile Duct OR Common Bile Duct Neoplasms OR Biliary Atresia, Extrahepatic OR Biliary Atresias, Extrahepatic OR Atresia, Biliary OR Familial Extrahepatic Biliary Atresia OR Idiopathic Extrahepatic Biliary Atresia OR Bile Ducts OR abnormalities OR Cholangitides OR Cholangitis OR SclerosingCholangitides OR Sclerosing Cholangitis OR SclerosingCholangiitides OR SclerosingCholangiitis OR Primary Sclerosing Cholangitis OR Primary SclerosingCholangitides OR Cholangitis OR Sclerosis OR Choledochal Cysts OR Cyst, Choledochal OR Bile Duct Cysts OR Bile Duct Cyst OR Choledochocele OR Choledochoceles OR Congenital Choledochal Cyst OR Choledochal Cysts, Congenital OR Choledochal Cyst, Type V OR Choledochal Cyst, Intrahepatic OR Choledochal Cysts, Intrahepatic OR Choledochal Cyst, Type III OR Choledochal Cyst, Type IV OR Multiple Choledochal Cysts OR Multiple Choledochal Cyst OR Choledochal Cyst, Type I OR Cyst, Common Bile Duct OR Cysts, Common Bile Duct OR Choledochal Cyst, Type II OR Choledochal Diverticulum OR CholedochalDiverticulums OR Choledochal Cyst, Diverticulum OR Choledochal Cysts, Diverticulum OR Biliary Tract Diseases OR Cysts OR Disease, Caroli OR Caroli's Syndrome OR Caroli Syndrome OR Carolis Syndrome OR Caroli's Disease OR Carolis Disease OR Bile Duct Diseases OR congenital OR Biliary Dyskinesia OR Cholestases OR Biliary Stasis OR Biliary Stases OR Bile Duct Obstruction OR Bile Duct Obstructions OR Extrahepatic Biliary Stasis OR Extrahepatic Cholestasis OR Bile Duct Obstruction, Extrahepatic OR Bile Ducts Cholestasis OR specific extrahepatic bile duct OR Cholestases, Intrahepatic OR Bile Duct Obstruction, Intrahepatic OR Intrahepatic Cholestasis OR Biliary Stasis, Intrahepatic OR Biliary Stases, Intrahepatic OR Bile Ducts, Intrahepatic OR Liver OR Syndrome, Alagille OR Alagille's Syndrome OR Alagilles Syndrome OR Alagille-Watson Syndrome OR Arteriohepatic Dysplasia OR Cardiovertebral Syndrome OR Hepatic Ductular Hypoplasia, Syndromatic OR Hepatofacioneurocardiovertebral Syndrome OR Watson Alagille Syndrome OR Watson Miller Syndrome OR Watson-Miller syndrome OR Cholestasis with Peripheral Pulmonary Stenosis OR Alagille Syndrome 2 OR Paucity of Interlobular Bile Ducts OR Hepatic Ductular Hypoplasia OR Alagille Syndrome 1 OR Bile Ducts, Intrahepatic OR Cholestasis, Intrahepatic OR Liver Cirrhoses, Biliary OR Biliary Cirrhosis OR Obstructive Liver Cirrhosis OR Secondary Biliary Cirrhosis OR Cholangitis, Chronic Nonsuppurative Destructive OR Primary Biliary Cirrhosis OR Liver Cirrhosis, Biliary OR Mirizzi's Syndrome OR Mirizzis Syndrome OR Mirizzi Syndrome OR Biliary Tract Diseases OR Common Bile Duct Diseases OR Biliary Dyskinesias OR Dyskinesia, Biliary OR Gallbladder Dyskinesia OR Gallbladder Dyskinesias OR Sphincter of Oddi Stenosis OR Sphincter of Oddi Dyskinesia OR Sphincter of Oddi Dysfunction OR Choledocholithiasis OR Common Bile Duct OR Bile Reflux OR Biliary Tract Neoplasm OR Biliary Tract Cancer OR Biliary Tract Cancers OR Cancer of Biliary Tract OR Cancer of the Biliary Tract OR Biliary Tract Neoplasms OR Bile Duct Neoplasm OR Bile Duct Cancer OR Bile Duct Cancers OR Cancer of the Bile Duct OR Cancer of Bile Duct OR Bile Duct Neoplasms OR Common Bile Duct Neoplasms OR Cholelithiases OR Cholelithiasis OR Cholecystolithiasis OR Gallstone OR Gall Stones OR Biliary Calculi OR Gall Stone OR Common Bile Duct Calculi OR Common Bile Duct Gallstones OR Gall Stones, Common Bile Duct OR Biliary Calculi, Common Bile Duct OR Common Bile Duct Gall Stones OR Gallstones OR Cholelithiasis, Common Bile Duct OR Gallbladder Diseases OR Disease, Gallbladder OR Gall Bladder Diseases OR Bladder Disease, Gall OR Bladder Diseases, Gall OR Disease, Gall Bladder OR Gallbladder Inflammation OR Gallbladder Empyema OR Gall Bladder Empyema OR Cholecystitis OR Cholecystitis, Acalculous OR Acalculous Gallbladder Inflammation OR Acute Cholecystitis OR Cholecystitis, Emphysematous OR Cholecystolithiasis OR Gallbladder Neoplasm OR Neoplasms, Gallbladder OR Cancer of Gallbladder OR Gallbladder Cancers OR Cancer, Gallbladder OR Gall Bladder Cancer OR Bladder Cancers, Gall OR Cancer of the Gallbladder OR Postcholecystectomy Syndromes OR Syndrome, Postcholecystectomy OR Post-Cholecystectomy Syndrome OR Post- Cholecystectomy Syndromes OR Sump Syndrome OR Sump Syndromes OR Postcholedochostomy Syndrome OR Postcholedochostomy Syndromes OR Post-Choledochostomy Syndrome OR Post-Choledochostomy Syndromes OR Postcholedochoduodenostomy Syndromes OR Syndrome, Postcholedochoduodenostomy OR Post-Choledochoduodenostomy Syndrome OR Post Choledochoduodenostomy Syndrome OR Post-Choledochoduodenostomy Syndromes OR Postcholedochojejunostomy Syndrome OR Postcholedochojejunostomy Syndromes OR Syndrome, Post-Choledochojejunostomy OR Syndromes, Post-Choledochojejunostomy OR Postcholecystectomy Syndrome OR Cholecystectomy OR Postoperative Complications) AND I: (cholangiopancreatography, endoscopic retrograde OR cholangiopancreatographies, endoscopic retrograde OR ERCP OR Cholangiography) AND C: (Catheterization OR Cannulation OR Catheterizations OR Cannulations OR Catheterization* OR Catheters OR Catheters* OR Stents OR Stents* OR instrumentation* OR Drainage OR methods).
Brazilian masters and doctorate theses (CAPES) strategy: ERCP and guide-wire.
EMBASE strategy: cholangiopancreatography, AND endoscopic AND retrograde OR cholangiopancreatographies, AND endoscopic AND retrograde OR ercp OR cholangiography AND (catheterization OR cannulation OR catheterizations OR cannulations OR catheterization* OR catheters OR catheters* OR stents OR stents* OR instrumentation* OR drainage OR methods), (filter: [controlled clinical trial]/lim OR [randomized controlled trial]/lim).
Cochrane strategy: ‘cholangiopancreatography, AND endoscopic AND retrograde OR cholangiopancreatographies AND endoscopic AND retrograde OR ercp OR cholangiography AND (catheterization OR cannulation OR catheterizations OR cannulations OR catheterization* OR catheters OR catheters* OR stents OR stents* OR instrumentation* OR drainage OR methods) - (filter: randomized controlled trials).
LILACS or CENTRAL strategy: cholangiopancreatography retrograde endoscopy (filter- randomized controlled trials).
SCOPUS strategy: (cholangiopancreatography AND endoscopic AND retrograde OR cholangiopancreatographies AND endoscopic AND retrograde OR ERCP OR cholangiography AND (catheterization OR cannulation or catheterizations OR cannulations OR catheterization)) AND (LIMIT-TO (DOCTYPE, "ar") OR LIMIT-TO (DOCTYPE, "re")) AND (LIMIT-TO (LANGUAGE, "English") OR LIMIT-TO (LANGUAGE, "Spanish")) AND (LIMIT-TO (SUBJAREA, "MEDI")).
Recibido: 08-04-2016
Aprobado: 27-08-2016