Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Gastroenterología del Perú
versión impresa ISSN 1022-5129
Rev. gastroenterol. Perú vol.36 no.4 Lima oct./dic. 2016
ARTÍCULOS ORIGINALES
Temporal trends and regional variations in gastrointestinal cancer mortality in Peru, 2005-2014
Tendencia y variaciones regionales de la mortalidad por cáncer gastrointestinal en Perú, 2005-2014
Akram Hernández-Vásquez1, Guido Bendezú-Quispe2, Diego Azañedo3, Bertha Huarez4, Belén Rodríguez-Lema1
1 Universidad de Buenos Aires. Buenos Aires, Argentina.
2 Facultad de Salud Pública y Administración. Universidad Peruana Cayetano Heredia. Lima, Peru.
3 Instituto de Investigación, Universidad Católica los Ángeles de Chimbote. Chimbote, Peru.
4 Oficina General de Información y Sistemas, Instituto Nacional de Salud. Lima, Peru.
ABSTRACT
Objective: To estimate and analyze the evolution of mortality rates of gastrointestinal (GI) cancer in Peru and its regions between 2005-2014. Material and methods: We performed a nationwide secondary analysis of Peru’s Health Ministry registry of deaths during the period 2005-2014, with a focus on regional differences. Deaths registered with codes C15 to C25 (malignant neoplasms of digestive organs) from the ICD-10 were included. Calculation of age-standarized mortality rates and years of life lost (YLL) due to GI cancer per 100,000 habitants were also performed. Results: Data of 67,527 deaths from GI cancers was analyzed, 35,055 (51.91%) were women. In 2005, the number of GI cancer deaths was 6,484, for 2014, 7,532 cases were recorded. The GI cancer age-standarized mortality rates at the country level showed a decrease of 12.70% between 2005-2014. Stomach cancer presented the highest age-standarized mortality rate despite showing a downward trend in the last years, equal for gallbladder, liver and biliary tract, and esophagus cancer. Colorectal, small intestine and anus cancer show a progressive increase. In 2014, Callao (48.8), Huancavelica (48.5), La Libertad (39.6), Lambayeque (40.5) and Huanuco (38.9) had the highest rates. The three types of GI cancers with the highest rates of YLL in 2014 were stomach cancer (118.51), followed by liver and biliary tract cancer (58.68) and colorectal (44.86). Conclusion: GI cancer mortality in Peru is high and a priority issue in regions like Huancavelica, Huanuco, Callao, La Libertad and Lambayeque. Stomach cancer remains the most frequent GI cancer, but with a downward trend in the study period.
Keywords: Gastrointestinal neoplasms; Cancer; Mortality; Epidemiology; Peru (source: MeSH NLM).
RESUMEN
Objetivo: Estimar y analizar la evolución de las tasas de mortalidad de cáncer gastrointestinal (GI) en el Perú y sus regiones entre 2005-2014. Material y métodos: Se realizó un análisis secundario del registro de defunciones del Ministerio de Salud de Perú para el período 2005-2014 con los códigos C15 a C25 (neoplasias malignas de los órganos digestivos) de la versión 10 de la Clasificación Internacional de Enfermedades, además se calculó tasas de mortalidad ajustadas y años de vida perdidos (AVP) debido a cánceres GI por 100 000 habitantes. Resultados: Se analizaron datos de 67 527 muertes por cáncer GI, 35 055 (51,91%) eran mujeres. En 2005, el número de muertes fueron 6484; en 2014, hubo 7532 casos. Las tasas de mortalidad ajustadas a nivel nacional mostraron una disminución del 12,70% entre 2005-2014. El cáncer de estómago presentó la mayor tasa de mortalidad ajustada a pesar de mostrar una tendencia a la baja en los últimos años, igual para el cáncer de la vesícula biliar, del hígado y vías biliares y esófago. El cáncer colorrectal, de intestino delgado y de ano, mostraron tendencia al aumento. En 2014, Callao (48,8), Huancavelica (48,5), La Libertad (39,6), Lambayeque (40,5) y Huánuco (38,9) tuvieron las tasas más altas. Los tres tipos de cáncer GI con las tasas más altas de AVP en 2014 fueron el cáncer de estómago (118,51), cáncer de hígado y vías biliares (58,68) y colorrectal (44,86). Conclusión: La mortalidad por cáncer GI en Perú es alta, siendo un tema prioritario en regiones como Huancavelica, Huánuco, Callao, La Libertad y Lambayeque. El cáncer de estómago sigue siendo el cáncer GI más frecuente, pero con una tendencia descendente.
Palabras clave: Neoplasias gastrointestinales; Cáncer; Mortalidad; Epidemiología; Perú (fuente: DeCS BIREME).
INTRODUCTION
According to GLOBOCAN approximately 8.2 million people died of cancer in 2012 and 14.1 million new cases were registered. In both situations, more than half of them occurred in less developed regions (1). In Latin America and the Caribbean, the age-standarized incidence of cancer is estimated to be 177 cases per 100,000 populations, and although it does not exceed that of regions such as Europe and North America, it is accompanied by a high mortality rate that exceeds a million deaths each year (1).
In Peru, the Ministry of Health estimated a total of 30,792 cancer deaths in 2011 (60% were older than 60 years) with an age and sex-age-standarized rate of 107 deaths per 100,000 population (2). Another study conducted at the National Institute of Neoplastic Diseases (INEN) reported an annual incidence of 150 cases of cancer per 100,000 populations, in which 75% were diagnosed in advanced stages with chances of recovery or survival decreasing according to location (3).
The economic impact of cancer is high even for developed countries. In Peru in 2004, 378,050 years of healthy life lost (DALYs) due to this disease were estimated (4). The late diagnosis and lack of access to health services for cancer patients could be responsible for the high mortality rates in countries where the percentage of gross domestic product allocated to the health sector is low and variable (5). In addition to the shortage and low quality of cancer health services, their unequal distribution in large urban centers limits access for rural and low-income population (6).
In Peru, stomach cancer ranks first in mortality among all cancers, with an standarized rate of 17 cases per 100,000 populations for 2011, presenting a higher mortality in the Andean area. This cancer belongs to gastrointestinal (GI) cancer, which includes a group of neoplasms that affect the digestive system, including esophagus, gallbladder, liver, pancreas, stomach, small and large intestine, rectum and anus, with some of those being reported in the ranking of higher cancer mortality in the country. The development of GI cancer is related to alcohol and tobacco use, high-calorie diet, sedentary lifestyle and low intake of fruits and vegetables, all of which are the main factors associated with DALYs (2,7), and along with the demographic transition and consequent increase in population life expectancy, could favor the development of new cancer cases in the Peruvian population (2,8).
Given the high mortality associated with some cancers of gastrointestinal origin and the economic burden of these pathologies, this article aims to estimate and analyze the evolution of mortality rates of GI cancer in Peru and its regions between 2005-2014, and its impact expressed in years of life lost prematurely (YLL), in order to acknowledge the current landscape of this problem and observe trends in mortality by GI cancer in Peru.
MATERIAL AND METHODS
We performed a secondary analysis of Peru's Ministry of Health registry of deaths. Individual records of deaths nationwide during the period 2005-2014 under codes C15 to C25 (Malignant neoplasms of digestive organs) of the 10th version of the International Classification of Diseases (ICD-10) were included. These codes include esophageal malignant neoplasms (C15), malignant neoplasms of stomach (C16), malignant neoplasms of the small intestine (C17), malignant neoplasms of colon, rectosigmoid junction and rectum (C18-20), malignant neoplasms of anus and anal canal (C21), malignant neoplasms of liver and intrahepatic bile canaliculi (C22), malignant neoplasms of gallbladder, and other unspecified parts of biliary tract (C23-24) and malignant neoplasms of pancreas (C25). The C26 code corresponding to non-specific malignancies was not included.
The unit of analysis was each of the 25 regions of Peru. Population data for each region and study years were obtained from the National Series of the Instituto Nacional de Estadística e Informática of Peru (http:// webinei.inei.gob.pe:8080/sirtod-series/).
Both sources of information were consolidated into a spreadsheet in Microsoft Excel 2013 (Microsoft, Redmond, WA, USA), where tables and graphs were constructed with the absolute frequencies of mortality for GI cancer according to cancer site, sex, year and region. The spreadsheet was then exported to Stata version 14.1 (StataCorp LP, College Station, TX, USA), for calculations of GI cancer age-standardized mortality rates and YLL. The standardization of mortality rates was conducted by the direct method according to world standard population and grouped into 17 age groups of the World Health Organization (WHO) (9). The trends in the GI cancer studied were estimated and those with the highest frequency were graphed. For the calculation of the YLL, 80 years was chosen as life expectancy for both sexes taking as reference the male life expectancy at birth of the modified 26th Princeton West model life table (10). The value of YLL was reported by 100,000 inhabitants and was estimated at a national and regional level for all GI cancers included in the C15-C25 codes of ICD-10. No correction was made for underreporting of mortality because this procedure is done with general indicators for the country that might not account for the differences in mortality between regions, and the lack of epidemiological information on regional underreporting of cancer mortality serve as a correction parameter for each region of analysis (11).
The study did not require approval from an ethics committee as an ecological study using pooled secondary data in which identification of individual subjects is not possible.
RESULTS
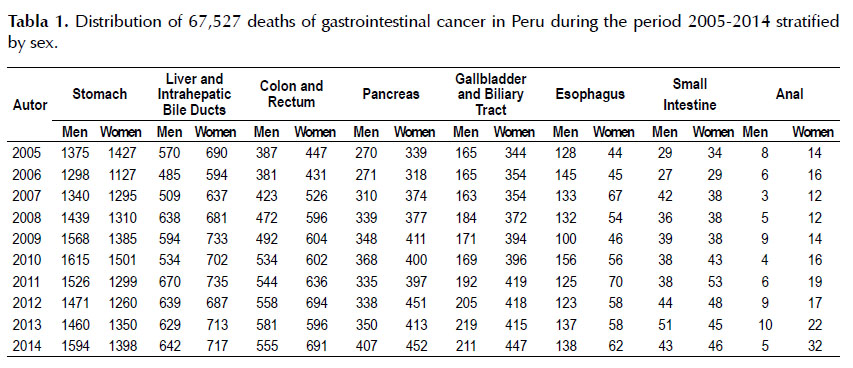
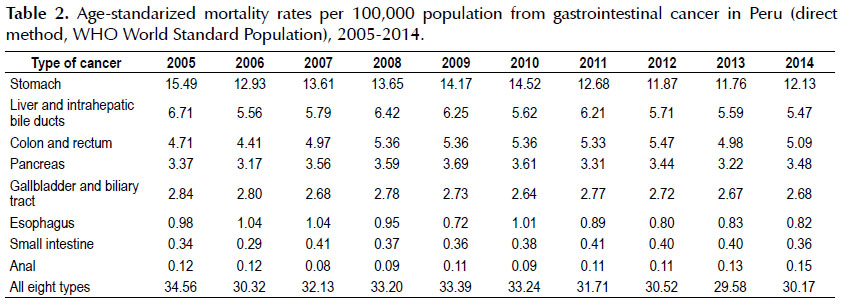
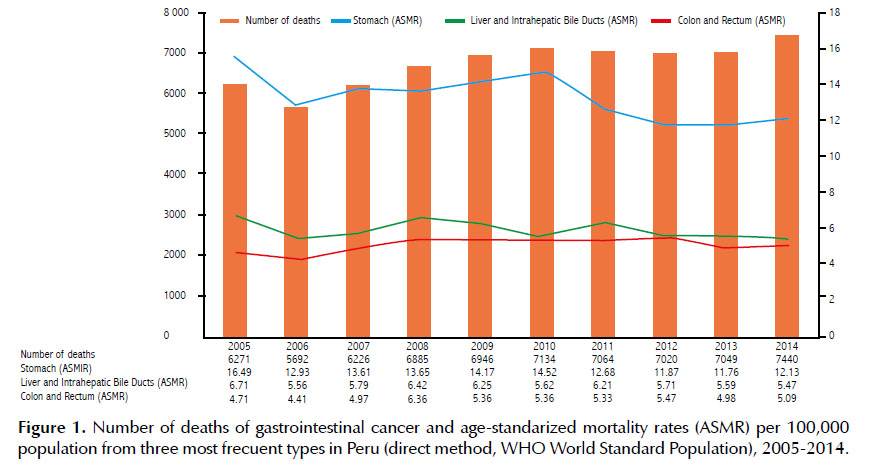
During 2005-2014, a total of 67,527 GI cancer deaths occurred, of which 32,472 (48.09%) were men and 35,055 (51.91%) women. In 2005, the number of GI cancer deaths was 6,484, with 3,043 (46.93%) cases in men and 3,441 (53.07%) in women; and for 2014, 7,532 cases were recorded, of which 3,644 were males and 3,888 females (Table 1). Gastric cancer accounted for the highest number of deaths in the study period with 28,038 cases, followed by liver and bile ducts (12,799) and colorectal (10,750) cancer (Table 1). The GI cancer standardized mortality rates at the country level showed a decrease of 12.70% between 2005 and 2014 (34.56 compared to 30.17 per 100,000 population). Age-standardized mortality rates for stomach cancer, liver, and biliary tract, and colorectal cancer in 2014 had values of 12.13; 5.47 and 5.09 per 100,000 population, respectively (Table 2).
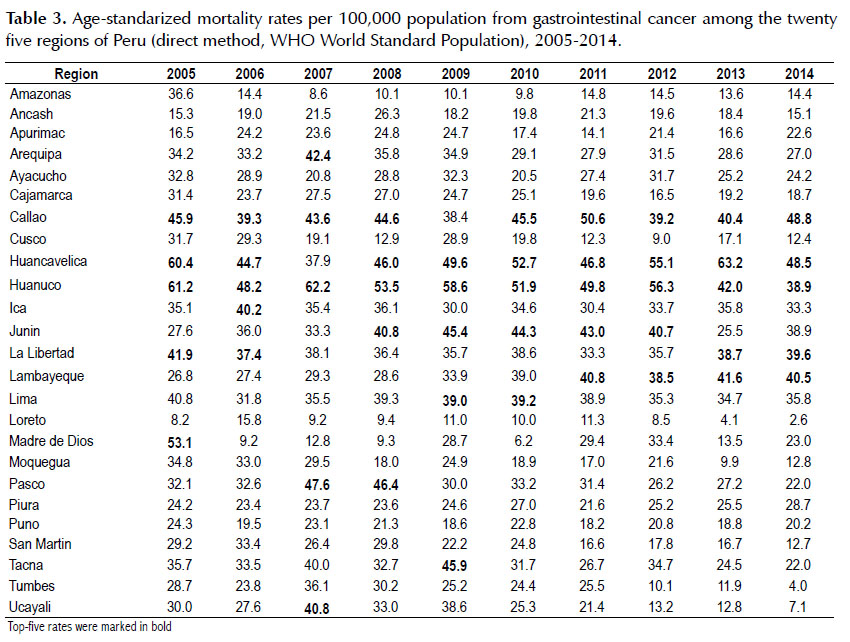
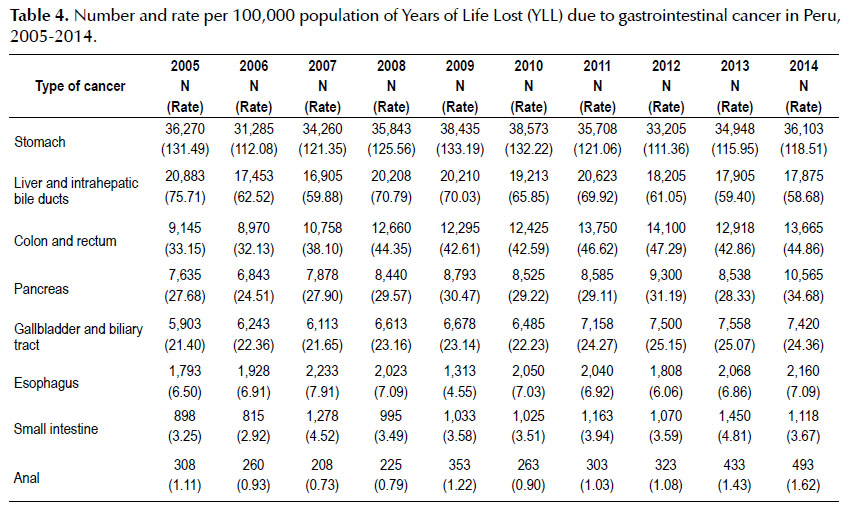
At the regional level, for 2005, Huanuco, Huancavelica, Madre de Dios, Callao and La Libertad showed the highest GI cancer standardized mortality rates being 61.2; 60.4; 53.1; 45.9 and 41.9 per 100,000 population, respectively. However, in 2014, Callao (48.8), Huancavelica (48.5), La Libertad (39.6), Lambayeque (40.5) and Huanuco (38.9) had the highest rates (Table 3). The three types of GI cancer with the highest rates of YLL in 2014 were stomach cancer with 118.51 per 100,000 people, followed by liver and biliary tract cancer with 58.68 and colorectal cancer with 44.86 (Table 4).
In the study period, 14,686 stomach cancer deaths were registered in men and 13,352 in women.
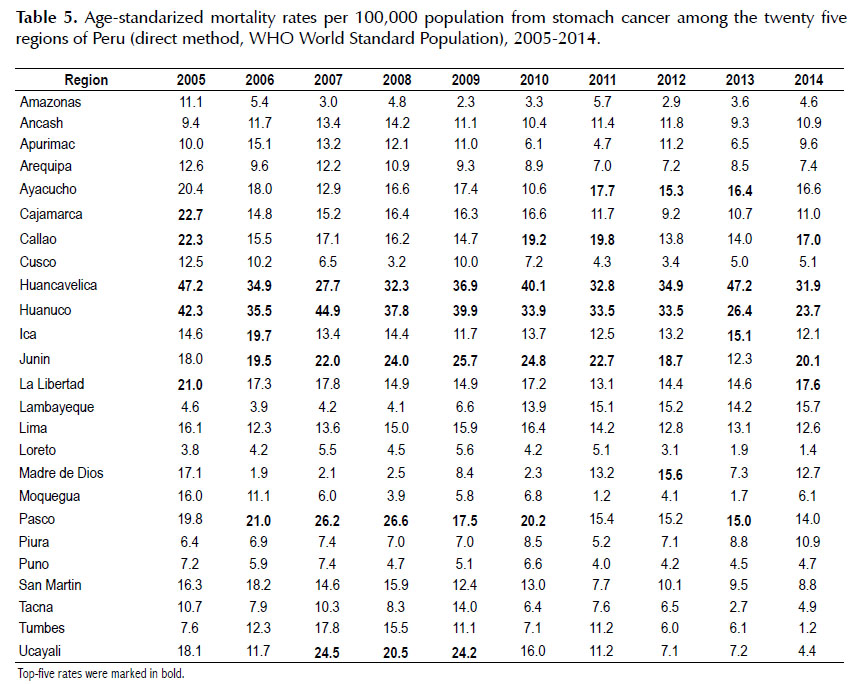
The highest age-standardized mortality rates in 2014 occurred in Huancavelica (31.9 cases per 100,000population), Huanuco (23.7) and Junin (20.1) (Table 5). In addition, a downward trend in stomach cancer mortality rates was observed in recent years (Figure 1).
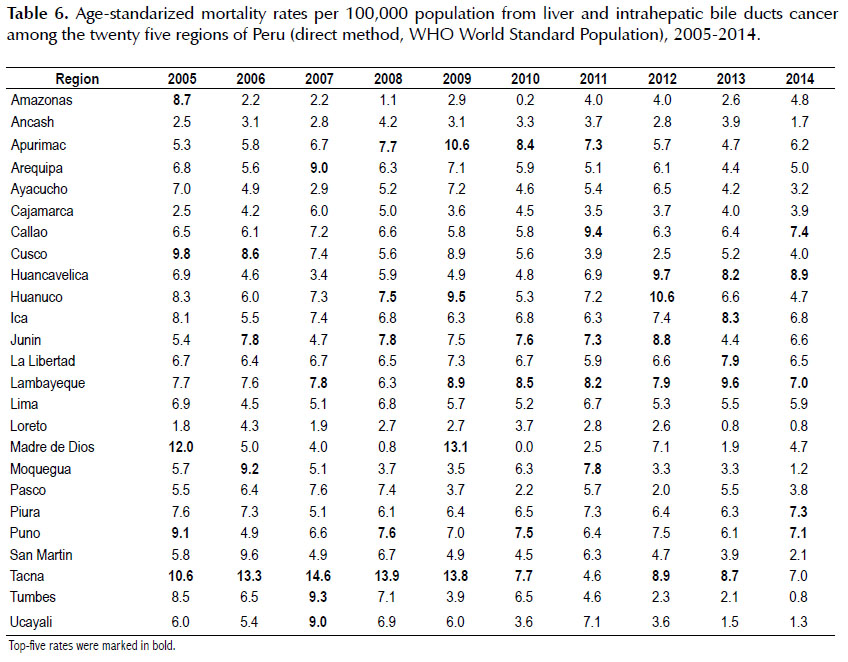
In 2005, liver cancer presented the highest agestandardized mortality rate in Madre de Dios (12.0), Tacna (10.6) and Cusco (9.8); while in 2014, the regions with the highest rates were Huancavelica, Callao, and Piura with 8.9; 7.4 and 7.3 cases per 100,000 population, respectively (Table 6), also showing a downward trend in deaths during the study period (Figure 1), as with esophagus and gallbladder cancer (Table 2).
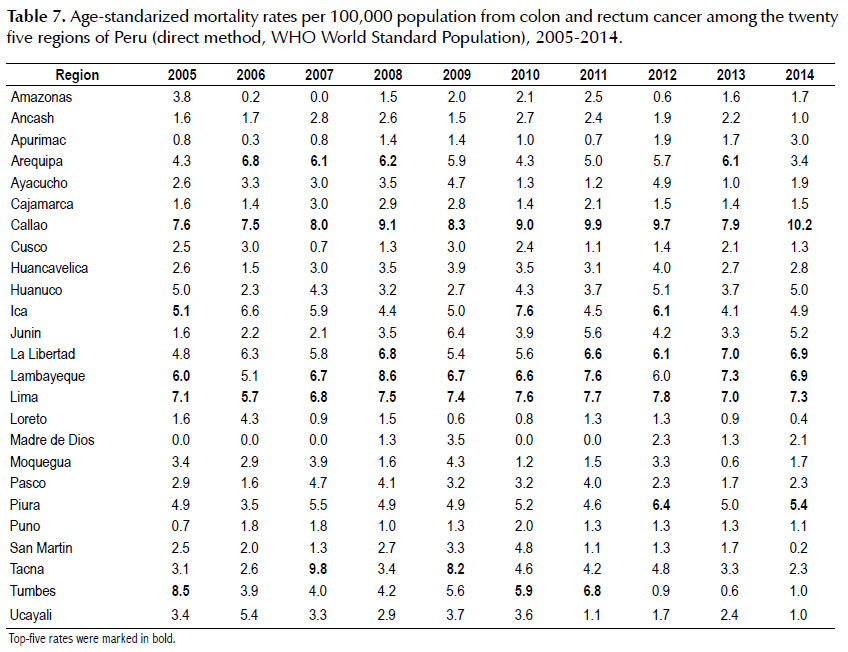
In 2005, the regions with the highest colorectal cancer age-standardized mortality rates were Tumbes (8.5), Callao (7.6) and Lima (7.1); while in 2014 the highest rates were found in Callao (10.6), Lima (7.3) and both Lambayeque (6.9) and La Libertad (6.9) (Table 7), showing a slight increase in mortality rate for this cancer (Figure 1), as in small intestine and anus cancer (Table 2).
DISCUSSION
Globally, stomach, liver and biliary tract and colorectal cancers are at the top of mortality rates ranking, only behind lung cancer according to GLOBOCAN 2012 (1). In Peru, these three types of GI cancers showed the highest mortality and would rank first, second and fifth nationwide respectively (2). GLOBOCAN estimations show an increased mortality of these GI cancers for 2030 by 87%, 91% and 83.6% respectively (1). It is also noted that other GI cancer such as the esophagus and pancreas cancer are among the ten leading causes of cancer deaths nationwide(2), highlighting the need to continue prevention and early diagnosis programs to mitigate the future social and economic impact of these health problems.
Between 2005 and 2014 in Peru, stomach, liver and biliary tract and colorectal cancer have been the leading cause of the increased mortality. Stomach cancer presented the highest age-standardized mortality rate despite showing a downward trend in the last years, also being reported for liver and biliary tract, esophagus and gallbladder cancer. Although some cancers showed a progressive increase such as colorectal, small intestine and anus; pancreatic cancer maintained an unchanged trend over time. Meanwhile, gastric cancer generates most of the YLL, followed by the liver and biliary tract and colorectal cancers.
Most GI cancer deaths are in women, which are in line with the global picture, which can be explained by the greater longevity of females for biological and social reasons as well as for an earlier onset of cancer and lower survival in men (1,12,13).
Gastric cancer was found to be the GI cancer with the highest mortality, as informed by a national report that marks it as cancer with the highest standardized mortality rate from all cancers (2). By the year 2012 one million new cases of gastric cancer worldwide were estimated, of which 77% were reported in developing countries, ranking third worldwide considering all cancer deaths (1). Between 2005-2014, gastric cancer showed a decline of 3.36 percentage points in the age-standardized mortality rate, possibly due to an improvement in the conditions of access to potable water. However, in the regions of Huancavelica, Huanuco, and Junin, those with the highest mortality, there is still insufficient access to drinking water for the inhabitants of rural areas (14) and difficulties in the provision of this service (2,15) could partly explain this problem, by favoring H. pylori transmission which significantly increases the risk of developing gastric cancer (16).
Liver and biliary tract cancers were found to be the second most common GI cancer in the country, although with a slight downward trend in deaths during the study period. Globally for 2012, about one million new cases were expected, where 83% occurred in less developed countries, causing the second highest cancer mortality rate (1). Viral hepatitis and its relationship with liver cancer is another important research point; so that a recently published study shows that there is great variability in the presentation mode of this disease in developing countries like Peru, where the therapy algorithms based on evidence generated in developed countries would have little use, urging the authors to evaluate management guidelines for this problem (17).
Colorectal cancer ranked third in GI cancer mortality according to our findings, with an increasing trend for the study period. This cancer is the third most common in men and second in women worldwide (1), ranking third in mortality in Asia (18) and second in Europe (19). Factors such as overweight and obesity, both very prevalent in the Peruvian population (20), as well as a fiber intake less than 50% of the amount recommended (21), would condition its presence as a problem for the country. To this day, no screening methods have been ideal for this disease (22), thereby necessitating the promotion of healthy lifestyles, nutrition and early detection programs for the Peruvian population.
With regard to other types of GI cancer, anal cancer mortality presented a rising trend in the study period. It is known that this cancer increased its incidence in the recent decades, mostly being associated with human papilloma virus (HPV), and other factors such as smoking, sexual practices, and sexually transmitted infections, with homosexual men being one of the groups with the highest increase of cases (23,24). Esophageal cancer showed a decrease in the number of deaths according to our findings, this being in line with global trends and explained by a decreasing prevalence of risk factors such as tobacco and alcohol use (2), both of which being related to squamous cell histological type of cancer, highlighting the increase of adenocarcinoma type of cancer which is associated with gastroesophageal reflux disease and obesity (22), problems that must be acknowledged in order to control them.
On the other hand, pancreatic cancer, maintains a stable trend over time, in line with the global trend for both sexes. This type of cancer characterized by the number of deaths being similar to its incidence, due to its poor prognosis and short survival; would benefit from controlling factors such as smoking and obesity (1,25). Gallbladder cancer has been declining in the Peruvian population according to our results, with prevention of obesity useful in maintaining this trend (26,27). Small intestine cancer showed an increase in mortality in Peru; studies carried out in U.S. and Franceindicate an increase in the number of cases (28,29), and as for pancreatic cancer, these respond to multiple risk factors, such as tobacco and alcohol use, both to be controlled in order to reduce the proportion of cases of this disease (30,31).
At the regional level, the Informe Situacional de Cáncer in Peru reports the degrees of vulnerability to cancer, taking into account variables such as the Human Development Index (HDI), standardized mortality rates, diagnostic and therapeutic capabilities, human resources in health and education, and health coverage, with Huanuco, Ayacucho, Huancavelica, Amazonas, Loreto and Pasco being highly vulnerable regions and in need of immediate intervention (2). Comparatively to our findings, only two regions (Huancavelica and Huanuco) would match this need for immediate action, while regions such as Lambayeque, La Libertad, and Callao, listed as regions with high GI cancer mortality in our study period, were not included as vulnerable regions. While our study only considers the problem of GI cancer in relation to regional variations in mortality, we believe that the prioritization of interventions aimed at cancer in Peru must take into account a territorial view, as associated factors could be exerting its effects differently between and within regions. Identifying priority areas for interventions and improving the access to cancer services for these regions is very much needed considering the low number of cancers diagnosed by screening and high diagnostic rate of final stage cancers (2).
Our study found that by 2014 the most common causes of GI cancer´s YLL corresponded to stomach, colorectal and liver and biliary tract cancer, a situation similar to that observed in the region of Latin America and the Caribbean (32). Regarding the burden of disease in Peru, for 2012, a total of 5,800,949 DALYs and 192.5 cases per 1,000 population were calculated, 53.3% being men and 47.8% of these DALYs corresponding to YLL, with malignant tumors being the third largest cause of DALYs in the age group over 60 years (33). The Institute for Health Metrics and Evaluation stated that by 2013, stomach, colorectal and liver and bile ducts cancer generated 91,964.64; 38,498.26 and 43,906.11 DALYs respectively (32), and according to the results of the Global Burden of Disease 2010, between 20052010, there was an increase of 6% in YLL for gastric cancer, going from the sixteenth to the twelfth position in the ranking of leading causes of YLL (34).
According to the INEN, 75% of cancers are diagnosed in advanced stages (involving the spread of cancer from the site of origin to distant organs of the body) (3). The introduction of the Plan Esperanza by the Peruvian Government, a program that uses resources from the Fondo Intangible Solidario en Salud (FISSAL), seeks to reduce morbidity and mortality from cancer in the country through improved access to health promotion, prevention, early detection, diagnosis, treatment and palliative care. It includes coverage for cervical cancer, breast cancer, lymphomas, leukemias, prostate, colon, and stomach cancer. This program reports that by June 2015, 132,635 Peruvians with cancer who were members of the Seguro Integral de Salud (SIS) were treated free of charge through FISSAL (35), this being an important breakthrough for the country, where the amount of money spent on cancer treatments is often catastrophic for most of the population, affecting the economic stability of households with a member with oncological pathology (36). Although other cancers continue to be covered within the portfolio of services of Peruvian health public insurance, a prioritization of interventions for patients diagnosed with liver cancer would be important because of its high mortality, and to emphasize the promotion of healthy lifestyles in the population and decreased exposure to GI cancer risk factors. The opening of Regional Institutes of neoplastic diseases in the south and north of the country, as well as increasing the membership in the SIS would allow an increase in the number of Peruvians offered care for oncological problems, increasing the diagnosis of tumors in less advanced stages and decreasing families’ expenditure.
This study has limitations related to the use of secondary sources of information, including the possibility of having incorrect or incomplete data, even more for cancer-related death events, in which the pathological diagnosis is essential in a country with low supply of oncologic health services and quality problems of mortality reports. However, we consider that the use of mortality records would provide an approach to the current scenario of cancer mortality in the country, and it is therefore necessary to have a good information and surveillance system of this public health problem, making epidemiological information available for implementation strategies, as well as to evaluate the effectiveness of current prevention measures.
In conclusion, GI cancer mortality in Peru is significantly evident, being a priority issue in regions like Huancavelica, Huanuco, Callao, La Libertad and Lambayeque, where the highest mortality rates were registered. Stomach cancer remains the most frequent GI cancer, but with a downward trend in the study period. Colorectal cancer is presented as a problem to be addressed by the country due to its increased incidence according to the current global scenario, and anal cancer being another cancer type which showed an increase in recent years of study. The GI cancer could be causing a significant number of YLL, therefore we believe that in order to better understand the landscape of cancer in the country, its factors and impact on the health of the Peruvian population; it is necessary to strengthen national plans for prevention and early diagnosis of cancer, in addition to promoting healthy lifestyles and reducing risk factors in the population. Likewise, the adoption of systems improvement in the registration of mortality in the country would provide the opportunity to improve decision-making in health based on real data, this being an engine for improving the health system and the basis for formulating health policies, such as the current Plan Esperanza. If not implemented, cancer will continue to generate a high burden on the health system and households.
Funding sources: self - funded.
Conflicts of interest: The authors declare no conflicts of interest.
REFERENCES
1. Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 Cancer Incidence and Mortality Worldwide [Internet]. Lyon, France: International Agency for Research on Cancer; 2013 [cited 27 July 2016]. Available at: http://globocan.iarc.fr [ Links ]
2. Dirección General de Epidemiología. Análisis de la Situación del Cáncer en el Perú, 2013 [Internet]. Lima, Perú: Ministerio de Salud; 2013 [cited 27 July 2016]. Available at: http:// www.dge.gob.pe/portal/docs/asis_cancer.pdf [ Links ]
3. Salazar MR, Regalado-Rafael R, Navarro JM, Montanez DM, Abugattas JE, Vidaurre T. El Instituto Nacional de Enfermedades Neoplásicas en el control del cáncer en el Perú. Rev Peru Med Exp Salud Publica. 2013;30(1):105-12. [ Links ]
4. Velásquez A, Seclén Y, Poquioma E, Cachay C, Espinoza R. Munayco C. La carga de enfermedad y lesiones en el Perú: Ajustado con datos nacionales de morbilidad y mortalidad [Internet]. Lima, Perú: MINSA/USAID; 2009 [cited 30 July 2016]. Available at: http://www.ins.gob.pe/ repositorioaps/0/0/jer/ult_inv_evi_cie2010/La%20carga%20 de%20la%20Emfermedad.pdf [ Links ]
5. The World Bank. Health nutrition and population statistics database [Internet]. Washington: The World Bank; 2016 [cited 26 July 2016]. Available at: http://data.worldbank.org/ data-catalog/health-nutrition-and-population-statistics [ Links ]
6. Velasquez-De Charry LC, Carrasquilla G, Roca-Garavito S. Equidad en el acceso al tratamiento para el cáncer de mama en Colombia. Salud Publica Mex. 2009;51(suppl 2):246-53. [ Links ]
7. Institute for Health Metrics and Evaluation. GBD Peru 2013 [Internet]. Seattle: IHME; 2016 [cited1 August 2016]. Available at: http://www.healthdata.org/peru [ Links ]
8. Huicho L, Trelles M, Gonzales F, Mendoza W, Miranda J. Mortality profiles in a country facing epidemiological transition: an analysis of registered data. BMC Public Health. 2009;9:47. [ Links ]
9. Ahmad O, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. [Internet]. Geneva Switzerland: WHO; 2000 [cited 5 July 2016]. Available at: http://www.who.int/healthinfo/paper31.pdf?ua=1 [ Links ]
10. Coale A, Guo G. Revised regional model life tables at very low levels of mortality. Popul Index. 1989;55(4):613-43. [ Links ]
11. Pineros M, Ferlay J, Murillo R. Cancer incidence estimates at the national and district levels in Colombia. Salud Publica Mex. 2006;48(6):455-65. [ Links ]
12. Cook MB, McGlynn KA, Devesa SS, Freedman ND, Anderson WF. Sex disparities in cancer mortality and survival. Cancer Epidemiol Biomarkers Prev. 2011;20(8):1629-37. [ Links ]
13. Dorak MT, Karpuzoglu E. Gender differences in cancer susceptibility: an inadequately addressed issue. Front Genet. 2012;3:268. [ Links ]
14. Instituto Nacional de Estadística e Informática. Perú: Evolución de los indicadores de los objetivos de desarrollo del milenio al 2010 [Internet]. Lima, Perú: INEI; 2012 [cited20 July 2016]. Available at: https://www.inei.gob.pe/media/MenuRecursivo/ publicaciones_digitales/Est/Lib1147/Libro.pdf [ Links ]
15. Cariampoma Arroyo A, Villegas Vega P. El acceso universal al agua potable. La experiencia peruana. Derecho PUCP. 2016;(76):229-50. [ Links ]
16. Guggenheim DE, Shah MA. Gastric cancer epidemiology and risk factors. J Surg Oncol. 2013;107(3):230-6. [ Links ]
17. Ruiz E, Rojas Rojas T, Berrospi F, Chavez I, Luque C, Cano L, et al. Hepatocellular carcinoma surgery outcomes in the developing world: a 20-year retrospective cohort study at the National Cancer Institute of Peru. Heliyon. 2016;2(1):e00052. [ Links ]
18. Pourhoseingholi MA, Vahedi M, Baghestani AR. Burden of gastrointestinal cancer in Asia: an overview. Gastroenterol Hepatol Bed Bench. 2015;8(1):19-27 [ Links ]
19. Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49(6):1374-403. [ Links ]
20. Ministerio de Salud del Perú (MINSA). Un gordo problema: Sobrepeso y obesidad en el Perú [Internet]. Lima, Perú: Ministerio de Salud; 2012 [cited 3 May 2016]. Available at: http://www1. paho.org/nutricionydesarrollo/wp-content/uploads/2012/05/ Gordo-problema.-Sobrepeso-y-Obesidad-Peru.pdf [ Links ]
21. Ministerio de Salud del Perú (MINSA). Encuesta Nacional de Indicadores Nutricionales, Bioquímicos, Socioeconómicos y Culturales Relacionados con las Enfermedades Crónicas Degenerativas [Internet]. Lima, Perú: MINSA; 2006 [cited 30 July 2016]. Available at:http://www.minsa.gob.pe/portada/ Especiales/2007/nutricion/publicaciones/INFORME_FINAL_ ENIN.pdf [ Links ]
22. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87-108. [ Links ]
23. Stanley MA, Winder DM, Sterling JC, Goon PK. HPV infection, anal intra-epithelial neoplasia (AIN) and anal cancer: current issues. BMC Cancer. 2012;12:398. [ Links ]
24. Shiels MS, Kreimer AR, Coghill AE, Darragh TM, Devesa SS. Anal cancer Incidence in the United States, 1977–2011: distinct patterns by histology and behavior. Cancer Epidemiol Biomarkers Prev. 2015;24(10):1548-56. [ Links ]
25. International Agency for Research on Cancer. World cancer report 2014. Geneva: WHO; 2014. [ Links ]
26. Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6(2):172-87. [ Links ]
27. Hundal R, Shaffer EA. Gallbladder cancer: epidemiology and outcome. Clin Epidemiol. 2014;6:99-109. [ Links ]
28. Bilimoria KY, Bentrem DJ, Wayne JD, Ko CY, Bennett CL, Talamonti MS. Small bowel cancer in the United States: changes in epidemiology, treatment, and survival over the last 20 years. Ann Surg. 2009;249(1):63-71. [ Links ]
29. Lepage C, Bouvier AM, Manfredi S, Dancourt V, Faivre J. Incidence and management of primary malignant small bowel cancers: a well-defined French population study. Am J Gastroenterol. 2006;101(12):2826-32. [ Links ]
30. Wu AH, Yu MC, Mack TM. Smoking alcohol use, dietary factors and risk of small intestinal adenocarcinoma. Int J Cancer. 1997;70(5):512-7. [ Links ]
31. Kaerlev L, Teglbjaerg PS, Sabroe S, Kolstad HA, Ahrens W, Eriksson M, et al. Is there an association between alcohol intake or smoking and small bowel adenocarcinoma? Results from a European multi-center case-control study. Cancer Causes Control. 2000;11(9):791-7. [ Links ]
32. Institute for Health Metrics and Evaluations. GBD Data Tool [Internet]. Seattle: IHME; 2016 [cited 25 July 2016]. Available at: http://www.healthdata.org/gbd-data-tool [ Links ]
33. Ministerio de Salud del Perú (MINSA). La carga de Enfermedad y Lesiones en el Perú. Mortalidad, incidencias, prevalencias, duración de la enfermedad, discapacidad y años de vida saludables perdidos [Internet]. Lima, Perú: MINSA; 2008 [cited 20 July 2016]. Available at: http://www.ins.gob.pe/repositorioaps/0/0/jer/ult_inv_evi_cie2010/La%20carga%20 de%20la%20Emfermedad.pdf [ Links ]
34. Institute for Health Metrics and Evaluation. GBD Profile: Peru [Internet]. Seattle: IHME; 2016 [cited 28 July 2016]. Available at: http://www.healthdata.org/sites/default/files/ files/country_profiles/GBD/ihme_gbd_country_report_ peru.pdf [ Links ]
35. Ministerio de Salud del Perú (MINSA). Memorias Plan esperanza [Internet]. Lima, Perú: MINSA; 2015 [cited 20 July 2016]. Available at: ftp://ftp2.minsa.gob.pe/descargas/ogc/ boletines/Memoria-Plan-EsperanzaPERU.pdf [ Links ]
36. Gutiérrez S, Cornejo K, Leyva D. Cáncer: costos de tratamiento en Perú. [Internet]. Lima, Perú: Acción internacional para la salud; 2009 [cited 7 July 2016]. Available at: http://www. aislac.org/recursos/acceso-a-medicamentos-esenciales/ publicaciones25/376-cancercostos-de-tratamiento-en-peru-2/file [ Links ]
Correspondence:
Akram Abdul Hernández Vásquez Calle Gavilán 3856, Buenos Aires, Argentina E-mail: akram.hernandez.v@upch.pe
Recibido: 28-07-2016
Aprobado: 22-09-2016