Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Gastroenterología del Perú
versión impresa ISSN 1022-5129
Rev. gastroenterol. Perú vol.37 no.1 Lima ene./mar. 2017
ARTÍCULOS ORIGINALES
Endoscopic gastrostomy: critical analysis in a regional referral hospital
Gastrostomía endoscópica: análisis crítico en un hospital referencial regional
Gabriel Marques Fávaro1a, Tiago Franco Vilela1a, Diego Soares Coca1a, Marco Antonio Buch Cunha2, Ricardo Sato Uemura2, Carlos Kyoshi Furuya Júnior2, Dayse Aparício2, Everson L. A. Artifon3
1 Digestive Endoscopy Departament, Hospital Ana Costa. Santos-SP, Brazil.
a Resident
ABSTRACT
Introduction: Percutaneous endoscopic gastrostomy (PEG) is a safe and effective endoscopic surgical procedure for enteral access and gastrointestinal decompression, and it is an excellent alternative to surgical gastrostomy. There are various clinical indications and these mainly include the need for prolonged enteral nutritional support due to complications from neurological, geriatric and oncological diseases and decompression of the gastrointestinal tract. Although safe and effective, a number of possible complications relating to the time (early or late complications) and severity (minor or major complications) may occur. Objective: To evaluate the indications and complications relating to PEG among selected patients at the digestive endoscopy service of a regional referral hospital. Materials and methods: A retrospective study on patients who underwent PEG between May 2013 and April 2015 was conducted. The patients were identified through searching the medical records and using a standardized data form. Results: 53 cases were analyzed. The average age was 70.47 years and 60.37% of the patients were women. The main indication identified was the need for enteral nutritional support, and 73.58% of these indications were derived from neurological complications, 15.09% from geriatric complications and 9.43% from oncological complications and 1.88% were due to gastrointestinal decompression. Complications occurred in 24.52% of the cases: 23.07% were major and 76.93% were minor. Regarding the time, there were eight cases of late complications and five of early complications. Conclusion: PEG was shown to be an effective and safe method for enteral access. The indication and complication rates were similar to those reported in the literature.
Keywords: Gastrostomy; Endoscopy; Complications (source: MeSH NLM).
RESUMEN
Introducción: La gastrostomía endoscópica percutânea (GEP) es un procedimento endoscópico-quirúrgico seguro y efectivo para el acceso enteral y para la descompresión gastrointestinal, constituyéndose como una excelente alternativa a la gastrostomía quirúrgica. Las indicaciones clínicas son variadas y comprenden principalmente: necesidad de soporte nutricional enteral prolongado por complicaciones de las enfermedades neurológicas, geriátricas y oncológicas, así como la descompresión del tracto gastrointestinal. Aunque es segura y eficaz, se puede producir una serie de posibles complicaciones relacionadas al momento (precoz temprano o tardío) de la realización del procedimiento y a la gravedad (mayor o menor). Objetivo: Evaluar las indicaciones y complicaciones relacionadas a la realización de la GEP en pacientes seleccionados de un sector de endoscopia digestiva de un hospital regional de referencias. Materiales y métodos: Fue realizado un estudio retrospectivo de los pacientes sometidos a la GEP en el periodo de mayo de 2013 a abril de 2015. Los pacientes fueron identificados a partir de la investigación de los registros y formulario estándar de datos. Resultados: Fueron analizados 53 casos. La edad media fue de 70,47 años con un 60,37% del sexo femenino. La indicación principal verificada fue la necesidad de soporte nutricional enteral, siendo 73,58% por complicaciones neurológicas, 15,09% geriátricas, 9,43% oncológicas; y 1,88% de las indicaciones fueron para descomprensión gastrointestinal. Ocurrieron complicaciones en 24,52% de los pacientes: 23,07% mayores y 76,93% menores. En relación al momento, fueron verificados ocho casos de complicaciones tardías y cinco de complicaciones precoces (tempranas). Conclusión: La GEP se mostró como un método eficaz y seguro para el acceso enteral. Los índices de complicación fueron semejantes a los datos evidenciados en la literatura.
Palabras clave: Gastrostomía; Endoscopía; Complicaciones (fuente: DeCS BIREME).
INTRODUCTION
Percutaneous endoscopic gastrostomy (PEG) is an endoscopic surgical procedure that is used to provide prolonged enteral nutrition for patients with limited capacity for oral ingestion whose gastrointestinal tract is functional (1-3). The objective in performing PEG is not only to improve these patients nutritional status and life expectancy, but also to improve their quality of life, which is not necessarily correlated with nutritional improvement (4).
PEG was first described by Dr. Michael W. L. Gauderer in the United States during the 1970s and it has become widely disseminated since then (5). Today, several techniques for performing the procedure exist, among which the traction technique is the one most used (6).
There are various clinical indications and these include the need for prolonged enteral nutritional support (more than four weeks) due to incapacity for oral feeding caused by complications from neurological, geriatric and oncological diseases; decompression of the gastrointestinal tract; and others (administration of unpalatable medications, gastric fixation in cases of volvulus or diaphragmatic hernia and furnishing of a gastric access for endoscopic procedures (5,7).
The two main indications for performing PEG are the need for prolonged enteral access in patients without the capacity for sufficient oral ingestion due to reversible or irreversible neurological dysfunctions; and decompression of the gastrointestinal tract (8).
Contraindications have also been mentioned in a diversity of worldwide consensuses and guidelines. Several conditions relating to patients’ general state, comorbidities, anatomical abnormalities or other factors may make it impossible to perform PEG either definitively (absolute contraindications) or momentarily (relative contraindications) (9).
The absolute contraindications include: refusal to agree with the free and informed consent statement; severe coagulopathy; hemodynamic instability and sepsis; severe ascites; peritonitis; infection of the abdominal wall at the site selected for puncture; signs of peritoneal carcinomatosis; interposition of organs (for example, the liver, spleen and colon); previous history of total gastrectomy; obstruction of the gastric outlet; and severe gastroparesis (6).
The main relative contraindications involve: presence of neoplasms of the oropharynx or esophagus, since these represent a potential risk of implantation of tumor cells along the path of the PEG; previous abdominal surgery; hepatosplenomegaly; peritoneal dialysis; and portal hypertension with esophageal and gastric varices (8,10).
It should be emphasized that three basic safety principles need to be respected in performing PEG: gastric distension during the endoscopy; viewing of finger pressure on the anterior gastric wall and transillumination of the abdominal wall (8).
The present study had the objective of evaluating the indications and complications relating to performing PEG on selected patients at a digestive endoscopy service in a regional referral hospital.
MATERIALS AND METHODS
A retrospective study was conducted with 53 patients who underwent PEG at the Hospital, between May 2013 and April 2015.
The exclusion criteria were: previous subtotal gastrectomy surgery; obstructive head-and-neck or esophageal tumor impervious to passage of a 9.8 mm conventional device; refusal by the patient; or absence of visible transillumination during the PEG procedure.
The patients were identified through searching the medical records and by a study entry form. Only the patients who have signed the free and informed consent statement were described in this study.
The PEG procedures selected for analysis were performed by means of the traction technique, using a video gastroscope (Pentax EPK-1000). Kits were used for the primary percutaneous enteral access (EndoVive PEG pull, Boston Scientific®), along with exchange devices (Tri-Funnel, BARD®).
All the examinations were conducted by two trained endoscopists. The patients underwent sedation, aided by an anesthesiologist. Intravenous antibiotic prophylaxis using a first-generation cephalosporin (Kefazol® 2g) was administered 30 minutes before each procedure, for the patients who were not already using broad-spectrum antibiotics.
All the variables were firstly described descriptively. For the quantitative variables, this analysis comprised observation of the minimum and maximum values and calculation of the means, standard deviations and medians. For the qualitative variables, the absolute and relative frequencies were calculated. To test the homogeneity between the proportions, the chi-square or Fisher exact test was used. The significance level used for the tests was 5%.
RESULTS
Among the 53 patients analyzed, 32 (60.38%) were female and 21 (39.62%) male. Their mean age was 70.47 years, with a minimum of 16 years and maximum of 93 years; 70% were aged 65 years or over. The median age was 77 years.
The indications for the PEG procedure were neurological diseases (73.58%), followed by geriatric and oncological diseases (15.1% and 9.4%, respectively). Furthermore, there were a small number of indications for decompression of the gastrointestinal tract (1.9%).
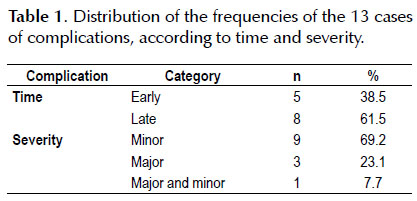
Regarding the time and severity of the complications, 61.5% were late complications and 69.2% were minor complications (Table 1).
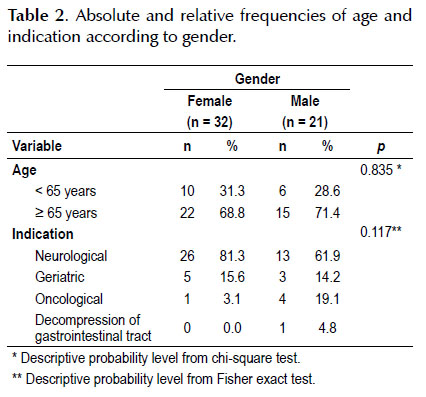
Table 2 shows a comparison of genders in relation to age and indication.
We observed that the gender groups did not present any significant difference in relation to age or indication.
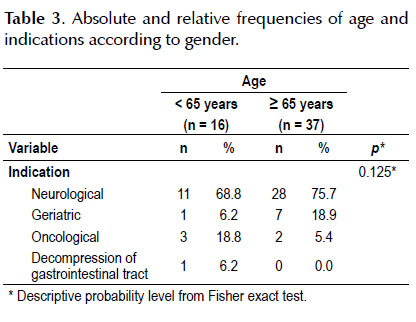
Table 3 shows a comparison between age groups and indications.
We observed that the age groups did not present any significant difference in relation to indication.
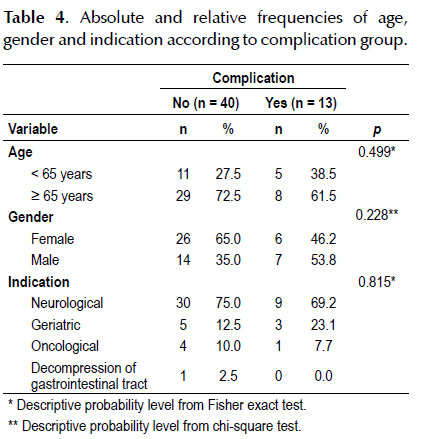
Table 4 shows a comparison between the groups with and without complications.
We observed that the groups did not present significant differences in relation to age, sex or indication.
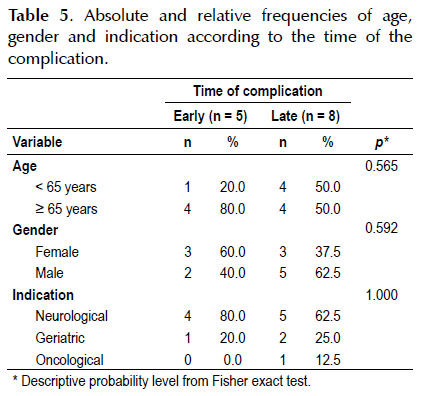
Table 5 shows a comparison between the early and late complication groups.
We observed that these groups did not present any significant differences in relation to age, sex or indication.
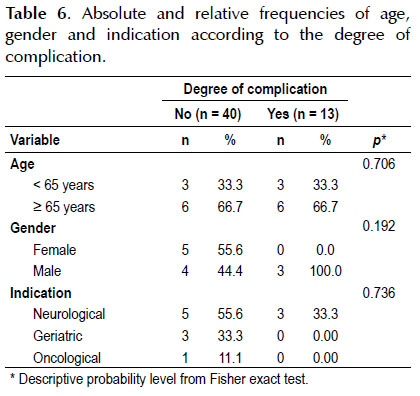
Table 6 shows a comparison between the groups of degrees of complication.
We observed that the groups did not present any significant differences in relation to age, sex or indication.
DISCUSSION
PEG has been shown to be an efficient method for interventions in cases requiring enteral nutritional support. With regard to the two main indications that are generally seen (prolonged enteral access in patients with insufficient capacity for oral ingestion due to either neurological dysfunctions or decompression of the gastrointestinal tract) (8). The present study likewise found that enteral access was most frequently indicated for patients with neurological diseases, accounting for 73.6% of the cases analyzed.
The next most frequent indication was complications resulting from problems with deglutition due to geriatric conditions, which were responsible for 15.1% of the cases. Regarding decompression of the gastrointestinal tract, there was only one case. This difference in relation to previous studies may have been due to the number of subjects included in the study. A more representative sample might have led to different percentages of indications observed.
There are other indications considered important such as obstructive lesions of the aerodigestive tract (seen in 5.66% of the cases) (7,11). However, it needs to be borne in mind that the hospital of the present study is located in a municipality in which the adult population over 55 years of age and the elderly population are greater than in other Brazilian cities, including the state capital (12). This variable may have contributed towards the considerable prevalence of neurological cases and, especially, geriatric cases. In fact, in the present study, the patients mean age was 70.47 years, without any significant difference between the genders, even though females predominated slightly, accounting for 60.4% of the sample. The mean age found and the low difference between the genders is in line with the literature (13).
Regarding the types of complications, no problems relating to upper digestive endoscopy were seen: such conditions are considered to be rare, according to the literature (8). Regarding early and late complications, a total of eight late and five early complications was seen. Among these, loss or accidental/inadvertent dislodgement of the tube was the most frequent late complication. This differ from findings in the literature, where formation of local granuloma has been reported to be the commonest late complication, with prevalence of around 43% in some studies (9). This can be explained by the absence of long and regular follow-up.
The complications relating to the PEG procedure itself can be classified as either early (within the first 15 days) or late (beyond the first 15 days). Minor complications relating to the post-procedure period are treated conservatively, while major complications may require hospitalization, transfusion of blood concentrates, endoscopic therapy and/or surgery, depending on the severity of the complication (14-19).
It has been observed that the complications classified as minor and major differ from each other (14,20). The minor complications may include: peristomal infection, self-limited bleeding, non-complicated pneumoperitoneum, extravasation of content, local granuloma, peristomal dermatitis, late accidental dislodgement, probe obstruction, probe degradation, distal migration of the probe and enlargement of the stoma, among others. The most frequent minor complications are peristomal infections (21). The major complications may include: buried bumper syndrome, high-output gastrocutaneous fistula, cellulitis, stenosis of the puncture site, peritonitis, early accidental dislodgement, perforation of hollow viscera or solid organ, aspiration, upper digestive hemorrhage and tumor implantation in the stoma, among others.
The most prevalent late complication is formation of granulation tissue in the stoma of the gastrostomy (22). Minor complications associated with PEG tend to occur more frequently than do major complications, with rates of around 13% to 43% and 0.4% to 8.4%, respectively (16).
Data gathered from the literature indicate that this procedure is considered to be safe and effective when appropriately indicated and implemented. It is more commonly performed among individuals over the age of 65 years, without any significant difference between the genders. The results from a nationwide survey conducted in the United States in 2013 showed that the mortality rate after PEG was low: only 10.8% of the patients out of a sample of 181,196 subjects died while still in the hospital. These patients’ mean age was around 70 years and proportions of men and women were similar: 51% and 49%, respectively (23). Another study that sought to determine factors that might predict mortality after PEG presented a mortality rate of 6.5%, 30 days after the procedure had been performed (24).
However, a series of possible complications of greater or lesser severity may occur at the time of the upper endoscopy, during or after performing PEG (14,15). Complications arising from upper digestive endoscopy are uncommon (frequency of 0.13%, with mortality of 0.004%) and generally occur at the time of performing the procedure (16). They include cardiopulmonary disorders, bronchoaspiration, hemorrhage and perforation (8).
It was also found, coincidentally, that the most frequent minor complication was inadvertent removal of PEG tube, in 4/53 cases, followed by peristomal infection in 2/53 cases. These data differed from the findings in some previous studies, in which infection at the puncture site was reported to be the most frequent complication, with prevalence of up to 65% (25,26).
In the present study, antibiotic prophylaxis was used systematically. This may in some way have influenced the results found. A total of four cases of major complications were found (4/53), only one consisted of buried bumper syndrome, it occurred 12 days after the procedure. This corroborates the data found in the literature generally within three weeks after the procedure is performed (6).
As described in the results section, the statistical analyses used to correlate the variables did not find any significant relationships between the variables described, including the relationships between the genders, ages, indications and complications, concerning either the time or the severity. The main variables were in accordance with the data presented in the literature.
PEG has been shown to be an important tool for enteral nutrition for patients who require nutritional support under a variety of conditions (27). The patients of the present study confirmed this. However, as a possible theme for future studies, it can be suggested that the cases undergoing this procedure should continue to be followed up, so as to gather data on complications and mortality over the medium and long terms. Furthermore, prospective studies making comparisons with other techniques for performing this type of procedure (e.g. PEG with gastropexy) could be designed in order to evaluate the reduction in the frequency of complications.
Conflict of interests: the authors have declared that no competing interests exist.
Funding: none.
BIBLIOGRAPHIC REFERENCES
1. Schröder O, Hoepffner N, Stein J. Enteral nutrition by endoscopic means; I. Techniques, indications, types of enteral feed. Z Gastroenterol. 2004;42(12):1385-92. [ Links ]
2. Nicholson FB, Korman MG, Richardson MA. Percutaneous endoscopic gastrostomy: a review of indications, complications and outcome. J Gastroenterol Hepatol. 2000;15(1):21-5. [ Links ]
3. Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, et al. Role of endoscopy in enteral feeding. Gastrointest Endosc. 2002;55(7):794-7. [ Links ]
4. Bannerman E, Pendlebury J, Phillips F, Ghosh S. A crosssectional and longitudinal study of health-related quality of life after percutaneous gastrostomy. Eur J Gastroenterol Hepatol. 2000;12(10):1101-9. [ Links ]
5. Gauderer MWL. Percutaneous endoscopic gastrostomy and the evolution of contemporary long-term enteral access. Clin Nutr. 2002;21(2):103-10. [ Links ]
6. Azar AAR, Rahnemaiazr AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: Indications, technique, complications and management. World J Gastroenterol. 2014;20(24):7739-51. [ Links ]
7. Löser C, Aschl G, Hébuterne X, Mathus-Vliegen EMH, Muscaritoli M, Niv H, et al. ESPEN guidelines on artificial enteral nutrition – percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005;24(5):848-61. [ Links ]
8. Schraq SP, Sharma R, Jaik NP, Seamon MJ, Lukaszczyk JJ, Martin ND, et al. Complications related to percutaneous endoscopic gastrostomy (PEG) tubes. A comprehensive clinical review. J Gastrointestin Liver Dis. 2007;16(4):407-18. [ Links ]
9. Mello GFS. Avaliação da gastrostomia endoscópica percutânea como procedimento ambulatorial em pacientes com câncer de cabeça e pescoço: viabilidade, complicações e impacto clínico do momento da realização pré, per ou póstratamento. [Dissertação] Rio de Janeiro: Instituto Nacional de Câncer – INCA; 2011. [ Links ]
10. Pickhardt PJ, Rohrmann CA Jr, Cossentino MJ. Stomal metastases complicating percutaneous endoscopic gastrostomy: CT findings and the argument for radiologic tube placement. Am J Roentgenol. 2002;179(3):735-9. [ Links ]
11. Ponsky JL, Gauderer MWL. Percutaneous endoscopic gastrostomy: indications, limitations, techniques and results. World J Surg. 1989;13(2):165-70. [ Links ]
12. Instituto Brasileiro de Geografia e Estatística (IBGE). Informações Estatísticas [Internet]. Río de Janeiro: IBGE; 2010 [citado el 21 de marzo de 2016]. Disponíble en: http:// cidades.ibge.gov.br/xtras/perfil.php?codmun=354850. [ Links ]
13. Schneider AS, Schettler A, Markowski A, Luettig B, Kauffman B, Klamt S, et al. Complication and mortality rate after percutaneous endoscopic gastrostomy are low and indicationdependent. Scand J Gastroenterol. 2014;49(7):891-8. [ Links ]
14. Schapiro GD, Edmundowicz SA. Complications of percutaneous endoscopic gastrostomy. Gastrointest Endosc Clin N Am. 1996;6(2):409-22. [ Links ]
15. McClave SA, Chang WK. Complications of enteral access. Gastrointest Endosc. 2003;58(5):739-51. [ Links ]
16. Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, et al. Complications of upper GI endoscopy. Gastrointest Endosc. 2002;55(7):784-93. [ Links ]
17. Fox VL, Abel SD, Malas S, Duggan C, Leichner AM. Complications following percutaneous endoscopic gastrostomy and subsequent catheter replacement in children and young adults. Gastrointest Endosc. 1997;45(1):64-71. [ Links ]
18. Mathus-Vliegen EMH. Gastrostomy and enterostomy. In: Tytgat GNJ, Classen M, Waye JD, Nakazawa S (eds.) Practice of Therapeutic Endoscopy. 2nd ed. Philadelphia: Saunders; 2000. p. 277-300. [ Links ]
19. Lin HS, Ibrahin HZ, Kheng JW, Fee W, Terris D. Percutaneous endoscopic gastrostomy: strategies for prevention and management of complications. Laryngoscope. 2001;111(10):1847-52. [ Links ]
20. Shellito PC, Malt RC. Tube gastrostomy. Techniques and complications. Ann Surg. 1985;201(2):180-5. [ Links ]
21. Lipp A, Lusardi G. A systematic review of prophylatic antimicrobials in PEG placement. J Clin Nurs. 2009;18(7):938-48. [ Links ]
22. Crosby J, Duerksen D. A retrospective survey of tube-related complications in patients receiving long-term home enteral nutrition. Dig Dis Sci. 2005;50(9):1712-7. [ Links ]
23. Arora G, Rockey D, Gupta S. High In-hospital mortality after percutaneous endoscopic gastrostomy: results of a nationwide population-based study. Clin Gastroenterol Hepatol. 2013;1(11)1:1437-44. [ Links ]
24. Zopf Y, Maiss J, Konturek P, Rabe C, Hahn EG, Schwab D. Predictive factors of mortality after PEG insertion: guidance for clinical practice. JPEN J Parenter Enteral Nutr. 2011;35(1):50-5. [ Links ]
25. Vanis N, Saray A, Gornjakovic S, Mesihovic R. Percutaneous endoscopic gastrostomy (PEG): retrospective analysis of a 7-year clinical experience. Acta Inform Med. 2012;20(4):235-7. [ Links ]
26. Preclik G, Grüne S, Leser HG, Lebherz J, Heldwein W, Machka K, et al. Prospective, randomised, double blind trial of prophylaxis with single dose of co- amoxiclav before percutaneous endoscopic gastrostomy. BMJ. 1999;319:881-4. [ Links ]
27. O’Mahoney D, McIntyre AS. Artificial feeding for elderly patients after stroke. Age Aging. 1995;24(6):533-5.
Correspondence:
Gabriel Marques Fávaro Rua Pedro Américo, 60, 10° andar, 11075-905. Santos/SP, Brazil.
E-mail: gm.favaro@hotmail.com
Recibido: 4-4-2016
Aprobado: 2-8-2016