Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Gastroenterología del Perú
versión impresa ISSN 1022-5129
Rev. gastroenterol. Perú vol.37 no.1 Lima ene./mar. 2017
REPORTE DE CASO
Penetrating gastric ulcer as a manifestation of multisystemic tuberculosis
Úlcera gástrica penetrante como manifestación de tuberculosis multisistémica
Jorge Espinoza-Ríos1a, Eduar Bravo Paredes1b,2c, José Pinto Valdivia1b,2c, Julissa Guevara1b,2c, Jorge Huerta-Mercado2c,3b, Martín Tagle Arróspide2c,3b, Alejandro Bussalleu Rivera2c,4b
1 Hospital Cayetano Heredia. Lima, Peru.
2 School of Medicine, Universidad Peruana Cayetano Heredia. Lima, Peru.
3 Clínica Angloamericana. Lima, Peru.
4 Clínica Médica Cayetano Heredia. Lima, Peru.
a Resident in Gastroenterology; b Gastroenterologist; c Professor
ABSTRACT
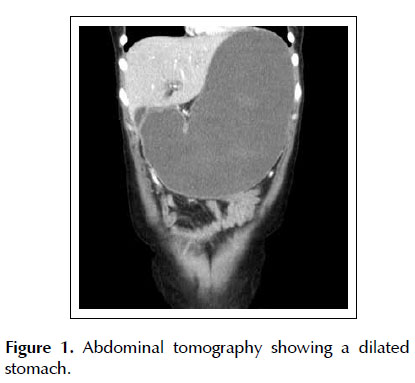
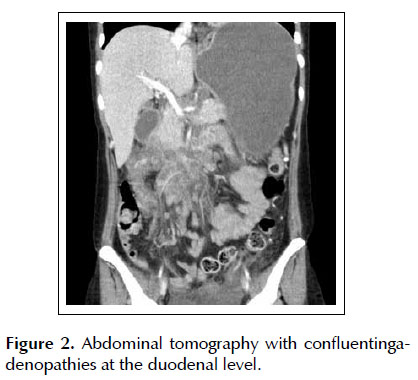
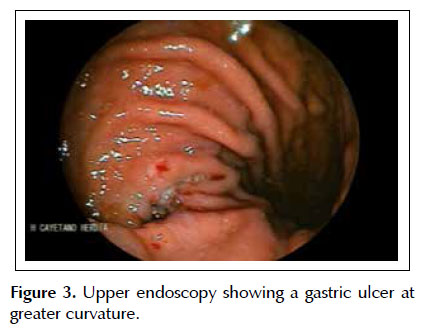
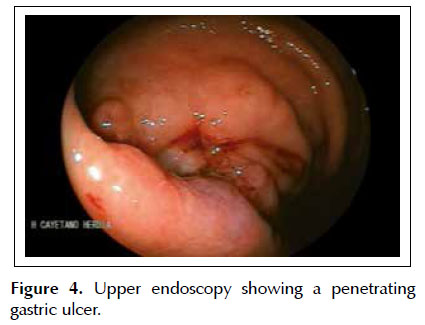
We present the case of a 30-year old female with a history of abdominal pain, fever, poor oral tolerance and weight loss for 6 months. An abdominal CT scan showed marked gastric dilatation due to extrinsic compression from lymphadenopathies around the second portion of the duodenum. The upper endoscopy revealed the presence of a penetrating gastric ulcer in the greater curvature. Biopsies of the lesions showed hystiocytes with granulomatous features and Acid Fast Bacilli (AFB) positive, and the cultures grew Mycobacterium tuberculosis sensitive to Isonazid and Rifampin. Subsequently anti-TB regimen was initiated achieving great clinical and endoscopic improvement.
Keywords: Tuberculosis, gastrointestinal; Stomach ulcer; HIV (source: MeSH NLM).
RESUMEN
Se presenta un caso de una mujer de 30 años de edad con historia de dolor abdominal, fiebre, poca tolerancia oral y pérdida de peso por 6 meses. Un CT scan abdominal muestra dilatación marcada gástrica debido a una compresión extrínseca por adenopatías alrededor de la segunda porción del duodeno. Una endoscopía alta revela la presencia de una úlcera gástrica penetrante en la curvatura mayor. Las biopsias mostraron histiocitos con granulomatosis y bacilos acid fast positivos y en los cultivos crecieron micobacterium tuberculosis sensibles a isoniacidad y rifampicina. Subsecuentemente se inició el régimen anti TBC lográndose una mejoría clínica y endoscópica evidente.
Palabras calve: Tuberculosis gastrointestinal; Úlcera gástrica; VIH (fuente: DeCS BIREME).
INTRODUCTION
Gastrointestinal tuberculosis (TBC) is still a big diagnostic challenge, since it does not manifest any classic symptoms at presentation. There is usually a diagnostic delay and at the same time an increased probability of complications, mimicking many kinds of diseases (1). There is currently an increase in the incidence of TBC in developed countries due to a higher prevalence of immunosupressed individuals (mainly HIV/AIDS), the immigrant population coming from countries with high rates of TBC, and a shortage of health services (1,2). Primary gastric TBC is rare and clinically similar to peptic ulcers or malignancy (3-6). Gastrointestinal TBC is frequently associated with pulmonary TBC, to some degree of immunodeficiency from HIV infection or close contacts with persons with the infection (7,8).
CASE REPORT
We evaluated a 30-year old female patient with a history of 6 months of intermittent fever, (predominantly nocturnal), colicky epigastric pain of moderate to severe intensity with anorexia and oral intolerance. There was a 5 kg weight loss and three weeks prior to admission she was diagnosed with HIV infection. She denied cough, hematemesis, diarrhea or melena. Abdominal examination did not reveal organomegaly or tender points. Significant laboratory examinations showed Hb 8.8 g/dL, with normal differential count, Serum creatinine 0.6 mg/dL, Total Bilirubin 0.4 mg/ dL, AST 31 IU/L, ALT 25 UI/L, Albumin 2.5 g/dL. CD4 count 15 cells/mm3, HIV RNA 270,978 copies/ml. Her chest X ray was within normal limits.
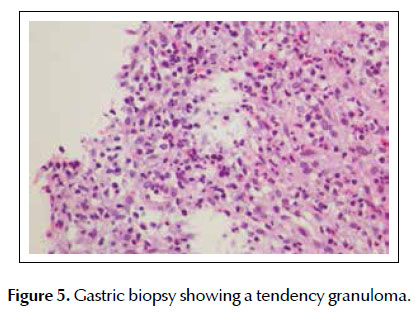
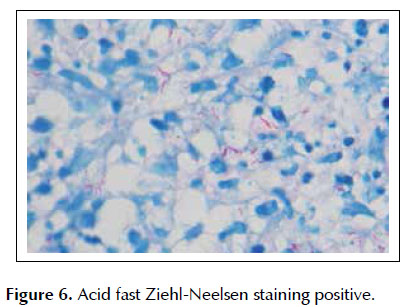
An abdominal CT scan showed marked dilatation of the stomach (Figure 1) and multiple adenopathies in the periduodenal region and around the superior mesenteric artery and vein. There was no free fluid or air or air-fluid levels (Figure 2). We performed an upper endoscopy finding a large deep ulcer in the gastric body in the lesser curvature, with prominent edges. Biopsies were taken (Figures 3 and 4), showing chronic superficial and deep gastritis, absence of H. pylori and histiocytes with a tendency to form granulomas (Figure 5). Acid-Fast Bacilli (AFB) staining was positive for mycobacteria (Figure 6). Treatment with Isonazid, Rifampin, Pirazynamide and Ethambutol was initiated, with a marked clinical improvement and reduction in size of the abdominal lymphadenopathies. The cultures confirmed the presence of Mycobacterium tuberculosis sensitive to Isonazid and Rifampin. Eight weeks later a repeat endoscopy documented disappearance of the gastric lesion.
DISCUSSION
The most frequent localization of gastrointestinal TBC is in the ileo-cecal and jejunal regions with more than 60% of cases (1,7,8). Primary gastric TBC is infrequent, probably due to bactericidal activity of gastric acid and the paucity of lymphoid tissue in the gastric mucosa (8,9). Possible routes of acquisition for the infection are oral ingestión, hematogenous spread, adjacent lymphoid nodules or contiguous TBC lesion (1,4). Patients can present non-specific symptoms such as epigastric pain, vomiting, fever, weight loss, anorexia, upper GI bleeding among others, so a high index of suspicion is required (5,10). Endoscopically gastric TBC presents frequently as ulcers, erosions or lesions mimicking a neoplasm, and can be located in the antrum, lesser curvature, pyloric channel or even in the fundus (11,12). Nodular hypertrophic lesions stenosing the pylorus has been described as well (10). Our patient had a lesion in the greater curvature. Differential diagnosis of gastric TBC includes carcinoma, lymphoma and syphilis (1).
Diagnosis should be based on histological and microbiologic study of the biopsies, and occasionally on surgical specimens(5,11) . Difficulties to obtain precise diagnoses have been reported based on AFB staining or cultures, and apparently this is due to the fact that the granulomas containing the mycobacteria are preferentially located in the submucosa, and the endoscopic biopsies are taken from the mucosa (13). For this reason, when the suspicion for TBC is high the procedure must be repeated(14). In our case the diagnosis was based on the biopsies taken from the edges of the lesion showing a granulomatous tendency (Figure 5) with AFB staining (Figure 6) confirmed by culture.
Gastrointestinal TBC usually responds to medical treatment with anti-TBC medications and early diagnosis can avoid unnecessary surgical interventions. All the patients should receive at least 6 months of therapy including 2 months with Isonazid, Rifampin, Pirazynamide and Ethambutol, followed by 4 months with Isonazid and Rifampin. Some specialists recommend extending therapy to 9 months (1). Our patient started the above mentioned therapy with clinical and endoscopic improvement, and she is currently asymptomatic and receiving therapy with high activity antiretroviral therapy (HAART).
Disclosures: Informed consent was obtained for this case report.
Interest conflicts: None.
BIBLIOGRAPHIC REFERENCES
1. Debi U, Ravisankar V, Kishor Prasad K, Kant Sinha S, Kumar Sharma A. Abdominal tuberculosis of the gastrointestinal tract: Revisited. World J Gastroenterol. 2014;20(40):14831-40. [ Links ]
2. Burzynski J, Schluger NW. The epidemiology of tuberculosis in the United States. Semin Respir Crit Care Med. 2008;29(5):492-8. [ Links ]
3. Padma V, Anand NN, Rajendran SM, Gurukal S. Primary tuberculosis of stomach. J Indian Med Assoc. 2012;110(3):187-8. [ Links ]
4. Amarapurkar DN, Patel ND, Amarapurkar AD. Primary gastric tuberculosis – report of 5 cases. BMC Gastroenterol. 2003;3:6. [ Links ]
5. Hinojosa W, Sánchez L, Espinoza R, Nago A, Watanabe J, Caller A, et al. Tuberculosis gástrica. Rev Gastroenterol Peru. 1985;5(3):128-33. [ Links ]
6. Sharma V, Rana SS, Gunjan D, Chhabra P, Sharma R, Bhasin DK. Primary gastric tuberculosis mimicking a submucosal tumor. J Dig Endosc. 2015;6(3):130-2. [ Links ]
7. Iwaki R, Bussalleu A. Tuberculosis gastrointestinal y peritoneal. Rev Gastroenterol Peru. 1994;14:99-103. [ Links ]
8. Yriberry S, Cervera Z, Soriano C, Frisancho O, Machado A, Zumaeta E. Tuberculosis digestiva en el Hospital Nacional Edgardo Rebagliati Martins (HNERM): Un estudio retrospectivo de 5 años (1993-1998). Rev Gastroenterol Peru. 1998;18(3):238-49. [ Links ]
9. Arabi NA, Musaad AM, Ahmed EE, Ibnouf MM, Abdelaziz MS. Primary gastric tuberculosis presenting as gastric outlet obstruction: a case report and review of the literature. J Med Case Rep. 2015;9(1):265. [ Links ]
10. 11Khan FY1, AlAni A, Al-Rikabi A, Mizrakhshi A, Osman Mel-M. Primary gastric fundus tuberculosis in immunocompetent patient: A case report and literature review. Braz J Infect Dis. 2008;12(5):453-5. [ Links ]
11. 10Rao YG, Pande GK, Sahni P, Chattopadhyay TK. Gastroduodenal tuberculosis management guidelines, based on a large experience and a review of the literature. Can J Surg. 2004;47(5):364-8. [ Links ]
12. Subei I, Attar B, Schmitt G, Levendoglu H. Primary gastric tuberculosis: A report and literature review. Am J Gastroenterol. 1987;82(8):769-72. [ Links ]
13. Padmanabhan H, Rothnie A, Singh P. An unusual case of gastric outlet obstruction caused by tuberculosis: challenges in diagnosis and treatment. BMJ Case Rep. 2013;2013:169051. doi: 10.1155/2013/169051 [ Links ]
14. Öztürk B, Nural MS, Ecemiş Ö, Danacı M. Imaging findings of an isolated gastric tuberculosis case mimicking lymphoma and infiltrative gastric cancer. Turk J Gastroenterol. 2015;26(1):65-6.
Correspondence:
Jorge Espinoza- Ríos Av. Del Rio N° 390, Dpto H, Urb. Bahia, Pueblo Libre (Lima 21). Lima - Peru.
E-mail : jorge.espinoza@upch.pe
Recibido: 12-2-2016
Aprobado: 2-7-2016