Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de Gastroenterología del Perú
Print version ISSN 1022-5129
Rev. gastroenterol. Perú vol.38 no.1 Lima Jan./Mar. 2018
ARTÍCULOS ORIGINALES
Prevalence of non A to E hepatitis in Mumbai, India
Prevalencia de la hepatitis no A /E en Mumbai, India
Nishtha Nagral1a, Vrunda Joshi2b, Karan Baria3b, Pathik Parikh4c, Aabha Nagral5d, Jayanthi Shastri6e, Chandrakant Pawar5f
1 BYL Nair Medical College. Mumbai, India.
2 LTM Medical College. Mumbai, India.
3 Sheth GS Medical College. Mumbai, India.
4 Department of Gastroenterology, LTM Medical College. Mumbai, India.
5 Kasturba Hospital of Infectious Diseases. Mumbai, India.
6 Department of Microbiology, Kasturba and Nair Hospital. Mumbai, India.
a Student, b Intern, c Lecturer, d Consultant Physician and Hepatologist, e Head, f Dean
ABSTRACT
Introduction: Acute viral hepatitis is a common problem in India. World wide data shows that 5 to 20 percent of this is caused by non A-E hepatitis. There is no data in India regarding non A-E hepatitis. We carried out this study to evaluate the epidemiology, clinical features, risk factors and outcome of non A-E hepatitis. Material and methods: In this single centre study, we evaluated all patients admitted with features of acute viral hepatitis at our hospital between the period of February to July 2015. A detailed history about the epidemiology, risk factors and clinical features was done. Patients were evaluated with bilirubin, transaminases and prothrombin time. Each patient was investigated for IgM HAV, IgM HEV, HBsAg and Antibody against hepatitis C. Patients turning out negative were investigated for presence of autoimmune hepatitis or Wilson’s disease. All viral markers were repeated a week later to confirm non A-E status. Results: A total 265 patients were included of which 41 (15.4%) patients were non A-E hepatitis. They had higher age (28.55 vs 34.99, p<0.05) but similar gender and sub urban location. Median SEC classification was A2 in hepatitis A/E group as compared to A3 in non A-E group. The duration of symptoms and clinical features between the two groups were similar with Anorexia, Malasie, Nausea/vomiting being most common. The risk factors between the two groups were similar. The bilirubin and transaminases were non significantly lower than hepatitis A/E patients while albumin levels were significantly lower. The outcomes of both groups were similar with no mortality or fulminant hepatitis. Conclusion: Non A-E hepatitis patients tends to be older, lower SEC class and had lower albumin levels as compared to hepatitis A/E.
Keywords: Hepatitis; Jaundice; Hepatitis C antibodies (source: MeSH NLM).
RESUMEN
Introdución: La hepatitis viral aguda es un problema común en la India. Los datos mundiales indican que el 5 al 20% es causada por hepatitis no A-E. No hay datos en la India sobre hepatitis no A-E. Objetivo: Se realiza este estudio para evaluar la epidemiología, clínica, factores de riesgo y pronóstico de la hepatitis no A-E. Material y métodos: En este estudio de un solo centro evaluamos a todos los pacientes que se admitieron con clínica de hepatitis viral aguda en nuestro hospital en el periodo de febrero a julio del 2015. Se realizó una historia detallada para evaluar la epidemiología, características clínicas. Se les tomó bilirrubinas, transaminasas y tiempo de protrombina. A cada paciente se le realizó HAV IgM, HEV IgM, HbsAg y anticuerpo anti hepatitis C. Los que fueron negativos se les estudió para hepatitis autoinmune y enfermedad de Wilson. Todos los marcadores virales se repitieron a la semana para confirmar hepatitis no A-E. Resultados: Se incluyeron 256 pacientes, 41 de ellos (15,4%) fueron hepatitis no A-E. Tuvieron más edad (28,55 vs 34,99, p<0,05), pero el mismo género y ubicación urbana. La clasificación media SEC fue A2 en el grupo hepatitis A/E, comparada con 3 en el grupo de no A-E. La duración de los síntomas y el desarrollo clínico fue similar en ambos grupos, siendo la anorexia el malestar general, las náuseas y los vómitos los más frecuentes. El factor de riesgo fue similar, al igual que las transaminasas, mientras que la albúmina fue significativamente menor. El resultado fue similar sin caso alguno de hepatitis fulminante. Conclusión: Los pacientes con hepatitis no A-E tienden a ser mayores, de clase SEC más baja y con valores de albumina más bajos que los pacientes con hepatitis A-E.
Palabras clave: Hepatitis; Ictericia; Anticuerpos contra la hepatitis C (fuente: DeCS BIREME).
INTRODUCTION
Acute viral hepatitis (AVH) is a systemic infection predominantly affecting the liver and it continues to be a major public health problem in India. Acute viral hepatitis is caused by mainly hepatitis A, hepatitis E and non A to E viral hepatitis. Hepatitis B and hepatitis C rarely presents as a cause of acute viral hepatitis. Nearly 119,000 cases of all cause viral hepatitis were reported in India in 2012 (1). The Integrated Disease Surveillance Programme of the NCDC received notification of 290,000 cases of acute viral hepatitis in 2013. Globally, an estimated 1.4 million cases of hepatitis A virus (HAV) infection occur annually (1-3).
HEV is the most important cause of epidemic hepatitis, though HAV is more common among children. About 10 to 15 percent of patients with non-A, non-B, non E hepatitis have no evidence of hepatitis C virus (HCV) infection after extensive evaluation and can therefore be classified as having non-A–E hepatitis (4,5). Different studies have been carried out at various centers of the world to determine the clinico pathological features of this entity (4-7). The clinical picture and the prognosis of this disease vary from mild forms with minimal symptoms to acute liver failure. Some cases may become chronic, with a potential to progress to cirrhosis. Owing to the wide variability in the clinical aspects and in the biochemical and histologic characterization of this syndrome, it is important to better define the clinical patterns of the disease. However, no data is available in Indian literature regarding non A-E hepatitis. No data is available regarding the presentation or epidemiology in Indian patients. We carried out prospective study at a referral centre for viral hepatitis to determine the epidemiology, presentation and outcome of viral marker negative acute viral hepatitis.
MATERIAL AND METHODS
Design
This is a single centre study prospective study carried out at Kasturba Hospital of Infectious Diseases, Mumbai from February 2015 to July 2015. The Ethics Committee approval was sought and obtained from Institutional Ethics Committee.
Inclusion and exclusion criteria
All patients admitted with jaundice (serum bilirubin ≥3.0 mg/dl) and fulfilling the case definition of Acute viral hepatitis were included during the period of six months. Clinical case definition for acute viral hepatitis was, "an acute illness with discrete onset of symptoms (e.g. fatigue, abdominal pain, loss of appetite, intermittent nausea, vomiting) and later on developing jaundice". An informed consent was taken from each patient. All patients with history of significant alcohol (>60 grams per day for more than 5 years, with a last binge within 4 weeks before onset of jaundice), cirrhosis of liver (compensated or decompensated, diagnosed on ultrasound, serum albumin and platelets), Wilsons disease, autoimmune hepatitis and hepatitis B (HBsAg positive) were excluded. Patients with any history of hepatotoxic drug intake within 30 days prior to onset of jaundice were also excluded.
Evaluation
A detailed history regarding the epidemiological data, clinical presentations, risk factors and dietary effects were taken from all patients. All patients were classified according to SEC classification (8). All patients were examined for the signs of chronic liver disease and investigated in form of complete blood count, serum bilirubin, transaminases, alkaline phosphatise, prohrombin time, ultrasound abdomen, serum creatinine, IgM HAV, IgM HEV, HBsAg and anti hepatitis C antibody. In patients who were all markers negative were evaluated by anti nuclear antibody, anti smooth muscle antibody, ceruloplasmin, urinary copper and ophthalmic examination. The viral markers were repeated once at the interval of 15 days to rule out window period. Transaminases and bilirubin levels were repeated weekly till it normalized.
Statistics
Statistical analyses were done using chi square tests for categorical data and student’s t test for continuous data. Mean and standard error were calculated for epidemiological data. Univariate and multivariate analyses was carried out to determine the factors statistically different in non A to E hepatitis and hepatitis A/E patients.
RESULTS
Epidemiology
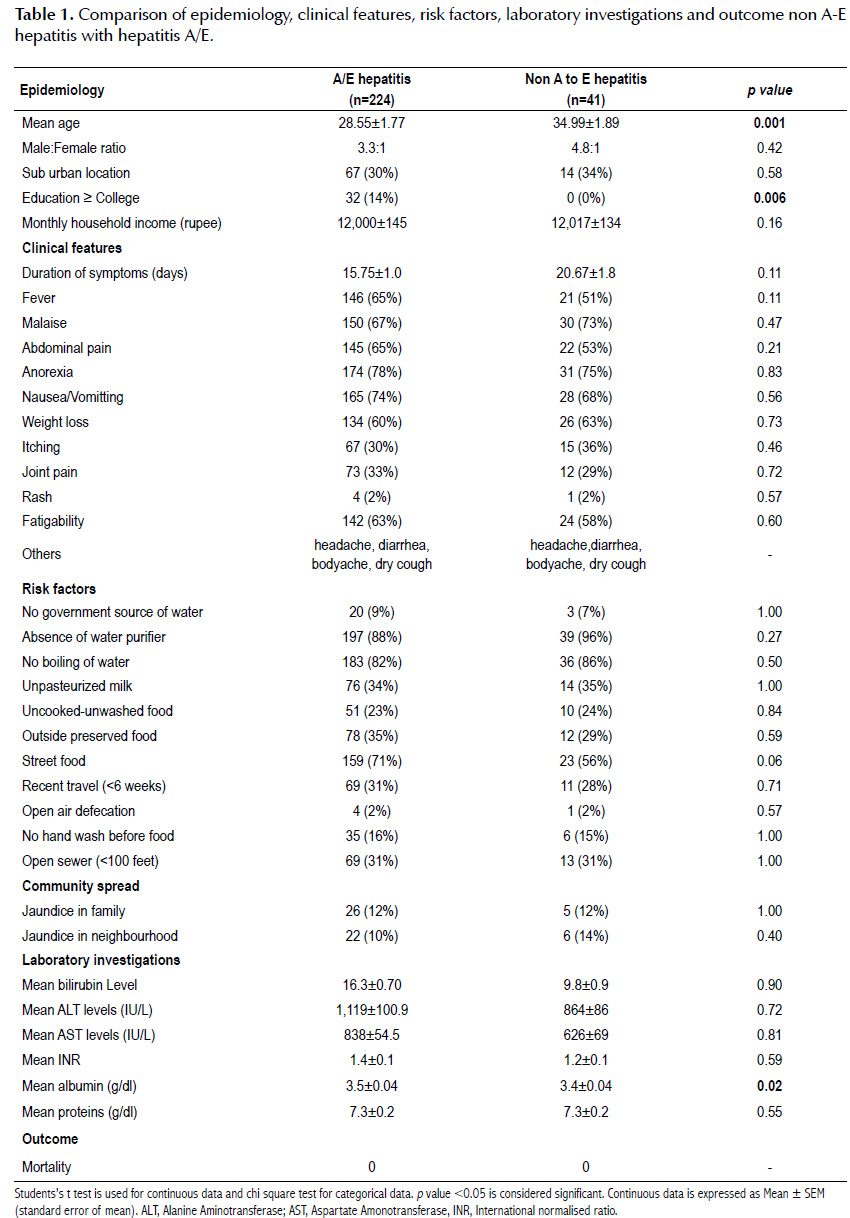
A total of 265 patients were admitted. Of these 265 patients, 41 patients (15.4%) were non A to E hepatitis while 224 patients had either hepatitis A or hepatitis E. The difference in epidemiology between these patients is shown in Table 1. Patients with non A to E hepatitis had statistically higher age of presentation as compared to A or E hepatitis. However, there was no statistical difference between the two groups in terms of gender distribution, monthly family income or location of their residence (Suburban versus Urban). It was found in our study that proportion of patients with education below graduation was significantly higher in non A to E group. The median SEC class for hepatitis A and E patients was A2 while for patients with non A to E hepatitis was A3.
Clinical features
There was no difference in clinical features between non A to E hepatitis patients and hepatitis A/E patients. Duration of symptoms at presentation and symptoms were similar between the two groups. Both the group patients had symptoms of anorexia, malaise and nausea/vomiting as most common symptoms. Other symptoms were fever, abdominal pain, weight loss, fatigability, itching, rash, joint pains, head ache, body ache, diarrhoea and dry cough.
Students’s t test is used for continuous data and chi square test for categorical data. p value <0.05 is considered significant. Continuous data is expressed as Mean ± SEM (standard error of mean). ALT, Alanine Aminotransferase; AST, Aspartate Amonotransferase, INR, International normalised ratio.
Risk factors
There was no difference in the risk factors causing the hepatitis between the two groups. All risk factors, non government water source, absence of water purifier at home, no boiling of water before drinking, eating uncooked-unwashed food, preserved food or street food and presence of open sewer nearby (<100 feet) or open air defecation were similar between the two groups. Even the secondary attack rate was similar with history jaundice in family members or neighbours being non statistically different.
Laboratory investigations
The mean bilirubin, ALT and AST levels were lower in non A to E hepatitis group, though it did not reach statistical significance. Even the INR and proteins values were similar between the groups. Serum albumin values were statistically lower as compared to patients with hepatitis A/E.
Univariate and multivariate analyses
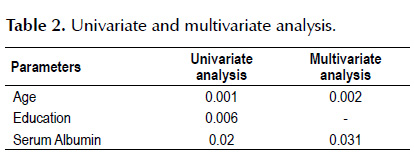
On univariate analysis the factors different in non A to E viral hepatitis group were higher age, lower education and lower serum albumin levels. On multivariate analyses however, only age and albumin levels turned out to be significant (Table 2).
DISCUSSION
Non A-E hepatitis is also known as hepatitis X. The virus causing this acute sporadic viral hepatitis is not known. Though initially suspected, Hepatitis G was not the cause of non A to E hepatitis (4). HGV, TTV, and SENV also do not seem to be responsible for the majority of sporadic acute non-(A-E) hepatitis cases (6). The cause of acute non-A–E viral hepatitis in the United States remains unknown (4). The heterogeneous nature of the demographic, clinical, and epidemiologic characteristics of this group suggests that there are multiple etiologic factors, some of which may not be viral (4,6,7).
In a study by Alter MJ et al. (4) the characteristics of patients in this group were distinctly different from those of patients with known types of viral hepatitis. The patients were older, had milder illness, were more likely to be hospitalized for their hepatitis independent of their age, and had few identifiable sources of disease. In a recent study contrary findings were seen; it is believed to lead to chronic hepatitis in 15% cases unlike hepatitis A and E and has severe acute presentation (6). In the present study also we found out that patients with non A-E hepatitis was seen in 15% cases and had higher age, lower albumin levels and non significantly lower bilirubin, ALT and AST levels. In a recent study by Delic et al. (9) the frequency of non-A-E AH was 7.6%. Almost no difference was found between sexes; it was developed in all age groups, with the highest incidence in the middle age (mean age was 38.32 +/- 15.3 years). It appeared equally throughout the whole year. The duration of incubation varied much ranging from 20 to 180 days (median 60 days). In study by Chu et al. (10), in acute non-A-E hepatitis, the sex ratio was 34:19, and ages ranged from 21 to 76 years (median 49), biochemical tests revealed albumin 3.6 (2.2-4.4) g/ dl, AST 714 (193-2311) U/l, ALT 896 (310-3,000) U/l, bilirubin 11.2 (0.9-36.3) mg/dl, and prothrombin time >1.1 (0-11.5) seconds. No patients reported parenteral exposures or household contact. Forty-five percent had severe hepatitis (i.e., albumin <3 g/dl, bilirubin >15 mg/dl or prothrombin time >3 sec), including 3% with fulminant hepatitis. This is in corroboration with our study showing transaminases in lower range. However, in our study it was found that there is no difference in the clinical presentation as not only the symptoms but also the risk factors responsible for causing this type of hepatitis was similar to usual hepatitis A and E. The distribution of virus as well as secondary attack rate is similar to hepatitis A and E. In study by Delic et al., out of risk factors, inoculation risk was predominant (before all, dental interventions), mostly involving urban population living in comfortable conditions. By clinical course, moderate and icteric forms were most common, mostly corresponding to acute hepatitis A.
The limitation of our study was that patients were not followed up for six months. In different studies the rate of chronicity has remained between 8 to 15 percent (7,9,10). The outcome is believed to be similar to chronic hepatitis B and even cases of cirrhosis have been reported. In study by Chu et al. it was concluded that clinical severity was similar to that of hepatitis C at least in hospitalized patients, but the rate of chronic evolution is much lower.
In conclusion, non-A-E hepatitis remains enigmatic and not fully understood. The clinical presentation of our cases, strongly suggested a viral disease with spontaneous resolution in all cases. Non-A-E hepatitis seems to involve more than one disease, perhaps with regional peculiarities, and a variable prognosis.
BIBLIOGRAPHIC REFERENCES
1. Shrivastava A. Hepatitis in India: Burden, Strategies and Plans. NCDC Newsletter. 2014;3(1):1-3. [ Links ]
2. Gupta A, Chawla Y. Changing Epidemiology of Hepatitis A infection. Indian J Med Res. 2008;128(1):7-9. [ Links ]
3. Subhash Chandra N, Sharma A, Roop Rai R, Malhotra B. Contribution of hepatitis E virus in acute sporadic hepatitis in North West India. Indian J Med Res. 2012;136(3):477-82. [ Links ]
4. Alter JM, Gallagher M, Morris TT, Moyer LA, Meeks EL, Krawczynski K, et al. Acute non-A–E hepatitis in the United States and the role of hepatitis G virus infection. entinel Counties Viral Hepatitis Study Team N Engl J Med. 1997;336(11):741-6, [ Links ]
5. Buti M, Jardi R, Rodríguez-Frias F, Quer J, Esteban R, Guardia J. Non-A, non-B, non-C, non-E acute hepatitis: does ¡t really exist? In: Nishioka K, Susuki H, Mishiro S, Oda T (eds.). Viral hepatitis and Liver Disease. Tokyo: Springer Veriag; 1994. p. 77-9. [ Links ]
6. Tassopoulos NC, Papatheodoridis GV, Delladetsima I, Hatzakis A. Clinicopathological features and natural history of acute sporadic non-(A-E) hepatitis. J Gastroenterol Hepatol. 2008;23(8):1208-15. [ Links ]
7. Rochling FA, Jones WF, Chau K, DuCharme L, Mimms LT, Moore B, et al. Acute sporadic non-A, non-B, non-C, non-D, non-D, non-E hepatitis. Hepatology. 1997;25(2):478-83. [ Links ]
8. The new SEC system [Internet]. Worli, Mumbai: Medical Research Users Council; 2011 [citado el 6 de febrero de 2017]. Disponible en: http://mruc.net/assets/frontend/images/download/NEW%20SEC%20System.pdf [ Links ]
9. Delić D, Mitrović N, Spurnić AR, Svirtlih NS, Babić JS. Epidemiological characteristics and clinical manifestations of acute non-A-E hepatitis. Vojnosanit Pregl. 2010;67(11):903-9.
10. Chu CM, Lin DY, Yeh CT, Sheen IS, Liaw YF. Epidemiological characteristics, risk factors, and clinical manifestations of acute non-A-E hepatitis. J Med Virol. 2001;65(2):296-300. [ Links ]
Correspondence:
Pathik Parikh
A 52 Shaligram 3, Prahladnagar, Ahmedabad, India, 380015.
E-mail: pathik269@gmail.com
Recibido: 31-7-2017
Aprobado: 26-10-2017