Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Gastroenterología del Perú
versión impresa ISSN 1022-5129
Rev. gastroenterol. Perú vol.38 no.4 Lima oct./dic. 2018
REPORTE DE CASO
Rendez-Vous laparoendoscopic after ERCP failure in patient with Billroth II gastrectomy
Laparoscopía por Rendez-Vous luego de falla de CPRE en un paciente con gastectomía Billroth II
Fernanda Kreve¹, Francisco S. Loss¹, Janaina Gatto¹, Jonas Takada2, Juliana Dantas³, Karina Inoue³, Alfredo L. Jacomo2, Everson L.A. Artifon2
1 Medical School Academic, Centro Universitário Fundação Assis Gurgacz. Cascavel, Brazil.
2 Departmentof Surgery, University of Sao Paulo. Sao Paulo, Brazil.
3 Medical School Academic, Universidade Federal do Paraná. Toledo, Brazil.
ABSTRACT
Endoscopic retrograde cholangiopancreatography (ERCP) is the treatment of choice in patients with choledocholithiasis. However, despite its high success rate, in some cases it is not successful, requiring alternative therapy. Billroth II partial gastrectomy is a condition associated with an important failure rate of ERCP. When endoscopic treatment fails, surgical exploration of the bile duct is the most common approach. However, the surgery is related to a greater complexity of execution and morbimortality. We describe the case of a patient with choledocholithiasis and Billroth II partial gastrectomy, submitted to the combined treatment called rendez-vous laparoendoscopic, after failure of ERCP, which unites in a single stage the endoscopic treatment of choledocholithiasis and laparoscopic removal of the gallbladder. We conclude that this therapeutic approach was effective, safe, with low cost and without complications.
Keywords: Gallstones; Cholangiopancreatography, endoscopic retrograde; Gastrectomy (source: MeSH NLM).
RESUMEN
La colangiopancreatografía endoscópica retrógrada (CPRE) es el tratamiento de elección en pacientes portadores de coledocolitiasis. Sin embargo, a pesar de su elevada tasa de éxito, en algunos casos no es exitosa, exigiendo terapia alternativa. La gastrectomía parcial con reconstrucción a Billroth II es una condición asociada a la importante tasa de fracaso de la CPRE. Cuando el tratamiento endoscópico falla, la exploración quirúrgica de la vía biliar es un enfoque más común. Sin embargo, la cirugía se relaciona con una mayor complejidad de ejecución y morbimortalidad. Describimos el caso de un paciente con coledocolitiasis y gastrectomía parcial con reconstrucción a Billroth II, sometido al tratamiento combinado denominado rendez-vous laparoendoscópico tras fallo de la CPRE, que une en una sola etapa el tratamiento endoscópico de la coledocolitiasis y la retirada laparoscópica de la vesícula biliar. Llegamos a la conclusión de que este enfoque terapéutico fue eficaz, seguro, de bajo costo y sin complicaciones.
Palabras clave: Cálculos biliares; Colangiopancreatografía retrógrada endoscópica; Gastrectomía (fuente: DeCS BIREME).
INTRODUCTION
Retrograde endoscopic cholangiopancreatography (ERCP) is the treatment of choice for choledocholithiasis resolution, with success rates reaching 90%. However, it becomes a difficult procedure in patients who have altered anatomy, requiring an alternative therapy for the gallstones extraction of the the main bile duct. We describe the case of a patient with previous Bilroth II partial gastrectomy, cholelithiasis and associated choledocholithiasis who, after ERCP failure, underwent cholecystectomy and bile duct endoscopic treatment in the same operative procedure using the Rendez-Vous technique guided by videolaparoscopy.
CLINICAL CASE
Male patient, 63 years old, pain in upper abdomen for 1 week and obstructive jaundice. Previous history of Billroth II partial gastrectomy because a gastric ulcer 20 years ago. No comorbidities. He underwent an ultrasound examination that showed cholelithiasis and choledocholithiasis. In view of the condition, the patient underwent endoscopic retrograde cholangiopancreatography (ERCP).
The ERCP was not successful in the resolution of choledocholithiasis due to anatomical distortions resulting from previous gastrectomy. During the procedure, after recognition of the afferent loop and introduction of the duodenoscope to the region of the major duodenal papilla, there was no success in extrahepatic bile duct cannulation. The patient’s previous gastrectomy displaced the papilla to an inverse position from the usual, making impossible its correctly visualization and cannulation. Then, laparoscopic removal of the gallbladder and the choledocholithiasis endoscopic treatment were proposed at the same surgical time.
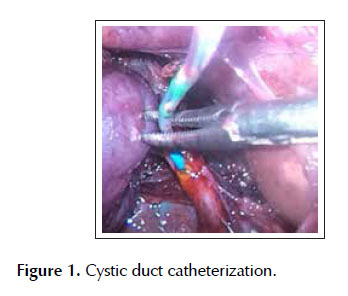
In surgery, we started with standardized laparoscopic gallbladder dissection. The calot triangle was dissected, the cystic artery individualized, ligated and sectioned. Subsequently, the cystic duct was identified and ligated into its proximal portion. We performed a small distal opening that allowed the catheterization of the catheter through a 0.035-inch guidewire (Jagwire, Boston Scientific Inc., Watertown Massachusetts, United States) coupled to a cholangiography catheter (Microknife ™ XL; Boston Scientific) (Figure 1).
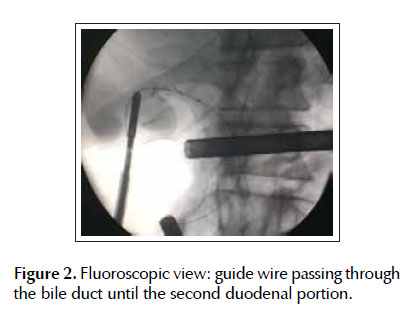
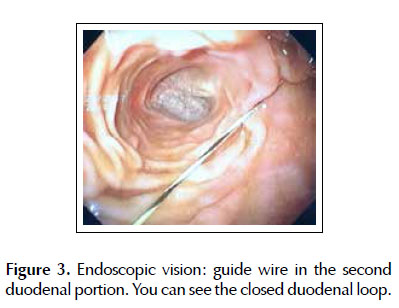
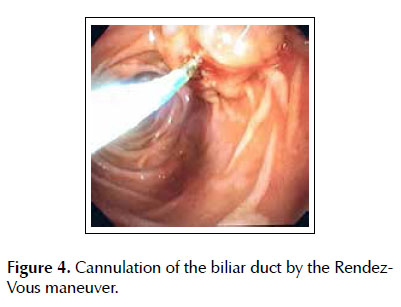
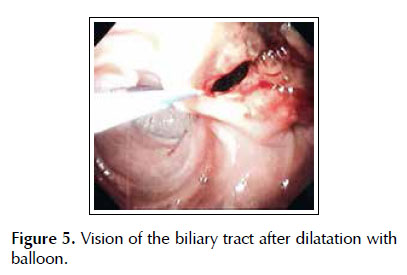
Under fluoroscopic and transcystic vision, the guide wire progressed anteriorly through the common bile duct and duodenal papilla to the second duodenal portion (Figures 2 and 3). From that moment, a frontal view endoscope was introduced by the afferent loop until the second duodenal portion, where the guidewire was recovered (Rendez-Vous maneuver) with the help of a polypectomy loop and used to guide the retrograde cannulation of the bile duct (Figure 4). After extensive papillotomy and balloon dilatation of the bile duct, we performed the big gallstone extraction of the common bile duct (Figure 5). We concluded with laparoscopic extraction of the gallbladder.
The surgical procedure lasted approximately 130 minutes and occurred without intercurrences. The patient had a good evolution, without complications, being discharged after 2 days of hospitalization, with ambulatory accompaniment.
DISCUSSION
Due to its effectiveness, endoscopic retrograde cholangiopancreatography (ERCP) is considered the treatment of choice in patients presenting with choledocholithiasis. It allows the removal of gallstones from the common bile duct not only in the preoperative period of cholecystectomy, but also during or after surgery, with success rates exceeding 90% (1). However, when necessary in patients with altered anatomy, as in the present case after a Billroth II partial gastrectomy (BII), it becomes a challenging procedure and with lower success rates.
In this case, the first problem to be solved was recognize the afferent loop at the site of the gastrojejunostomy. After accessing the afferent loop, should be progressed to the greater duodenal papilla and perform the therapy in reverse orientation to standard ERCP (2,3). Another complicating factor is the increased risk of perforation during ERCP in patients with altered anatomy (0.1% - 0.6% in patients with normal anatomy versus 10.2% in patients with Billroth II partial gastrectomy). The introduction of balloon-assisted enteroscopy in recent years has increased the success rate of duodenal stump intubation when performing ERCP in patients with BII reconstruction. However, the small operative channel of the enteroscope (2.8 mm), the frontal view, the lack of the elevator and the absence of adequate catheters for ERCP are limitations that may reduce its therapeutic efficacy when performing ERCP in altered anatomy (2).
When ERCP fails to treat choledocholithiasis, laparoscopic surgical exploration of the bile duct has been the choice because it presents lower rates of complications when compared to open surgery (6). To do this, it requires extensive experience in advanced laparoscopic procedures, involves unusual radiological and endoscopic knowledge to many surgeons, which increases surgical time and complication rate (7,8). Thus, given the technical difficulties, the long and difficult learning curve and the need for technical resources (high quality fluoroscopy and choledochoscope) not available in many operating rooms, laparoscopic exploration of the bile duct is technically restricted to a few medical centers (9).
ERCP is easy to perform and widely available in the hospital setting. When combined with laparoscopic exploration of the bile duct, it has the advantage that can be applied independently of the bile duct diameter, size or number of gallstones (10). Thus, in 1993, Deslandres et al., developed the combined laparoendoscopic treatment. The treatment described during videolaparoscopic cholecystectomy consists of the intraoperative realization of ERCP after the anterograde (transcystic) insertion of a guidewire to reach the greater duodenal papilla and to make its cannulation guided, easier and safer, allowing the gallstones withdrawal from the common bile duct with balloon catheter or basket (11,12).
The main advantage in performing intraoperative ERCP using the Rendez-Vous technique is to allow selective access of the bile duct, avoiding excessive manipulation of the major duodenal papilla and unintentional cannulation of the pancreatic duct. Consequently, it results in a lower chance of pancreatitis when compared to conventional ERCP (13). In addition, there is a reduction in surgical time through the anatomical passage of the guide wire through transcystic access, a decrease in hospital stay and lower costs (14,15). Therefore, laparoendoscopic Rendez-Vous is an alternative to be considered as a rescue in ERCP failure in patients with GII before attempting to avoid surgical exploration.
Probably the main obstacle to the laparoendoscopic Rendez-Vous technique is the need to coordinate and synchronize surgical and endoscopy teams, who must work together. For this, the endoscopic team must be previously familiar with the surgery that the patient will be submitted to and be ready to enter the field once the guide wire reaches the duodenum (15). Williams and Vellacot (16) state that, in an ideal scenario, it would be more advantageous for the surgeon to be able to perform ERCP. Otherwise, it would require a longer time related to the logistics organization of the procedure, as reported in previous studies (17).
CONCLUSION
The proper management of choledocholithiasis in the biliary tract with altered anatomy is closely related to the technical skills of medical teams. In laparoendoscopic treatment in a single stage, some of the advantages over the two-step method include: reduction of cannulation time and the complications associated with endoscopic manipulation of the major duodenal papilla, and lower risk of intestinal perforation, in addition to low cost and short hospitalization. Therefore, it is a safe and effective alternative in the treatment of choledocholithiasis in patients with altered anatomy, as in the previous Bilroth II gastrectomy.
BIBLIOGRAPHIC REFERENCES
1. Kumar S, Sherman S, Hawes RH, Lehman GA. Success and yield of second attempt ERCP. Gastrointest Endosc. 1995;41(5):445-7. [ Links ]
2. Ciçek B, Parlak E, Dişibeyaz S, Koksal AS, Sahin B. Endoscopic retrograde cholangiopancreatography in patients with Billroth II gastroenterostomy. J Gastroenterol Hepatol. 2007;22(8):1210-3.
3. Costamagna G, Mutignani M, Perri V, Gabrielli A, Locicero P, Crucitti F. Diagnostic and therapeutic ERCP in patients with Billroth II gastrectomy. Acta Gastroenterol Belg. 1994;57(2):155-62. [ Links ]
4. Kim MH, Lee SK, Lee MH, Myung SJ, Yoo BM, Seo DW, et al. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: a comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy. 1997;29(2):82-5. [ Links ]
5. Costamagna G, Loperfido S, Familiari P. Endoscopic retrograde cholangiopancreatography (ERCP) after Billroth II reconstruction [Internet]. UpToDate; c2019 [citado el 21 de junio de 2019]. Disponible en: https://www.uptodate.com/contents/endoscopic-retrograde-cholangiopancreatographyercp-after-billroth-ii-reconstruction [ Links ]
6. Grubnik VV, Tkachenko AI, Ilyashenko VV, Vorotyntseva KO. Laparoscopic common bile duct exploration versus open surgery: comparative prospective randomized trial. Surg Endosc. 2012;26(8):2165-71. [ Links ]
7. Ghazal AH, Sorour MA, El-Riwini M, El-Bahrawy H. Singlestep treatment of gall bladder and bile duct stones: a combined endoscopic-laparoscopic technique. Int J Surg. 2009;7(4):338-46. [ Links ]
8. Tinoco R, Tinoco A, El-Kadre L, Peres L, Sueth D. Laparoscopic common bile duct exploration. Ann Surg. 2008;247(4):674-9. [ Links ]
9. Flowers JL. ERCP versus laparoscopic surgery: the contest over common bile duct stones. Endoscopy. 1996;28(5):438-40. [ Links ]
10. Sherman S, Hawes RH, Rathgaber SW, Uzer MF, Smith MT, Khusro QE, et al. Post-ERCP pancreatitis: randomized, prospective study comparing a low- and high-osmolality contrast agent. Gastrointest Endosc. 1994;40(4):422-7. [ Links ]
11. Deslandres E, Gagner M, Pomp A, Rheault M, Leduc R, Clermont R, et al. Intraoperative endoscopic sphincterotomy for common bile duct stones during laparoscopic cholecystectomy. Gastrointest Endosc. 1993;39(1):54-8. [ Links ]
12. La Grecca G, Barbagallo F, Di Blasi M, Chisari A, Lombardo R, Bonaccorso R, et al. Laparo-endoscopic ‘‘Rendez-Vous’’ to treat cholecysto-choledocholithiasis: Effective, safe and simplifies the endoscopist’s work. World J Gastroenterol. 2008;14(18):2844-50.
13. Nathanson LK, O’Rourke NA, Martin IJ, Fielding GA, Cowen AE, Roberts RK, et al. Postoperative ERCP versus laparoscopic choledochotomy for clearance of selected bile duct calculi: a randomized trial. Ann Surg. 2005;242(2):188-92.
14. Cox MR, Wilson TG, Toouli J. Peroperative endoscopic sphincterotomy during laparoscopic cholecystectomy for choledocholithiasis. Br J Surg. 1995;82(2):257-9. [ Links ]
15. Rábago LR, Vicente C, Soler F, Delgado M, Moral I, Guerra I, et al. Two-stage treatment with preoperative endoscopic retrograde cholangiopancreatography (ERCP) compared with single-stage treatment with intraoperative ERCP for patients with symptomatic cholelithiasis with possible choledocholithiasis. Endoscopy. 2006;38(8):779-86. [ Links ]
16. Williams GL, Vellacot KD. Selective operative cholangiography and perioperative endoscopic retrograde cholangiopancreatography (ERCP) during laproscopic cholecystectomy. A viable option for choledocholithiasis. Surg Endosc. 2002;16(3):465-7. [ Links ]
17. Montori A, Miscusi G, Masoni L, Gasparrini M, Pietropaolo V, Montori J, et al. Endoscopic and surgical integration in the approach to biliary tract disease. J Clin Gastroenterol. 1999;28(3):198-201. [ Links ]
Correspondence:
Everson L.A. Artifon
Departmentof Surgery, University of Sao Paulo. Sao Paulo, Brazil.
E-mail: eartifon@hotmail.com
Recibido: 16-4-18
Aprobado: 17-12-18