Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de Gastroenterología del Perú
Print version ISSN 1022-5129
Rev. gastroenterol. Perú vol.39 no.4 Lima Oct./Dec. 2019
REPORTE DE CASO
Esophageal intramural pseudodiverticulosis in a patient with food bolus impaction
Pseudodiverticulosis intramural esofágica en un paciente con impactación de bolo alimentario
Jean Félix Piñerúa-Gonsálvez1,2, Rosanna del Carmen Zambrano-Infantino1,3, Mariseli Sulbaran1
1. Department of Gastroenterology, Hospital Militar "Dr. Carlos Arvelo". Caracas, Venezuela.
2. Hospital de Clínicas Caracas. Caracas, Venezuela.
3. Policlínica Metropolitana. Caracas, Venezuela.
ABSTRACT
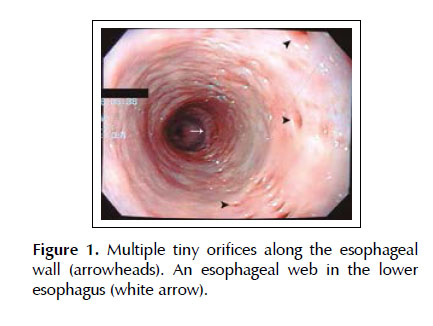
Esophageal intramural pseudodiverticulosis is an uncommon esophageal benign disease. The typical finding during endoscopy is the presence of numerous pinhead-sized outpouchings along the esophageal wall. We reported a case of food bolus impaction secondary to esophageal intramural pseudodiverticulosis. A 67-year-old man presented with sudden-onset dysphagia. Multiple tiny orifices were revealed during upper endoscopy. In addition, there were an impacted food bolus and an esophageal web. The patient was treated with balloon dilatation and proton pump inhibitors. As a result the symptoms disappeared completely. Esophageal intramural pseudodiverticulosis is a rare cause of food bolus impaction and its treatment is directed towards the underlying associated conditions as well as the resolution of complications.
Keywords: Dysphagia; Esophageal diseases; Gastric balloon (source: MeSH NLM).
RESUMEN
La pseudodiverticulosis intramural esofágica es una enfermedad benigna del esófago poco común. El hallazgo típico durante la endoscopia es la presencia de numerosos sáculos del tamaño de una cabeza de alfiler a lo largo de la pared esofágica. Reportamos un caso de impactación de bolo alimentario secundario a pseudodiverticulosis esofágica intramural. Un hombre de 67 años presentó disfagia de aparición repentina. Se encontraron múltiples orificios pequeños en la endoscopia superior. Además, hubo un bolo alimentario impactado y una red esofágica. El paciente fue tratado con dilatación con balón e inhibidores de la bomba de protones. Como resultado, los síntomas desaparecieron por completo. La pseudodiverticulosis intramural esofágica es una causa rara de impactación del bolo alimentario y su tratamiento se dirige a las condiciones asociadas subyacentes, así como a la resolución de complicaciones.
Palabras clave: Disfagia; Enfermedades del esófago; Balón gástrico (fuente: DeCS BIREME).
INTRODUCTION
Esophageal intramural pseudodiverticulosis (EIPD) is an uncommon esophageal benign disease whose etiology is still unclear. Clinical features include dysphagia, chest pain, vomiting, weight loss and upper gastrointestinal bleeding (1,2). This rare disease has been associated with several underlying conditions, such as diabetes mellitus (DM), gastroesophageal reflux disease, HIV infection, eosinophilic esophagitis, esophageal candidiasis and esophageal carcinoma (3-5). This article aimed to report a case of food impaction secondary to EIPD.
CASE REPORT
A 67-year-old man presented with sudden-onset dysphagia and chest tightness while he was having steak. The patient had a medical history of DM treated with metformin/saxagliptin and without complications. He smoked 15 cigarettes per day. There were no remarkable findings in the physical examination. Electrocardiogram and routine analytical tests were within normal limits. Upper endoscopy was performed five hours after the onset of symptoms, revealing multiple lines of tiny diverticular orifices in the middle and lower esophagus (Figure 1). In addition, there was an impacted food bolus at 4 cm above the gastroesophageal junction, which was extracted en bloc by using a polypectomy snare. Afterwards, a esophageal web was found, therefore, a through-the-scope balloon dilation was performed by filling up the balloon from 15 mm to 18 mm. Biopsies were taken from the upper, lower esophagus and the esophageal web. Histopathology reported basal cell hyperplasia, elongation of papillae and eosinophilic infiltration <15 cells per high-power field, without evidence of malignancy. Esophageal manometry did not reveal motility disorders. The patient was treated with omeprazole for three months. The patient did not present recurrence of the symptoms for a 12-month follow-up period.
The patient consent was obtained for publication of the case.
DISCUSSION
EIPD was first reported by Mendl et al. in a patient who had presented with dysphagia and chest pain and the barium swallow showed intramural diverticula (6). The pathogenesis is still unclear. Histologically, EIPD is characterized by dilated excretory ducts of submucosal glands, bordered by an inflammatory infiltrate. Thus, it is thought that a chronic inflammatory condition blocks excretory ducts of submucosal glands which leads to the formation of pseudo diverticula (1,3,7-9).
This condition is more frequent among patients in their fifties and sixties (7). Nevertheless, it has been reported some cases in younger patients (10). Usually, symptoms include dysphagia, which can be either intermittent or progressive, chest tightness, odynophagia, vomiting, chest pain, weight loss and rarely hematemesis and melena (1). In the present case, the symptoms were dysphagia and chest tightness. Our patient had a past history of diabetes mellitus and histological findings compatible with reflux esophagitis, which are underlying conditions that have been associated to EIPD. Others include HIV infection, eosinophilic esophagitis, esophageal candidiasis and esophageal carcinoma (3-5).
Diagnosis of EIPD is established by either barium esophagogram or upper endoscopy. The typical finding during upper endoscopy is the presence of numerous pinhead-sized outpouchings along the esophageal wall (3). In the current case, multiple tiny orifices in the middle and lower esophagus were revealed during endoscopy. In addition, an esophageal web was found and was treated by balloon dilation. Approximately half of patients present with strictures at the moment of diagnosis and represent the most common complication (11). Strictures are often treated by using bougienage (with excellent improvement of the dysphagia) and balloon dilation. However, in cases of extensive and refractory strictures, esophageal resection should be considered. The management of EIPD includes treatment of the underlying conditions as well as the resolution of complications (strictures, perforation, broncho-esophageal fistula and gastrointestinal bleeding) (12,13). Our patient did not have recurrence of the symptoms during the follow-up period.
As shown above, we reported a case of food bolus impaction secondary to EIPD, which was successfully treated by balloon dilation and omeprazole.
Author contributions: JF Piñerúa-Gonsálvez and RC Zambrano-Infantino drafted the manuscript. M Sulbaran reviewed and approved final draft of the manuscript. JF Piñerúa-Gonsálvez is the article guarantor.
Financial disclosure: None to report.
Citar como: Piñerúa-Gonsálvez JF, Zambrano-Infantino RC, Sulbaran M. Esophageal intramural pseudodiverticulosis in a patient with food bolus impaction. Rev Gastroenterol Peru. 2019;39(4):362-3
REFERENCES
1. Siba Y, Gorantla S, Gupta A, Lung E, Culpepper-Morgan J. Esophageal intramural pseudodiverticulosis, a rare cause of food impaction: case report and review of the literature. Gastroenterol Rep (Oxf). 2015;3(2):175-8. [ Links ]
2. Yamamoto N, Nakamura M, Tachibana S, Konno H, Nakamura S, Nishino N. Esophageal intramural pseudodiverticulosis with Mallory-Weiss syndrome: report of a case. Surg Today. 2002;32(6):519-22. [ Links ]
3. Sinha N, Mikityanskiy Y, Mularz S, Trillo J. Esophageal intramural pseudodiverticulosis. Gastrointest Endosc. 2018;88(4):764-5. [ Links ]
4. Plavsic BM, Chen MY, Gelfand DW, Drnovsek VH, Williams JP 3rd, Kogutt MS, et al. Intramural pseudodiverticulosis of the esophagus detected on barium esophagograms: increased prevalence in patients with esophageal carcinoma. AJR Am J Roentgenol. 1995;165(6):1381-5. [ Links ]
5. Szczesna M, Gatarek J, Orlowski T. Esophageal intramural pseudodiverticulosis as a diagnostic and therapeutic problem. Kardiochir Torakochirurgia Pol. 2016;13(3):265-8. [ Links ]
6. Mendl K, McKay JM, Tanner CH. Intramural Diverticulosis of the Oesophagus and Rokitansky-Aschoff Sinuses in the Gall- bladder. Brit J Radiol. 1960;33(392):496-501. [ Links ]
7. Chon YE, Hwang S, Jung KS, Lee HJ, Lee SG, Shin SK, et al. A case of esophageal intramural pseudodiverticulosis. Gut Liver. 2011;5(1):93-5. [ Links ]
8. Wightman AJ, Wright EA. Intramural oesophageal diverticulosis: a correlation of radiological and pathological findings. Br J Radiol. 1974;47(560):496-8. [ Links ]
9. Medeiros LJ, Doos WG, Balogh K. Esophageal intramural pseudodiverticulosis: a report of two cases with analysis of similar, less extensive changes in "normal" autopsy esophagi. Hum Pathol. 1988;19(8):928-31. [ Links ]
10. Peters ME, Crummy AB, Wojtowycz MM, Toussaint JB. Intramural esophageal pseudodiverticulosis: a report in a child with a 16-year follow up. Pediatr Radiol. 1983;13(4):229-30. [ Links ]
11. Halm U, Lamberts R, Knigge I, Mossner J, Zachaus M. Esophageal intramural pseudodiverticulosis: endoscopic diagnosis and therapy. Dis Esophagus. 2014;27(3):230-4. [ Links ]
12. Struyve M, Langmans C, Robaeys G. Pneumomediastinum as a complication of esophageal intramural pseudodiverticulosis. Acta Gastroenterol Belg. 2018;81(3):433-5. [ Links ]
13. Tyberg A, Jodorkovsky D. A Treatment option for esophageal intramural pseudodiverticulosis. ACG Case Rep J. 2014;1(3):134-6. [ Links ]
Correspondence:
Jean Félix Piñerúa-Gonsálvez
Department of Gastroenterology. Hospital Militar "Dr. Carlos Arvelo", Caracas, Venezuela.
E-mail: jeanfelixmedicina@hotmail.com