INTRODUCTION
Both hepatitis A virus (HAV) and hepatitis E virus (HEV) are leading causes of acute viral hepatitis in developing countries due to poor sanitary conditions. These viruses spread by the fecal-oral route or through contaminated water and food. The prevalence of HAV and HEV coinfection has been reported 1-3, however, there are only few studies about its clinical presentation 4,5.
Although these are self-limited infections and present with mild symptoms, extrahepatic manifestations are reported in both of them, mostly in pediatric patients. These include pleural effusion, gallbladder abnormalities ascites, glomerulonephritis, cryoglobulinemia, thrombocytopenia, agranulocytosis, aplastic anemia, pancreatitis, among others 5-9. We report the first case - to the best of our knowledge - of a patient with three of these complications, in the context of a HAV and HEV dual infection.
CASE REPORT
A 32-year-old woman was admitted to the clinic with two days history of intense epigastric pain, nausea, vomiting and dark urine. There was no significant medical history. She had traveled to Colombia two weeks before admission. She was afebrile with normal vital signs. On physical examination, she was icteric, had epigastric tenderness, positive Murphy sign and liver was not palpable.
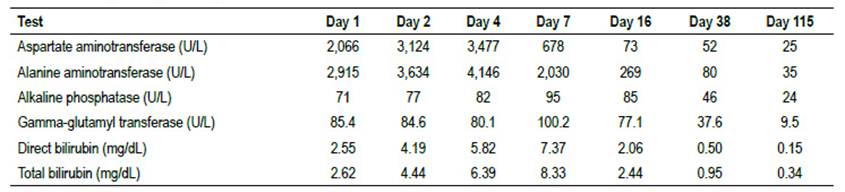
Laboratory examination yielded the following: hemoglobin: 14.4 g/dL, hematocrit: 41.8%, white blood cell count: 3,100 cells/mm3, platelet count: 200,000 cells/mm3, amylase: 73 U/L, total bilirubin: 2.62 mg/dL, direct bilirubin: 2.55 mg/dL, aspartate aminotransferase: 2,066 U/L, alanine aminotransferase: 2,915 U/L, gamma-glutamyl transferase: 85.4 U/L, alkaline phosphatase: 71 U/L and c-reactive protein: 6.2 mg/L, HAV IgM was positive; INR, electrolytes, albumin and glucose were in the normal ranges. An abdominal ultrasound showed a thickened (9 mm) not calculous gallbladder (Figure 1A). The diagnosis of hepatitis A with acute reactive cholecystitis was established.

Figure 1: A) Thickening of gallbladder wall (9 mm) on the day of admission. B) Free liquid in the hepatorenal recess and right paracolic recess. C) Right pleural effusion on the 4th day of admission.
On the 4th day of admission, the patient persisted with abdominal pain and presented abdominal distention. A second ultrasound revealed ascites with perihepatic and perisplenic fluid (Figure 1B) and right pleural effusion (Figure 1C). IgM for Hepatitis E virus was positive. Serological markers for Hepatitis B virus and Hepatitis C virus were interpreted as negative. She was managed with supportive parenteral fluids and eventually a low-fat diet, and clinical improvement was seen over the next days. Hepatic enzyme levels raised initially, but gradually returned to normal values within a four-month follow-up (Table 1), in which the patient continued to do well, showing no sonographic signs of extrahepatic manifestations.
DISCUSSION
Hepatitis A is generally an acute, self-limiting liver infection transmitted through the fecal-oral route by a positive-strand RNA virus, the hepatitis A virus (HAV), which causes 10 million infections worldwide each year 10. Serological and molecular studies have shown that hepatitis E virus (HEV) is globally distributed and is the leading cause of enterically transmitted viral hepatitis illness worldwide. It is estimated that two billion people worldwide are infected with HEV every year, with 14 million symptomatic cases and 300,000 deaths 11. Considering the similar epidemiological profile of both viruses, it is unsurprising that a dual infection is not uncommon. A cross-sectional study conducted in India reported that the prevalence of both HAV and HEV in patients with acute viral hepatitis was 11.5% 1. Another study in Cuba demonstrated that such coinfection is up to 12.8% of cases of acute viral hepatitis 3, unfortunately, there is a lack of data regarding the clinical manifestations and natural history of this under-reported condition.
Although both infections usually present with clinical manifestations that are mainly limited to liver inflammation; both viruses, especially HAV, may present with complications, such as cholecystitis, pleural effusion and ascites. The prevalence of these complications is not as unusual as previously thought. In a recent retrospective study, findings were collected from ultrasound examinations and laboratory data from 43 adult patients with HAV infection who were admitted to the "Hadassah-Hebrew University Medical Center" between 2004-2016. Ascites was noted in 8 patients, a thickened gallbladder wall was observed in 14, pericholecystic fluid in 8 and biliary sludge in 4 6.
Ascites in liver diseases may occur as a result of venous and lymphatic obstruction or hypoalbuminemia; as albumin levels were in the normal range in our patient, an increase in venous or lymphatic pressure due to the compression of hepatic sinusoids may explain the occurrence of ascites in this case 12.
Pleural effusion may be secondary to ascites due to fluid transport through the diaphragmatic lymphatics or direct passage through a diaphragmatic defect 12, or due to deposit of immune complexes 7,8. Gallbladder abnormalities are also reported, being gallbladder thickening the most common. One possible mechanism is that it occurs when hepatocyte injury at the onset of HAV infection causes a temporary decrease in bile production and excretion. A second hypothesis is that HAV contained in bile juice causes a direct injury to the gallbladder mucosal and muscular layers. Another hypothesis is that hepatocyte necrosis causes inflammatory reaction in the tissues surrounding the liver, including the gallbladder wall 13, and possibly the pleura.
Despite of not being uncommon, since three of the complications were seen in the same patient at the same time, we suggest that the HAV and HEV co-infection must have played a synergic role causing inflammation in tissues surrounding the liver, possibly due to deposit of immune complexes that finally led to this unusual presentation.
In conclusion, our case represents a unique manifestation of a dual infection with Hepatitis A and Hepatitis E. The goal with this report is to emphasize the possibility of a coinfection of this kind, in the context of an immunocompetent patient who presents the clinical findings mentioned above.