INTRODUCTION
Eosinophilic gastroenteritis is a rare condition characterized by abnormal eosinophil infiltration of the gastrointestinal wall 1. Symptoms depends on the site involved and the depth of the compromise, typical clinical manifestations include abdominal pain, vomiting, diarrhea, dysphagia, microcytic anemia and hypoproteinemia. Previous history of atopy is common (50%-75%). High eosinophil count in peripheral blood and a count may be present in peripheral blood of 30 or more eosinophils on biopsies of patients without diagnosis of parasitic infections, autoimmune diseases, ulcerative colitis, allergies, malignancies or transplantation immune can be found 2. This article reviews the case of a patient with gastric outlet obstruction as manifestation of eosinophilic gastroenteritis, which was only diagnosed after partial gastrectomy. The importance our case report highlights a rare entity causing gastric outlet obstruction because of primary eosinophilic infiltration in the antrum.
CASE REPORT
A 60-year-old man with no relevant medical history presented to the urgent care with a chief complain of upper abdominal pain, vomiting and a 4 kg weight loss for 2 weeks. On physical examination, blood pressure was 113/82 mmHg, heart rate 76 bpm, respiratory rate 18 rpm, no fever. The abdomen was lightly distended without palpable masses. Laboratory studies showed blood count cell count in 13,300, eosinophil count of 21.1% (2,800 cells). Normal renal and liver tests, amylase of 294 U/L, normal stool sample, electrolites and a negative HIV test. Computed tomography showed thickening of the antrum, pylorus and superior duodenum, without evidence of defined masses or fluid collections (Figure 1). Gastrointestinal endoscopy showed loss of distensibility and thickening of pyloric folds, as well as thickened superior duodenal mucosa, biopsies showed reactive gastropathy with fibrosis in the lamina propria, eosinophil infiltrate. The duodenal mucosa was normal. Gastric Endoscopic Ultrasonography (EUS) showed a hypoechoic thickening of 16 mm within the fourth echolayer, with hypoechoic perigastric round lesion of about 6.4 mm (Figure 2).
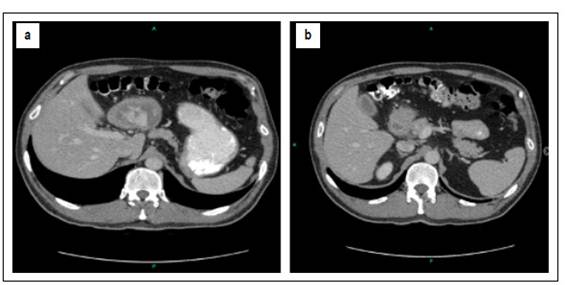
Figure 1 (a) Axial abdominal computed tomography with contrast shows thickening of the walls of the stomach concerning gastric outlet obstruction, (b) the pylorus and duodenum.
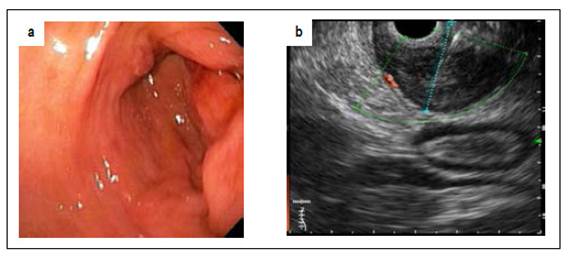
Figure 2 a) Endoscopic image of the antrum edema and erythema with luminal stenosis. b) Endoscopic Ultrasonography findings:Hypoechoic homogeneous thickening of 16 mm within the deep wall layers, up to the muscular layer.
Symptoms of gastric obstruction persisted so, a possible malignancy was suspected. He was taken to partial gastrectomy with Roux-en-Y reconstruction, lymph node removal and cholecystectomy. Few free peritoneal fluid was found, frozen section biopsy of the lymph nodes was reported as negative. Pathology findings infiltrative mass conditioning serous retraction, extending from the Antrum into the Pylorus and reached the superior duodenum. (Figure 3).
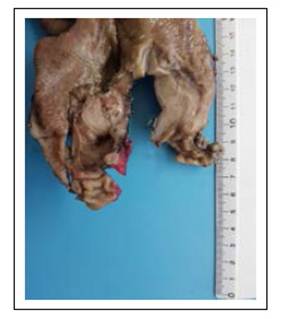
Figure 3 Macroscopy view of Antrum and the body gastric a depressed lesion with thickened folds, fibrous, irregular edges, light brown in color, of 5x4x3 cm.
Microscopic sections shoed a dense eosinophilic inflammatory infiltrate with associated abscesses and granulomas that compromised the entire wall depth. Hyperplasia of the muscular layer with extensive inflammatory eosinophilic infiltration dissecting the muscle fibers, reaching the serous layer and compromising blood vessel walls. Neural plexus was also compromised. The distal section edge of the surgical piece and the duodenal edge were also affected. Lymph nodes showed sinusoidal hyperplasia with histiocytic and eosinophilic infiltration (Figure 4), immunohistochemistry for S100 and CD1 were negative. The diagnosis was eosinophilic gastritis and gastroenteritis as final diagnosis.
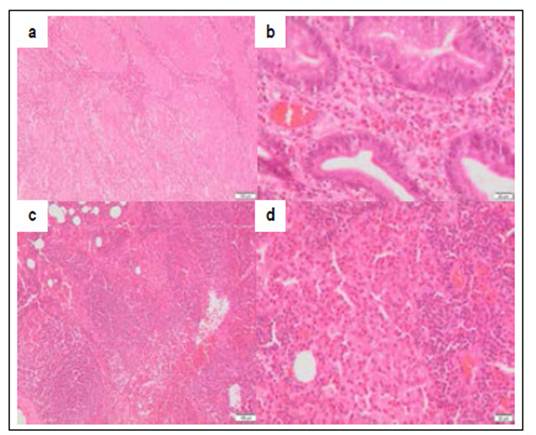
Figure 4 Biopsy gastric showing areas of increased eosinophilic infiltration. a) Muscularis mucosae. b) Antral and pyloric mucosa showed dense eosinophilic infiltration that penetrates the glandular epithelium. c) Muscular fibers of the muscularis mucosae. d) Close-up of muscularis mucosae.
After surgery, showed WBC 8,400, eosinophils 200 cells corresponding to 2.4%. Immunoglobulin E 31.5 U/ mL. Subsequently, the patient was initiated Prednisone 40 mg for 8 weeks, continuing with 5mg weekly. The patient was discharged after 10 days of clinical improvement. At 8 weeks after discharge, blood test with eosinophil count of 0% and at 12 weeks 0.9%. One year after surgery patient was doing well without any digestive symptom.
DISCUSSION
Eosinophils are a normal part of the mucosa of the gastrointestinal tract. They play an important role in the innate and adaptive immunity, specially the Th2 response. Eosinophil activation may cause cytokine release that conditions neural activation, muscular spasms and pain 3. Talley et al. in 1990 showed a common pattern of recurrent gastrointestinal symptoms in patients with eosinophilic infiltration identified in biopsies and peritoneal fluid 4. The etiology of eosinophilic gastroenteritis is unknown; prevalence of 2.5/100,000, higher incidence in men 1.2:1, in the second and fifth decades of life 4. Approximately 60% of patients have a history of atopy and 27% to family history 5.
Genta et al. 6 observed in a 370 patient study a mean eosinophil count of 8.2 +/- 6.3 per high power field. Talley et al. 7 in a randomized trial with 1001 patients with endoscopy, documented a mean eosinophil count of 11 per 5 high power fields in the stomach and 22 eosinophils per 5 high power fields in duodenum. Generally, the diagnosis of EG is at least 30 eosinophils per 5 high power fields are observed 2.
The clinical manifestations are chronic abdominal pain, vomiting and diarrhea, to weight loss and obstruction, in some cases, even chest pain has been observed as a symptom. Usually, when the muscular layer is compromised, obstructive manifestations, as seen in our patient 8,9. Histopathology findings the presence of eosinophils in the muscularis mucosae is almost always considered abnormal 10. Although histologic confirmation is necessary for diagnosis, it has its limitations. Eosinophilic infiltration can be distributed in deeper layers or in patches, therefore superficial biopsies can sometimes be normal 11,12. Gastrointestinal endoscopy, although unspecific, can also be useful, some findings include mucosal hyperemia, edema, small ulcers, nodularity or loss of normal vascular pattern 13. Diagnosis is defined by the presence of gastrointestinal symptoms, biopsies showed eosinophilic infiltration in the gastrointestinal tract and exclusion of secondary causes of eosinophilic infiltration.
There is no stablished standardized treatment for eosinophilic gastroenteritis due to the heterogeneous clinical manifestations and low prevalence. Corticosteroids play an important role in the EG; although a third of the patients show a temporary response to treatment and there is a risk of risk of further recurrence. We found no randomized control trial in the literature. Prednisone 20 to 40 mg daily, during 2 to 4 weeks or until remission is recomended. the duration of treatment remains controversial. Other interventions include elimination of dietary allergens such as wheat, milk, eggs, soy, nuts, seafood. H1 antagonists, antileukotriene medications and immunomodulatory drugs can be used as alternatives. Vedolizumab, a monoclonal antibody against  4
4  7 integrin showed recent promising results in 5 patients diagnosed with EG 14. In summary we report a case of gastric outlet obstruction due to EG in a middle age man who was treated with partial gastrectomy.
7 integrin showed recent promising results in 5 patients diagnosed with EG 14. In summary we report a case of gastric outlet obstruction due to EG in a middle age man who was treated with partial gastrectomy.
Informed consent was obtained for this case report.















