INTRODUCTION
The first cases of the acute respiratory distress syndrome due to SARS-CoV-2 appeared in the late 2019 in China 1,2. Despite being considered a less lethal virus than MERS-CoV and SARS-CoV, it is much more contagious, and given its rapid expansion the WHO declared this new disease as a pandemic on March 11, 2020 3,4.
This new disease generated a reorganization in the health system given that a great amount of resources was directed to the treatment of patients with COVID-19. In our hospital, these changes led to redefining priorities in patient care and reinforcing protective measures to reduce the risk of infection 5-7.
One of the activities that have been most affected within the new prioritized care scheme was the performance of endoscopies. Since endoscopy constitutes a potentially aerosol-generating procedure, it is considered to be at high risk of contagion of SARS- CoV-2 8-12. In this context, recommendations have been published by various scientific societies at an international level, giving guidelines for endoscopic practice based on the assessment of the procedure's urgency, stratification of the patient regarding the risk of SARS-CoV-2 infection, and the adequate use of personal protective equipment (PPE) 10-14.
In our Gastroenterology Department, in accordance with the recommendations of the Peruvian Society of Gastroenterology (15) and the hospital 16, all non-urgent endoscopic procedures were temporarily suspended, prioritizing the performance of urgent procedures, such as those indicated due to upper gastrointestinal bleeding (UGIB).
An endoscopy in the context of UGIB is considered an emergency procedure and should be performed as a priority within the first 24 hours after hemodynamic resuscitation, according to international and national recommendations 17,18. However, under the current situation, the time to endoscopy could be altered. Therefore, this study is conducted with the objective of evaluating the impact of the COVID-19 pandemic in the time to endoscopy in patients with UGIB.
The main objective was to compare the time since arrival at the hospital and the performance of the endoscopy between both groups. Secondary objectives were to compare the number of procedures performed, hospital stay and in-hospital mortality.
MATERIALS AND METHODS
Study design and participants
An observational retrospective cohort study was carried out that analyzed the database of patients presenting to the Emergency Department of our hospital with UGIB and underwent an endoscopy between 19th October 2019 and 6th June 2020. Patients older than 18 years were included.
Methods and variables
The following information was available for each patient: demographic data, signs and symptoms before admission, pre-endoscopic management, as well as the date of arrival at the hospital, evaluation by gastroenterology, endoscopy and discharge.
The doctors collected all the information. A medical doctor (HBG) subsequently reviewed the database. Patients were divided into two groups, depending on the time they were treated (pre-pandemic and during the pandemic, respectively) taking into account that in March the first case of COVID-19 was reported in Peru (06/03/2020):
- Phase A: pre-pandemic (19/10/2019 - 29/02/2020).
- Phase B: pandemic (01/03/2020 - 06/06/2020).
Statistical analysis
With 184 patients, a power of 80% was obtained to detect a difference of 3 hours between the patients treated in both groups, assuming a standard deviation of 5 hours. The patient database was downloaded in Microsoft Excel format excluding the personal information of the patients. Statistical analysis was performed using Stata v.10. Categorical variables were expressed using frequencies and percentages whereas numerical variables using measures of central tendency and dispersion. The relationship between categorical variables was analyzed using the Chi square test and Fisher's exact test when necessary. The t-student and Mann-Whitney U tests were used to compare the attention time in each phase. A p-value<0.05 was considered as statistically significant.
Ethical considerations
The protocol was approved by the local Ethics Committee (Comité de Ética en Investigación para COVID-19, Instituto de Evaluación de Tecnologías en Salud e Investigación, 27 May 2020). Informed consent was waived because of the retrospective nature of the study and the analysis used anonymous clinical data. The study protocol conforms to the ethical guidelines of the 2013 Declaration of Helsinki as reflected in prior approval by the local Ethics Committee.
RESULTS
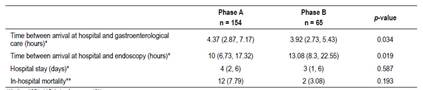
During the period under analysis 219 endoscopic procedures for UGIB were performed. The median age was 69 years (interquartile range (IQR), 58 - 80 years). 136 patients were male (62.10%). The clinical characteristics of the patients during the phases of the pandemic are described in Table 1. There were no differences in the clinical characteristics nor in the number of transfusions between the two groups. 154 endoscopies (1.18 endoscopy/day) and 65 endoscopies (0.68 endoscopy/day) were performed during the pre- pandemic and pandemic phases, respectively.
Table 1 Clinical characteristics according to the phase in which they were admitted.
*Median (IQR), **Relative frequency (%)
During the pandemic phase, two endoscopies were performed in asymptomatic patients with SARS- CoV-2 infection. These two patients had no respiratory symptoms and were diagnosed using a serological screening test prior to endoscopy. Positive IgG was found in the first case and positive IgG/IgM was found in the second case.
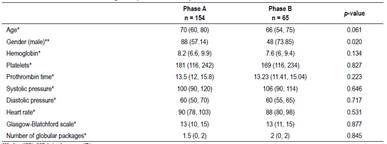
Table 2 describes the patient waiting times. There was no significant difference between the times to evaluation by gastroenterology. However, the time to endoscopy was significantly longer in phase B (p-value = 0.019).
For the first patient with SARS-CoV-2 infection, an early endoscopy had to be prioritized due to hemodynamic decompensation, performed after 15.82 hours. In the second case, conservative management was chosen, obtaining a good result at the beginning, nevertheless, when observing progressive decline in hemoglobin, it was decided to perform an endoscopy almost 530.02 hours after admission. Neither case with SARS-CoV-2 infection died during hospitalization.
DISCUSSION
SARS-CoV-2 infections continues to rise in Peru, forcing health services to reorganize medical work and prioritize patients with COVID-19. These measures have drastically reduced medical care not related to COVID-19, performing only emergency medical care, as occurs in cases of UGIB, whose prognosis depends on the performance of an early endoscopy.
Previous studies report fewer attention in the Emergency Department during quarantine 19-21. This study also observes a lower number of patients with UGIB presenting to our hospital during the pandemic phase, similar to that reported in a study carried out in Austria in which a reduction of 40.7% of cases of UGIB during the quarantine was observed 22. This result could be explained by the difficulty in accessing health services during quarantine, the fear of patients due to the risk of COVID-19 transmission in hospitals, or by the patient's perception that the symptoms are not serious enough to go to a hospital.
The time between arrival at the hospital and the performance of the endoscopy was longer during the pandemic phase. Although a longer delay in performing endoscopy has been observed in patients admitted during the pandemic, this is not expected to cause a delay longer than 24 hours in most cases. However, for one of the patients with SARS-CoV-2 infection, a longer waiting time was observed because conservative management was chosen at the first, eventually producing a larger hospital stay.
Endoscopy is a diagnostic and therapeutic tool in case of UGIB, however it is a potentially aerosol-generating procedure so it is considered a high risk of SARS- CoV transmission 8-12. Even when various guidelines recommend an endoscopy within the first 24 hours in cases of UGIB, the decision to perform the endoscopic procedure have being made on a case by case basis. Unfortunately, there are no clinical guidelines for the management of UGIB during the COVID-19 pandemic but some authors suggest optimizing conservative management at the beginning, prioritizing the performance of procedures based on clinical judgment and the use of pre-endoscopic prognostic tools such the Glasgow-Blatchford scale 6,23. In addition, despite the lack of evidence to recommend an ideal period of time for performing endoscopy in patients with COVID-19, it has been described that this should be done in cases where the patient does not respond to conservative management after 24 hours 24.
A recent study carried out in two hospitals in the United States found that during the pandemic phase, patients presented a lower hemoglobin value and a longer hospital stay compared to patients admitted before the pandemic 25. In contrast, our study does not find a significant difference between the initial laboratory values or hospital stays. In this regard, hospital stays are likely to be similar despite a longer time to perform the endoscopy since efforts are being made to discharge patients shortly after the procedure in order to avoid the risk of infection among hospitalized patients and because of the necessity to increase availability of beds in the Emergency Room.
Evidence of performing an early endoscopy is based on information from pre-pandemic studies, and postponing endoscopy for up to 24 hours has not been shown to affect 30-day mortality in a recent publication 26. Our study suggest evaluating cases according to severity of bleeding and status of SARS- CoV-2 infection. In cases where SARS-CoV-2 infection is confirmed, conservative management evaluating hemodynamic stability and hemoglobin value could initially be considered in non-severe cases (according to clinical judgment and the use of prognostic tools). If adequate response after 24 hours is not observed, performing an endoscopy with adequate PPE is recommended 10-14.
The limitation of our study lies in its retrospective nature; however, all the information was collected in a prospective database, so that, this bias is reduced. On the other hand, the strengths of this study lie in the fact that data contains a large number of patients which allows the comparison of the time to endoscopy and it also represents the first attempt to evaluate the impact of the pandemic by COVID-19 on the care of patients with UGIB in our country.
In conclusion, the management of patients with UGIB in the context of the COVID-19 pandemic is complex and requires the application of clinical judgment using screening tools to decide the best timing to perform an endoscopy with adequate biosecurity measures and guaranteeing the safety of the patient and medical staff.