INTRODUCTION
Intraductal papillary neoplasms of the bile duct (IPNB) is a rare variant of bile duct tumors, and based on the latest World Health Organization (WHO) classification in 2010, is characterized by a papillary neoplasm or villous biliary covering delicate fibrovascular stalks and histological spectrum ranging from benign disease to invasive malignancy 1.
Attention has been drawn to biliary tumors with macroscopically visible mucin secretion, which show predominantly papillary growth within the dilated bile duct lumen and secrete a large amount of mucin 2-3. IPNB presents as an intraductal mass within the dilated intrahepatic or extrahepatic bile ducts on imaging studies. Many terms have also been used to describe this disease including biliary papillomatosis, mucin-hypersecreting intrahepatic biliary neoplasm, mucinosus cholangiocarcinoma, biliary intraductal papillary neoplasm of the liver, ductectatic mucinous cystadenocarcinoma, and biliary intraductal papillary neoplasm 2. The new concept IPNB is the biliary counterpart of intraductal papillary mucinous neoplasm (IPMN) of the pancreas, has been suggested. IPNB with low- or intermediate- and high-grade intraepithelial neoplasia are regarded as premalignant and non- invasive IPNB, whereas IPNB with an associated invasive carcinoma is considered malignant and invasive IPNB 1-3. In this case report and literature review, we describe two cases, IPNB concept, clinical, pathologic, and suggested treatment.
CASES REPORT
Case 1
Comorbid 86-year-old female patient, with a history of cholecystectomy by laparoscopy for symptomatic cholelithiasis in 2018, who presented recurrent obstructive biliary syndrome of two years of evolution, requiring endoscopic intervention of the bile duct by endoscopic retrograde cholangiopancreatography (ERCP) on 5 occasions, and surgical exploration of the bile duct, with cholangiography repeatedly showing an image suggestive of recurrent choledocholithiasis. She was admitted to our institution for emergencies, referred from the outpatient clinic on suspicion of acute cholangitis. On admission, the patient is hemodynamically stable, without respiratory distress in the absence of signs of a systemic inflammatory response, without abdominal pain, asymptomatic. Admission laboratories show as the only positive finding a hemogram with leukocytosis (14,800/ul). Kidney, liver function, amylase, electrolyte levels, acute phase reactants, serum lactate, urinalysis, and chest radiography are within normal limits. A total abdomen ultrasound was performed, identifying a dilated extrahepatic bile duct (12 mm) as positive findings in the presence of pneumobilia, with a normal intrahepatic bile duct.
She was evaluated by gastroenterology, considering the suspicion of acute cholangitis (Tokyo 2018 A2 + C2 criteria), indicating empirical antimicrobial coverage with Ampicillin and Sulbactam. She carried to ERCP, a large duodenal papilla with a large infundibulotomy opening was observed on duodenoscopy. Deep cannulation of the bile duct is performed on the first attempt with an extractor balloon, observing in cholangiography by occlusion a normal intrahepatic bile duct with a dilated extrahepatic bile duct (12 mm common bile duct), identifying the presence of multiple fixed filling defects, which displace the balloon during its removal (Figure 1 A, B and C), obtaining the exit of mucoid material through the papilla. Given the suspicion of a coledocian tumor lesion due to the findings, a single operator (Spyglass, Boston Scientific) choledochoscopy was performed at the same endoscopic time, identifying multiple exophytic lesions of papillomatous appearance, lobed patterned at the distal and middle level and vascular irregularity (Figure 1 D and E), from which biopsies were taken with Spy- bite (Figure 1F).
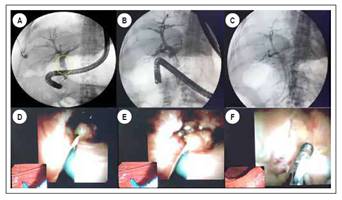
Figure 1 A, B and C. ERCP observing a 12 mm common bile duct in the cholangiography, identifying the presence of multiple fixed filling defects in the middle and distal bile duct. D and E. Cholangioscopy (Spyglass) identifying several exophytic lesions with papillomatous appearance in common bile duct. F. Biopsy of papillomatous lesions described with Spy-scope.
Exploration of proximal common bile duct and hepatic common duct without evidence of lesions, with a usual mucosal and vascular pattern, inserting a plastic biliary stent of 10 Fr x 7 cm, without complications. The pathology report is conclusive for an intraductal papillary neoplasm of the bile duct with high-grade dysplastic changes (Figure 2 A and B). After her discharge from the hospital, she was evaluated by the biliopancreatic diseases service of our institution, considering herself together with family members and taking into account the clinical status and functionality of the patient not a candidate for surgical management, indicating the insertion of a metallic biliary stent uncovered (10 mm x 80 mm), procedure performed without complications.
Case 2
A 73-year-old female patient who required prolonged extra-institutional hospitalization before a bacterial liver abscess and secondary abdominal sepsis, with K. pneumoniae isolation in blood cultures was admitted to our institution with a 2-month history of fever associated with low back pain, with progressive loss of strength in lower limbs. Nuclear magnetic resonance with gadolinium, of the lumbosacral spine confirms the presence of spondylodiscitis at the T11-T12 and T12-L1 level with pathological T12 fracture, as well as extensive multiloculated collections in the psoas muscles, suggestive of abscesses at this level. Complementary contrast CT scan of the abdomen confirms the presence of collections at the level of the psoas muscles (right 102x26x27 mm and left 100x18x22 mm) as well as liver collections (larger than 42x13 mm) and suggestive changes and infectious spondylitis, indicating empirical antimicrobial coverage with meropenem. Drainage of the hepatic, psoas and vertebral collections was performed by interventional radiology, obtaining fluid with purulent characteristics, with isolation of cultures of a K. pneumoniae of the usual pattern, indicating completion of 42 days of directed antibiotic management. Given the presence of a disseminated infectious process with an unclear focus and the suspicion of being of hepatobiliary origin, we decided to perform a complementary cholangioresonance, which identified a filling defect at the level of the proximal bile duct as a positive finding. Taking these findings into account, we consider performing ERCP (Figure 3) plus single-operator cholangioscopy (Spyglass), observing immediately below the confluence of the hepatic ducts a raised, hairy-looking lesion of prominent vessels of approximately 20 mm long, non-obstructive, suggesting the diagnosis of cholangiocarcinoma due to its characteristics. Biopsy is performed with the Spy-bite device, with an inconclusive pathology report, considering a new ERCP plus biopsy taking with conventional forceps guided by fluoroscopy. The pathology report of this new sample is compatible with an intraductal papillary neoplasm of the bile duct (Figure 4).

Figure 3 ERCP observing a dilated common bile duct in the cholangiography, identifying the presence of a filling defect in the proximal segment.
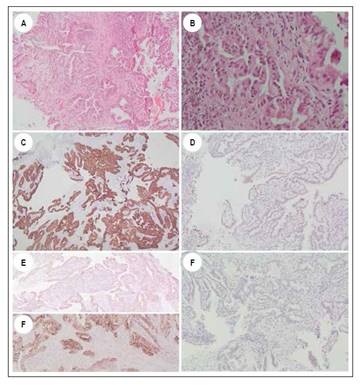
Figure 4 A and B. Hematoxylin-Eosin staining showing fragments of a tubulopapillary neoplasm lined by cubic epithelial cells with moderately pseudostratified pleomorphic nuclei. C and D. Immunohistochemistry study showing positivity of neoplastic cells for CK7 and CDX2. E and F. Immunohistochemistry study showing expression of neoplastic cells for MUC-1 and MUC2. G. Immunohistochemical study shows negativity of the tumor lesion for CK20.
DISCUSSION
Intraductal papillary neoplasm of the bile duct (IPNB) is a rare neoplasm, defined as an epithelial tumor of the bile duct characterized by a papillary growth pattern of an exophytic nature, which generates the formation of intraductal papillary masses that can develop in any segment of the biliary tree 1-3.
First described in 1976 with the name of multicenter biliary papillomatosis associated with invasive adenocarcinoma (4), it is until 2001 that Chen and Nakamura first proposed the term IPNB in the presence of a single tumor made up of multifocal papillary epithelial lesions with or without mucin production in the presence of bile duct dilation 5,6. In 2006 Zen and collaborators proposed the term IPNB to group biliary papillary tumors (biliary papillomatosis and papillary cholangiocarcinoma) as a single entity, the biliary counterpart to intraductal papillary mucinous neoplasia (IPMN-P) 7. In 2010, the World Health Organization (WHO) in its fourth edition, includes these types of tumors as precursor lesions for cholangiocarcinoma, establishing two categories of mucin-producing tumors of the bile duct: cystic mucinous neoplasia and intraductal papillary neoplasia 1,4,8, classifying IPNBs into 4 groups: IPN with low-grade, intermediate, high- grade intraepithelial dysplasia, and IPN associated with invasive carcinoma. Histologically it is characterized by a papillary or tubulopapillary architecture, with four histological subtypes being defined: pancreatobiliary (most common), intestinal, gastric, and oncocytic 3.
Because IPNB is a recently categorized and defined pathology, there are few works that cover this condition, and therefore, little is known about its morphological and clinicopathological characteristics. It is a tumor with wide geographic variation, mainly identified in eastern countries such as Taiwan, Japan, North and South Korea, where hepatolithiasis and clonorchiasis (parasitic zoonosis caused by the liver fluke or Clonorchis sinensis) are endemic. In western countries, its presentation is sporadic and of unknown etiology 3,4,9. It more frequently affects middle-aged patients (between 50 and 70 years) with a certain predominance in the male gender 3. Although its etiology is unknown, chronic inflammation of the bile duct secondary to the presence of biliopancreatic reflux, hepatolithiasis and oriental liver fluke infection (endemic in Asia) is considered a probable causal mechanism 2,9. It is an often asymptomatic condition, being detected incidentally in images or in the study of altered liver function. When symptomatic, they are the result of the development of bile duct obstruction, which leads to biliary colic, jaundice, and sometimes the development of cholangitis 2,3,9, the risk being higher in the presence of a secretory tumor mucin 2. The progression of IPNB to papillary adenocarcinoma has been defined through the adenoma-carcinoma pathway, an invasive component being described in 40 to 80% of reported cases 2,4.
Yaohong et al. in 2015 in their literature review mention a total of 354 cases reported as of the date of publication (52.8% of cases from Japan, 19.5% from other eastern countries such as China, Korea and Taiwan, and 27.7% from western countries such as the United Kingdom, the USA, and Germany), where an average presentation age of 64.6 years (35-80 years) and a male / female ratio of 1,5 are described. Among the clinical manifestations, pain in the right hypochondrium (35-88.5%), recurrent acute cholangitis (5-59%) and obstructive jaundice (20- 36%) were the prevalent findings, being asymptomatic in 5% of the cases. Of the 354 patients, 57.5% were located in the left hepatic lobe, 29.5% in the right lobe and 13.4% in other locations including the common hepatic duct 4. The most frequent histological subtypes found in this study were the pancreatobiliary (41.8%) and the intestinal (28%), with the pancreatobiliary and gastric subtypes being the most invasive 4. Since then, some reports and case series have been published in the world medical literature (Wang 19 cases, Pérez Saborido 3 cases, among others) 10,11. In Colombia, Doctor Martin Gómez in 2015 published the first case of intraductal papillary neoplasm of the bile duct 12.
Regarding the diagnosis of this biliary lesion, imaging studies such as ultrasound and contrast computed tomography (CT) are nonspecific. CT could demonstrate the presence of a hypercapturing biliary focal mass with proximal dilation of the bile duct. Cholanioresonance can show from ductal dilation in the absence of a visible tumor, to a tumor with multiple intraductal papillary projections in the presence of empty areas within the biliary lumen 2. Four radiological manifestations of IPNB have been described that depend on the size and morphology of the intraductal mass: 1) mass with proximal ductal dilation, 2) disproportionate biliary dilation without mass, 3) mass with proximal and distal ductal dilation, and 4) cystic lesions; however, they are not pathognomonic of this condition 9. In 2018, Lee et al. in a retrospective study with 120 patients, found that the findings in cholangioresonance that make it possible to differentiate between IPNB associated with low-grade intraepithelial neoplasia and IPNB associated with invasive carcinoma are: tumor size (≥ 2.5 cm), the presence of multifocal lesions, thickening of the bile duct wall> 3 mm, and invasion of adjacent organs (p value ≤ 0.002) 13. Tumor markers such as CA 19-9 tend to be higher in patients with mucinous neoplasms compared to simple cysts, however, the serum measurement of this tumor marker does not allow a precise differentiation between benign and malignant tumors. Intracystic measurement of Ca 19-9 is an additional method that aids in differentiating a simple cyst from a mucinous cyst 1. In some case series of patients with IPNB, elevation of Ca 19-9 has been reported in approximately 40% 10,14. The exit of a mucoid material by the papilla during duodenoscopy, as well as the presence of multiple small, fixed and irregular filling defects in the cholangiography during ERCP, could help in the diagnosis, however, they are not specific to this pathology. In cholangioscopy, papillary projections of disordered and irregular growth that arise from the biliary walls with a dilated bile duct can be identified (2). For its part, PET-CT may have a role in differentiating between non-invasive and invasive IPNB and papillary cholangiocarcinoma 15.
Regarding the treatment of these lesions, curative resection with negative margins is the treatment of choice in patients candidates for surgical management without compromise at a distance 1,4,9,10. Performing intraoperative cholangioscopy could be useful in determining tumor extension, as well as performing a freeze biopsy to determine surgical margins 10. If there is extensive compromise of the bile duct in the presence of positive margins, consideration should be given to resecting the entire biliary tree by means of a liver transplant with pancreatoduodenectomy 9. In the event that the patient is not a candidate for surgical management, palliative treatment includes chemotherapy, transhepatic percutaneous drainage, endoscopic drainage, laser cholangioscopy ablation, and intraluminal therapy with iridium 192 4. The median survival rate of patients with IPNB is 62 months, better than that of patients with cholangiocarcinoma 4.
In conclusion, biliary intraductal papillary neoplasia is an infrequent pathology and requires imaging, associated with cholangioscopy and biopsy by this method, or by ERCP to achieve a conclusive diagnosis, since it can initially be confused with choledocholithiasis.
















