INTRODUCTION
In the context of chronic diarrhea with structural involvement of the small intestine, differentiating between Crohn's disease (CD) and intestinal tuberculosis (ITB) is not easy, as they may have similar clinical, endoscopic and histological characteristics. In Colombia the incidence of CD is low, arround 0.5/100,000 persons per year 1, while that of tuberculosis is 25/100,000 2, of which 2% have intestinal involvement 3, being the ileocecal junction the most common area affected, followed by jejunum 3. However, the diagnostic error in patients with CD that was initially considered ITB was 17% in one report. In the same series 10% of ITB patients were initially diagnosed with CD 4. We report a case of 34 years old woman with malabsortive chronic diarrhea, which represented a diagnostic challenge between these two entities.
CASE REPORT
A 34-year old woman, housewife previously healthy, complained of 4 years bloodless lyenteric diarrheal stools, on average 6-8 a day and some at night, non localized colickly abdominal pain, transient nocturnal diaphoresis and loss of 15 kilograms of weight, without extra-intestinal symptoms or family history. On physical examination acropaquia and cachexia were found.
Laboratories, imaging and endoscopic studies were performed as shown in Figure 1. The initial results show severe hypoalbuminemia, human immunodeficiency virus (HIV) infection is ruled out and celiac disease serology is negative. Endoscopy and colonoscopy with biopsies were normal.
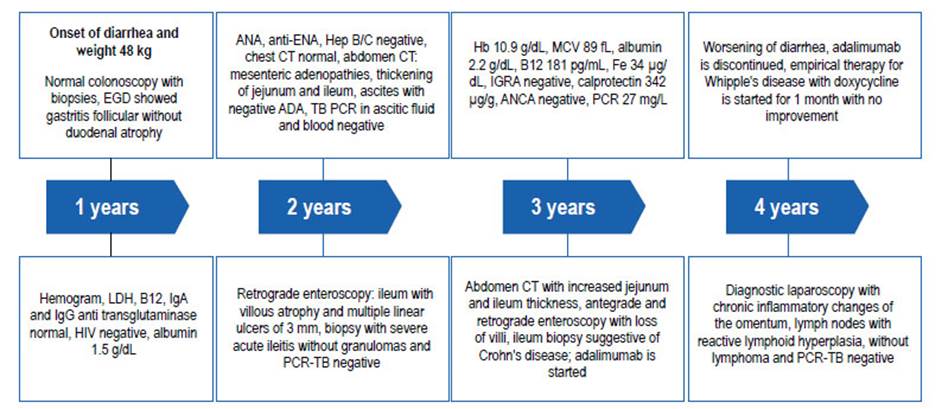
Figure 1 Time line with the evolution and results of studies conducted (year since the onset of symptoms).
The patient presented with non-portal hypertensive ascites, peritoneal tuberculosis was ruled out, abdominal tomography showed mesenteric adenopathies and thickening of the jejunum and ileum, retrograde enteroscopy up to 40 cm of the ileum showed atrophy of villi and multiple 3 mm ulcers (Figure 2A); biopsies were negative for granulomas and polymerase chain reaction for M. tuberculosis (PCR-TB). Given the persistence of digestive symptoms, anemization and elevated calprotectin (Figure 1), anterograde and retrograde enteroscopy was performed, which only evidenced microvilli atrophy in jejunum and ileum (Figure 2B), whose biopsies suggested CD. The interferon-gamma release test was negative and adalimumab was prescribed. After 4 months, the drug was discontinued due to clinical deterioration and diagnostic laparoscopy was performed, inflamed omentum and small lymph nodes were found, but no intestinal lesions; lymph nodes biopsies showed lymphoid hyperplasia and peritoneal PCR-TB was negative.
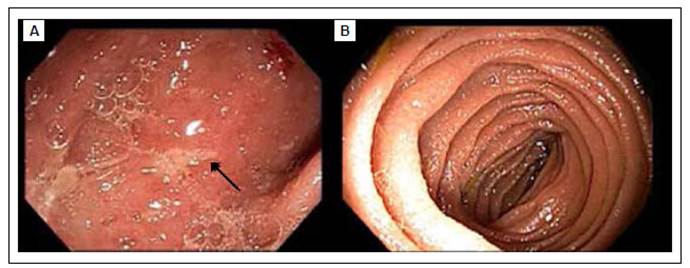
Figure 2 Antegrade and retrograde single-balloon enteroscopy. A. Retrograde enteroscopy with loss of microvilli in the ileum and multiple linear ulcers covered with 3 mm fibrin (arrow). B. Antegrade enteroscopy with decrease of villi in jejunum.
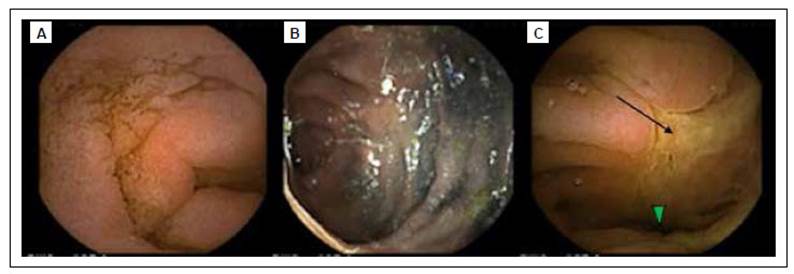
Figure 3 Endoscopic video capsule. A. Flattening of microvilli in jejunum. B. Tattooing with Indian ink of the last antegrade enteroscopy at the jejunum level. C. Stenosis (arrowhead) with ulcer (arrow) in jejunum after tattooing.
By the fourth year, she was admitted to our institution due to symtoms persistence, and severe malnutrition. An endoscopic video capsule was performed showing total loss of villi and ulcerated jejunal stenosis (Figure 3), from which samples were taken by laparoscopic- assisted enteroscopy (Figure 4). Biopsies with lymphoplasmocyte infiltration, without granulomas, silver staining, Ziehl-Neelsen and PCR-TB were negative. Due to the suspicion of ITB, it was empirically managed with isoniazid, rifampicin, ethambutol, pyrazinamide; after just 3 weeks there were marked improvement of symptoms. Two months later, a positive culture for M. tuberculosis from endoscopic biopsy was obtained.
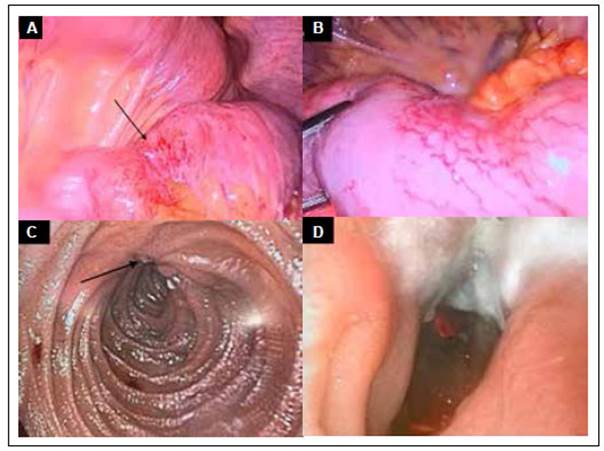
Figure 4 Anterograde single-balloon laparoscopic-assisted enteroscopy. A. Laparoscopy in which thickened and retracted mesentery 60 cm from the Treitz ligament is observed, with a small segment of a stenotic intestinal loop (arrow). B. Enlargement of image A with segment of stenotic and hypervascularized jejunum. C. Enteroscopy showing ulcer (arrow) with folds converging towards it. D. Transverse ulcer occupying 50% of the circumference, with whitish secretion and stenotic effect of 80% of the jejunal lumen.
DISCUSSION
As presented in case, it is not easy to differentiate between CD and ITB by reported clinical, endoscopic, radiological or histological findings. Tuberculosis is an endemic disease in Colombia as in regions of Southeast Asia and Africa. In 2018, 10 million new cases were reported worldwide (2.5), of which 8.6% were co- infected with HIV 5. Extrapulmonary involvement occurs in 20% of immunocompetent patients and 50% in immunocompromised individuals 6, of which 60% have no pulmonary involvement documented by culture or radiographic lesions 3,7. ITB is acquired by swallowing sputum or food with the tubercle bacillus, unpasteurized dairy products, by a hematogenous or lymphatic route, initiating infection in the lymphoid tissue of the submucosa 3,6. On the other hand, CD is a chronic inflammatory entity of unknown cause with associated genetic, environmental and microbiological risk factors 8. It occurs more frequently in the United States and northern Europe, with an incidence between 10-21/100,000 people per year 9.
The clinical manifestations are similar, with abdominal pain, diarrhea, anorexia and weight loss being the most frequent. There may be extraintestinal symptoms such as arthralgias, dermatological lesions or ocular involvement. Gastrointestinal compromise includes strictures, ulcers, fistulas and perforations 10. In CD the most frequent symptoms are diarrhea, hematochezia, perianal disease and extraintestinal manifestations, while in ITB the most frequent symptoms are anorexia, abdominal pain, ascites and nocturnal diaphoresis 11.
Correct diagnosis is important since the prognosis and management of CD and ITB are different, and the delay of specific treatment increases the risk of complications 7. Only the presence of caseating granulomas, alcohol-resistant acid bacilli, culture or positive PCR-TB are unequivocal for ITB 11.
The imaging techniques, like the radiology and endoscopy, are used for the initial approach in ITB; The tomographic findings related to this disease are perforation, intestinal obstruction with hourglass image due to the smooth contour of the stenosis, thickening of the distal ileum and the medial wall of the cecum, which may have enhancement and adenopathies >1 cm with central necrosis (present in inflammation or neoplasia) 3,11,12. In CD there is asymmetric thickening of the intestinal wall >3 mm with enhancement, long segmental involvement >3 cm, scalloped mesentery and the sign of the comb due to engorgement of the straight vessels (this is the most suggestive of CD) 8,10,13. The magnetic resonance visualizes better small bowel lesions, edema, and even the apparent diffusion coefficient (ADC) allows assessing the activity in CD and the response to management in ITB 13,14. Interestingly, in our case imaging findings were not typical of any disease.
Endoscopically, both can have lesions from the esophagus to the rectum, but the ileocecal area is the most involved. In CD, aphthous and longitudinal ulcers predominate, forming a cobblestone pattern, the mucosa around the ulcer is generally normal 15, while in ITB, transverse ulcers predominate, the edges are hypertrophied and there is yellow or white exudate as in our case (Figure 4D), the perilesional mucosa usually has inflammatory changes, scars or pseudopolyps. Elevated nodular lesions can also be observed forming masses, mainly close to the ileocecal valve, which can be found stenosed, deformed or "patulous" 3,10,15. Of note, here we report an infrequent findings for ITB, showing diffuse microvilli atrophy and scattered small ulcers without hypertrophy.
The culture and PCR-TB sensitivity are <60%, but there is a Bayesian prediction model available on the website https://www.pathology.med.umich. edu/shiny/tbcrohns/, which for our patient calculated a probability of ITB prior to culture of 84.6%. In the model, the findings with the highest LR+ for CD are perianal disease, extraintestinal manifestations, longitudinal ulcers and cobblestone pattern; in ITB they are nocturnal diaphoresis, pulmonary involvement, ascites, transverse ulcers and patulous ileocecal valve. This model was validated in Thailand, finding sensitivity of 90% and specificity of 92% 16.
Finally, in our case it was possible to confirm ITB, but since up to half of the cases may not have microbiological isolation, the Asia-Pacific guidelines 17 recommend empirical treatment with tretaconjugate for 8-12 weeks; if there is no improvement or it is partial, consider CD or resistant tuberculosis and the endoscopic study and imaging should be repeated; otherwise complete the tetraconjugate for 6 months and repeat the endoscopic study to determine cure of the mucosa 10,11,17.
Contributions: VA Costa provided the video capsule images, reviewed the manuscript and is the guarantor of the article. AF Delgado wrote and reviewed the manuscript. AM Leguízamo reviewed the manuscript and provided the enteroscopy and laparoscopy images. RD Vargas reviewed the manuscript.















