INTRODUCTION
Portal vein thrombosis, is a rare condition described as an obstruction of blood flow in the portal vein 1. Many conditions ranging from prothrombotic states to paraneoplastic syndromes can trigger its onset and progression of thrombosis over time can develop serious complications 2.
We present the case of a 29-year-old woman diagnosed with portal vein thrombosis in whom a laparoscopic splenectomy and proximal splenorenal shunt with distal pancreatectomy was successfully performed.
CASE REPORT
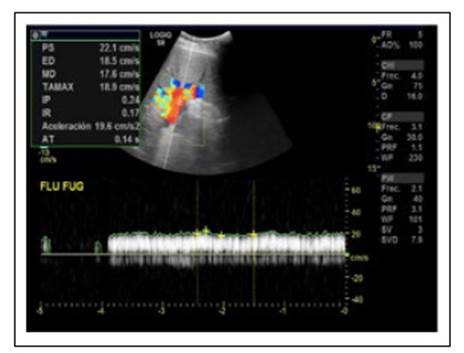
A 29-year-old woman came as an ambulatory patient seeking for treatment for a disease diagnosed before. Born in a jungle developing region in Peru without access to medical services, she was delivered at home under no medical assistance. Days after delivery, her mother evidenced erythema around the umbilical cord that was untreated and lasted for six months, after which it resolved spontaneously. At the age of 6, she debuted with upper gastrointestinal bleeding; esophagogastroduodenoscopy was performed with evidence of bleeding esophageal varices. Portal Doppler echography and abdominal tomography were performed and portal vein thrombosis was diagnosed (Figure 1). No treatment was given nor anticoagulation at that moment and was discharged only with propranolol.
The patient continued her exams few years later due to lack of medical and economical resources. During the next years, she developed hypersplenism with occasional abdominal pain and splenic sequestration with minor epistaxis episodes.
Fifteen years later her blood exams were abnormal as follows: hemoglobin, 11,3 g/dL; mean corpuscular volume and hemoglobin in 84,5 and 29,2 respectively; leucocytes, 1,6x103/mm3; platelets, 60x103/mm3 with medium plaquetary volume 9,7 fL. Serum iron, 51 mg/ dL; transferrin, 285 mg/dL; percentage of transferrin saturation 18%; seric homocysteine 9,9 μmol/L. Prothrombin time was within normal values. Total bilirubin, 0,95 mg/dL; total seric protein, 6,05 g/dL; albumin 3,82 g/dL; globulin 2,23 g/dL; ALT 14 U/L; AST 25 U/L; alkaline phosphatase 33 U/L; creatinine 0,61 mg/dL; protein S 29% (NV: 60-130); protein C 73% (NV: 70-140); factor V Leiden, 41,7% (NV: 70-120) but with a negative molecular analysis for mutation Factor V Leiden in real-time PCR. IgM and IgG anti-cardiolipin and B2-glicoprotein were within normal values. Serological tests for HIV, VDRL/RPR, HCV, HBsAg, were all negative as well as mutation of prothrombin, C677T and A129 in gen MTHFR.
Chest tomography revealed a prominent pulmonary artery (3,5 cm) with suspicion of pulmonary hypertension.
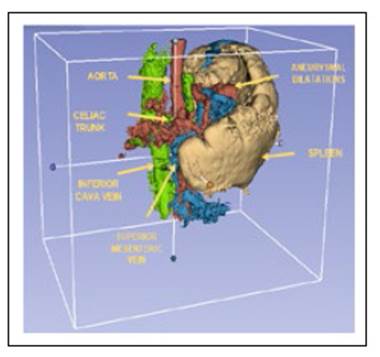
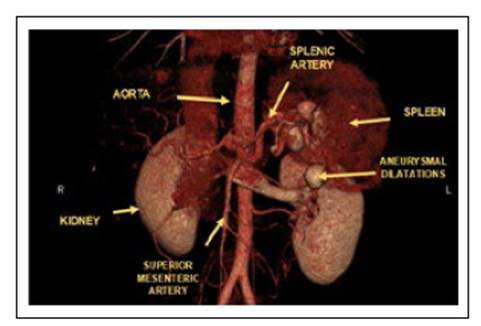
Abdominal tomographic images suggested portal vein thrombosis with multiple hypervascular nodular images in the liver that could correspond to arterioportal shunts. The patient presented moderate splenomegaly associated to portal hypertension signs with tortuous veins in the splenic hilium, perigastric and splenorenal space. Dilation of the splenic artery with saccular aneurysmal at the splenic hilum were present (Figure 2 and 3).
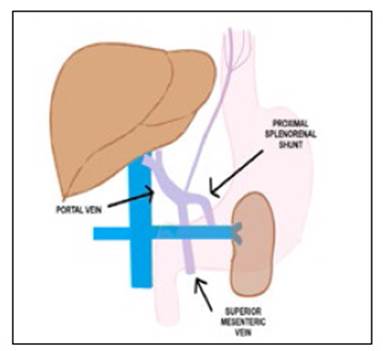
Laparoscopic splenectomy and proximal splenorenal shunt were proposed as surgery of choice (Figure 4). Informed consent was signed by the patient. During surgery, the liver presented normal appearance but giant spleen with multiple collateral circulation toward the renal vein was identified. The splenic vein was turgid with an intraluminal pressure of 19 mmHg as well as the left renal vein. Terminal-lateral anastomosis between the splenic vein and the left renal vein was performed without complications and pre hepatic portal hypertension was recognized. Distal pancreatectomy had to be performed because of proximity to aneurysmal dilatations of the splenic artery. After surgery, platelets raised up to 200x103/mm3.
At discharge, she was given anticoagulation treatment with Apixaban 5 mg twice a day.
DISCUSSION
Portal vein thrombosis (PVT) is defined as an obstruction of blood flow in the portal vein caused by the presence of a thrombus in the vasal lumen which can be partial or complete (1.
PVT is a non-frequent disease in the general population although prevalence in cirrhotic patients can range between 10-25% 2. It can be caused by inherited conditions as factor V Leiden, antithrombin, protein S and C deficiency and acquired conditions as neonatal funiculitis, lupus, cirrhosis, sepsis or malignancy 3.
Protein S is a natural anticoagulant synthetized in the liver and deficiency can be related to deep vein thrombosis, pulmonary embolism and less common cerebral, mesenteric or portal thrombosis 4. Its prevalence is difficult to stablish; however, on Scotland healthy volunteers the prevalence of familial protein S deficiency was between 0,03% and 0,13% 5 with a 2-11-fold increased risk for thromboembolism along with protein C deficiency 6.
In the present case, two conditions might have triggered the PVT: neonatal funiculitis and protein S deficiency. Unfortunately, there is no certain way to assure the presence of an umbilical cord infection in the infancy; however, conditions in which the patient was born can be strong predictors of neonatal funiculitis. On the other hand, primary deficiency of protein S has to be considered, as there was no liver function impairment such cirrhosis in our patient that can account for secondary causes of deficiency. No anticoagulant administration was given and was not the setting of an acute thrombotic event 7.
Laparoscopic splenectomy and proximal splenorenal shunt (PSS) were proposed due to absence of cirrhosis and preserved liver function. The PSS decompresses effectively the portal vascular system, reduces portal hypertension and has been widely used in portal vein obstruction 8. Distal pancreatectomy had to be performed because of vascular compromise and presence of saccular aneurysms.
In the literature, Deshpande et al, reported protein C-S deficiency in a non-cirrhotic 24-year-old male who debuted with acute superior mesenteric and PVT in which protein S activity was 38% (65%-140%); the patient was successfully treated with anticoagulation and no surgery intervention was needed 9. Rodríguez- Leal et al also identified protein C-S deficiency in a 63 non-cirrhotic patient who developed PVT and was treated successfully with enoxaparine and warfarin 10. Finally, Choi et al reported a total PVT recanalized by oral anticoagulation in a context of protein C-S deficiency 11.
Irawan and Mulyawan described a combination of modified Sugiura technique and proximal splenorenal shunt for reducing portal vein flow in a 59-year-old man with noncirrhotic portal hypertension due to portal vein thrombosis, who presented to the emergency department with upper gastrointestinal bleeding. After the procedure, the patient also evidenced improvement in physical condition and had no complications 12. Anand et al, reported 25 cases of proximal splenorenal shunt in non-cirrhotic portal hypertension for management of gastric variceal hemorrhage. After failing endoscopic therapy, patients were eligible for surgery. Follow-up evaluation was only performed to 20 patients; however, all of them evidenced variceal regression, and only 2 presented variceal rebleeding 13.
First line treatment is anticoagulation, second line includes mechanical thrombectomy, thrombolysis and interventional radiographic procedures or surgery (7). In patients with chronic PVT, indefinite anticoagulation is recommended in documented prothrombotic state, recurrent thrombosis or intestinal infarction 14,15. Our patient with a prothrombic state, was discharged with indefinite anticoagulation as no medication given is associated with new thrombotic events 16.
In conclusion, laparoscopic splenectomy and proximal splenorenal shunt for portal hypertension due to PVT is an adequate surgery procedure which should be applied in these medical cases. PVT is a complicated disease that should be diagnosed and treated immediately to avoid chronic consequences that can be irreversible and might require surgery treatment.