INTRODUCTION
Epithelioid hemangioendotheliomas are rare vascular neoplasms that commonly involve the liver 1. Hepatic epithelioid hemangioendothelioma (HEHE) is a rare tumor with an incidence rate of less than 0.1 per 100,000 people 2. It was first described by Ishak et al. in 1984 3. It can present from childhood to late adulthood, and it predominantly affects females 4,5. The clinical spectrum of HEHE ranges from asymptomatic to liver failure 6. We describe a case of HEHE in a 26-yearold male with non-cirrhotic portal hypertension. We present the following article in accordance with the CARE reporting checklist.
CASE REPORT
A 26-year-old male was referred to our department with a misdiagnosis of liver cirrhosis. The patient reported abdominal distention lasting three weeks prior to his diagnosis. The patient’s medical history was unremarkable, and he denied smoking or alcohol abuse. He had no family history of hepatic diseases.
On physical examination, ascites was identified by shifting dullness. All biochemical tests, including tumor markers, were within the normal ranges. Serum surface antigen for hepatitis B and anti-hepatitis C virus were negative. Anti-microsomal, anti-mitochondrial, antinuclear, and anti-smooth muscle antibodies were negative for autoimmune disease.
The chest and abdominal contrast-enhanced computed tomography (CT) revealed hepatomegaly with multiple nodules, forming coalescent lesions involving the peripheral liver, with heterogeneous contrast enhancement in segments IV and VI. Extrahepatic metastasis was not found. The largest lesion, measuring 79 mm x 93 mm, was in segment VI. Furthermore, the CT imaging findings showed dilated portal and splenic veins due to portal hypertension (17 mm and 10 mm, respectively) (Figure 1). Based on these, the patient underwent laparoscopic biopsy, which revealed an irregular surface with multiple whitish areas in the liver. A biopsy sample (30 mm x 30 mm x 20 mm) was taken at the largest lesion in segment IV. Pathological examination demonstrated that the tumor cells infiltrated the hepatic sinusoids and small vessels. In the remaining hepatic parenchyma, a hepatic architecture without fibrosis was observed. On immunohistochemical staining, the tumor cells tested positive for Factor VIII, CD31, and CD34 (Figure 2). The patient was referred to transplant surgery for liver transplant evaluation.
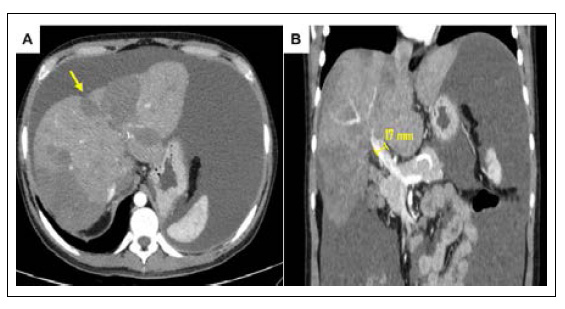
Figure 1. Contrast-enhanced images on CT. A) Coalescent hepatic nodules in peripheral location with capsular retraction (yellow arrow). B) Dilated portal vein.
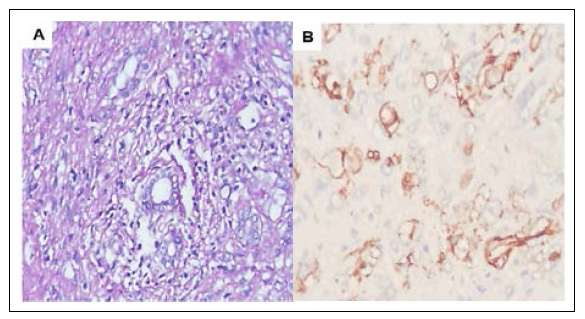
Figure 2. A) Tumor cells have infiltrated the sinusoids (hematoxylin and eosin staining x 200). B) Tumor cells were positive for the endothelial marker CD34 (CD34 immunostaining x 400).
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
DISCUSSION
To the best of our knowledge, this is the first reported case of HEHE with non-cirrhotic portal hypertension in Peru. HEHE is a rare tumor of vascular origin with only one to two cases for every one million people 2. Although this entity was termed for the first time by Weiss and Enzinger (1892) 7, HEHE was first described in a series of 32 cases by Ishak et al.3 (1984) as a tumor with primary liver involvement. The average age of presentation is 30 to 50 years old, with a female-tomale ratio of 3:2 2.
The etiology and risk factors of HEHE are unknown. Some possible etiologic factors include oral contraceptives, vinyl chloride, asbestos, major liver trauma, viral hepatitis, primary biliary cholangitis, and alcohol consumption 8-10. A quarter of cases are asymptomatic. The clinical manifestations of HEHE are generally nonspecific. These symptoms include right upper quadrant pain or weight loss, but some patients may present with liver failure, Budd-Chiari syndrome, or portal hypertension 3,5,6. In our present case, the patient had ascites, probably due to portal hypertension, related to the diffuse presentation of HEHE. In terms of laboratory findings, HEHE is typically characterized by slightly increased glutamyl transpeptidase, aspartate aminotransferase, alanine aminotransferase, and total bilirubin 6. Tumor markers including AFP, CEA, and CA 19-9 usually remain within normal limits, but some cases may have increased CEA 6.
Two different types of HEHE can be identified using imaging techniques. The earlier stage, which is the nodular type, is characterized by multifocal nodules with bilobar involvement. In the advanced stage, the confluent type, these nodules coalesce involving the peripheral liver and invading the great vessels 11. The last stage causes intrahepatic congestion, decreasing the portal vein flow and eventually inducing portal hypertension, as reported in this case. An abdominal ultrasound (US) is the first imaging study to assess HEHE, but US findings are often nonspecific. Hypoechoic nodules, calcifications, and mixed echogenicity lesions are described in US examination 12. A single study demonstrated typical signs (hyperenhancement in the arterial phase and hypoenhancement in the portal phase) of HEHE using contrast-enhanced US for suspected malignant lesions 13.
HEHE has specific CT and magnetic resonance imaging features. A capsular retraction associated with the peripheral location of coalescent hepatic nodules is a characteristic image of HEHE 14. Coalescent lesions were observed in the present case. In contrast-enhanced studies, there are two specific radiological findings of HEHE, the "Target sign" and the "Lollipop sign." The target appearance is produced by peripherally proliferating cells surrounding a central dense fibrous stroma, which, during dynamic study, manifest as a hypodense/hypointense core and a layer of enhancement 15. The "Lollipop sign" is composed of a hepatic vein or portal vein extending towards the HEHE and terminating within or at the edge of the hepatic lesion 16.
Histologically, HEHE is characterized by individual and small groups of three tumor cell types: epithelioid cells with a mucopolysaccharide-rich stroma, dendritic cells in the myxoid stroma with irregular shapes, and intermediate cells. The acinar architecture is preserved, but the liver cell plate disappears due to tumor cell growth around the hepatic sinusoid and veins. The epithelioid tumor cells have abundant cytoplasm and intracytoplasmic vacuoles, representing intercellular vascular lumina and contain red blood cells. Older lesions exhibit progressive fibrosis 17. Immunohistochemical staining of Factor VIII (99% of cases), CD34 (94%), and CD31 (86%) are positive in HEHE 18.
There is no standardized therapy or consensus treatment guidelines for HEHE due to its low incidence and variable behavior. However, there are published studies documenting observation strategy, chemotherapy, radiotherapy, anti-angiogenic drugs, liver resection, and liver transplantation (LT) in HEHE treatment 17. As seen in the present case, multiple bilobar hepatic lesions was the most frequent presentation. Thus, LT is considered the first-line treatment. In a multicenter retrospective study of 110 patients, who underwent LT between 1987 to 2005, Rodriguez et al.19) demonstrated good 1-year and 5-year overall patient survival rates (80% and 64%, respectively). In a large patient cohort of 149 transplanted patients from 1984 to 2014, the European Liver Intestine Transplant Association confirmed the significance of LT in managing HEHE (5-year and 10-year survival rates of LT were 79.5% and 74.4%, respectively) 4. Moreover, the study developed the HEHE-LT score based on the independent risk factors for post-LT recurrence (macrovascular invasion detected at pathology, a time to LT of at least 120 days and hilar lymph nodes infiltration). A lower score suggested a more favorable 5-year disease-free survival than a higher score (93.9% vs. 38.5%, respectively).
In conclusion, HEHE is an uncommon disease entity with metastatic potential and variable clinical course. Imaging modalities aid its diagnosis, and liver biopsy with immunohistochemical staining is necessary to differentiate it from other malignant lesions. This case increased the knowledge and educational value of a rare cause of non-cirrhotic portal hypertension.















