INTRODUCTION
Segmental arterial mediolysis (SAM) is a rare but severe non-atherosclerotic and non-inflammatory vasculopathy of unknown etiology. It is characterized by the lysis of the medial layer of the arterial wall, often resulting in dissection, aneurysm, occlusion or stenosis 1-3, and, has a peak incidence in individuals between 50 to 80 years of age, predominantly males 4.
SAM most commonly affects the branches of the abdominal aorta, such as the celiac, mesenteric and/ or renal arteries, with occasional involvement of the carotid, cerebral and coronary arteries 5. Depending on the artery involved and the underlying pathology (dissection with stenosis versus rupture), patients with SAM may experience chronic abdominal pain, acute mesenteric ischemia or even hemorrhagic shock 5. Since the first case of SAM described by Slavin and Gonzalez-Vitale in 1976, approximately 111 cases have been described in the literature until 2018 2,6.
The etiology remains unknown, however, the histopathological changes of SAM begin with vacuolar degeneration of smooth muscle cells, followed by the deposition of fibrin in the adventitious layer of the arteries. This, in turn, predisposes the rupture of the arterial medial layer, with resulting susceptibility to vessel dissection, hemorrhage and ischemia, being one of the main causes of spontaneous intra-abdominal hemorrhage 7.
The most common clinical presentation is abdominal pain, varying with the severity of the symptoms, such as flank pain, hematochezia, stroke, hemoptysis, headache, back pain as well as also resulting in catastrophic presentations, such as retroperitoneum hemorrhage, or aneurysm in the brain due to rupture or dissection 1.
There is a lack of literature addressing the diagnosis, management and prognosis of SAM, with conflicting data on its morbidity and mortality. Since its original description by RE Slavin and JC Gonzalez-Vitale in 1976, case reports continue to comprise most of the literature related to SAM 7.
CASE REPORT
S.R.M, the case subject, a 57 year old male, came to the gastroenterology service department with crisis pain in the left iliac fossa and had abdominal distension which started 7 years previous. S.R.M underwent palliative treatment with medication for the relief of symptoms. Upper gastrointestinal endoscopy showed enanthematous gastritis in antrum with H. pylori (-), magnetic resonance imaging of the abdomen (Figure 1), which suggested dissection of the iliac arteries.
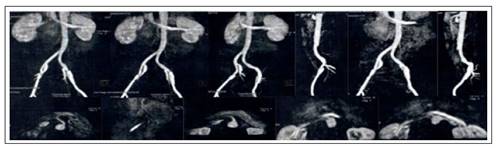
Figure 1 Abdominal Magnetic resonance angiography. Focal dilation of the proximal and middle thirds of the left external iliac artery, specified by the presence of a mediointimal flap, characterizing vascular dissection. And presence in the distal middle third of the left renal artery focal dilation, compatible with a mediointimal flap in the central portion, findings suggestive of vascular dissection.
For better investigation, a computerized angiotomography was requested for the same date, which subsequently showed focal bulging of the right internal carotid artery, which might have indicated a possible aneurysm or pseudoaneurysm (Figure 2). Due to exam results, it was requested that S.R.M undergo vascular US, which showed segmental aneurysm of the right external iliac artery with dissection in the dilation and segmental aneurysm of the left external iliac artery with discrete mural thrombi.
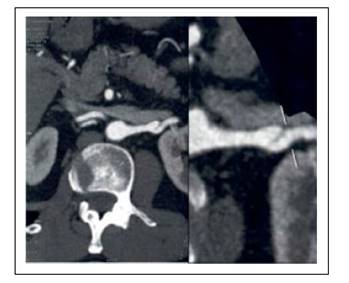
Figure 2 CT angiography of the thoracic aorta: saccular aneurysms in the middle third of the left renal artery measuring about 9 mm.
Continuing the investigation, AngioTC was requested a month later, which demonstrated a thoracic aorta with saccular aneurysmal dilation in the left renal artery, without signs of mural thrombi, and within the abdominal artery the angioTC demonstrated focal dilations of the external iliac arteries and left renal artery, accompanied by intraluminal intimal medial flap, compatible with vascular dissection. With the finding of 4 aneurysms in the imaging exams, combined with the delayed clinical diagnosis due to abdominal pain, the diagnosis of arterial mediolysis with abdominal angina was finally reached. Currently, the patient is stable and in the preoperative period of cholesteatoma.
DISCUSSION
The patient in question presented himself at peak age for the incidence of this pathology, with the clinical condition of unexplained and long-lasting abdominal pain, which may encompass a myriad of gastrointestinal pathologies, however, is also a typical symptom of SAM. Abdominal pain is the most common clinical presentation of SAM, being present in 60% of the cases described 4. It is well described in the literature that the angiographic appearance of SAM is variable, with a predominance of aneurysms, which commonly affect the branches of the abdominal aorta, such as the arteries of the celiac, mesenteric and/or renal arteries, with occasional involvement of the carotid, cerebral and coronary artery 8. Coincidentally, the case studied by this paper, in which the patient presented 4 aneurysms in arteries that are derived from the abdominal aorta, corroborated the diagnostic hypothesis.
Due to the scarcity of descriptions in the literature, there is no current consensus on common criteria or best practices for diagnosing SAM, however the pathology should be considered as a diagnostic hypothesis in patients who have unexplained or chronic acute abdominal pain, aneurysms or spontaneous ruptures of visceral arteries, it is worth mentioning that diagnostic images and/or histology are necessary to aid the diagnosis and exclude other arteriopathies similar to inflammation, infectious or hereditary diseases 9.
The principal differential diagnosis that must be taken into consideration during the medical investigation of SAM is arteriosclerosis, fibromuscular dysplasia, systemic inflammatory vasculitis, connective tissue diseases, neurofibromatosis, and inherited defects in vessel wall structural proteins 5.
Initially we avoided the premature and likely diagnosis of arteriosclerosis of the abdominal wall due to the patient lifestyle as well as the laboratory exams which did not corroborate with dyslipidemia. In addition, in imaging exams arteriosclerosis is generally disseminated in many regions of the vascular branches, whereas SAM is generally limited to anatomically local vessels 9. Yet, another important differential diagnosis, but difficult to avoid is fibromuscular dysplasia (FMD), especially since SAM is frequently considered a premature lesion of FMD 10,11. Classically, FMD presents itself in young women and the predisposition to renal arteries, causing premature hypertension. FMD, another classified pathology in the spectrum of SAM diseases is characterised by medial cystic necrosis (NMC) 11. However, normally NMC occurs within the aorta and large vessels in patients carrying Marfan syndrome 12, in such a way that these vessels are not normally affected by SAM, therefore such a pathology is eliminated due to the absence of clinical compatibility.
Thus, a differential diagnosis it is important to rule out the possibility of systemic inflammatory vasculitis prior to the diagnosis of SAM, since corticosteroids and immunosuppressive agents, which are fundamental in the treatment of inflammatory vasculitis, have no proven benefit in SAM, and may even delay the correct course of treatment 13. The treatment of MAS involves embolization, surgical bypass or resection of the injured arteries. The long-term prognosis of SAM is somewhat uncertain, as its natural history has not been fully characterized. It is known, however, that although cases of SAM complicated by intra-abdominal hemorrhage have a mortality rate of approximately 50%, the most common scenario is long-term disease- free survival after treatment 14.
The diagnosis of this pathology is a challenge for the physician, due to the complexity and scarcity of research on SAM. The diagnosis has histology as the gold standard, and the use of computerized tomography scans is an apparatus in determining and monitoring this pathology, which, added to the clinical history presented and physical examination, corroborates pathological identification.
In the case described, the anamnesis, added to the clinical history, physical examination and a wide range of complementary tests requested, helped and corroborated a favorable outcome to the case.















