INTRODUCTION
Liver transplantation is the most complex medical- surgical process in contemporary medicine today, due to the fact that it involves the care of a multi-organically compromised patient, who requires advanced and quality intensive support with the participation of a multidisciplinary team. Multi-organ monitoring in a transplant center is essential since this is part of the edge that will affect morbidity and mortality of the liver graft.
In the late 1950s, transplantation models in dogs were developed for all intra-abdominal organs. The most fruitful of these efforts involved the liver 1. Liver transplantation remains the only definitive treatment for patients with fulminant liver failure and irreversible liver injury. In 1963 Dr. Thomas Starzl performed the first liver transplant in humans, in Denver - USA 2; in Peru, Dr. Jose Chaman; successfully started liver transplantation activity in March 2000 at the Guillermo Almenara National Hospital (EsSalud).
The key factors affecting post-liver transplant survival are the severity of the recipient's pre-transplant disease and the quality of the graft used 3. The more severe encephalopathy there is at the time of surgery or the severity of multisystem organ failure, the less likely the surgery will be successful. There are several risk factors that have been associated with a decrease in the probability of survival of the patient after liver transplantation, including a history of life support, recipient age > 50 years, recipient BMI >= 30 kg/m2, and serum creatinine > 2.0 mg/dL 4. The main causes of death in the post-transplant period are sepsis and multi-organ failure 5.
The different phases of transplantation, from the search and qualification of the recipient to subsequent management, immunosuppression and its complications, have been notably systematized, achieving progressively better results. However, the low organ donation rate in Peru (2.28 pmp) continues to be a challenge, so an uninterrupted commitment is necessary.
Liver transplantation at the beginning was associated with large volumes of bleeding and the need for blood products with long and difficult post-transplant ICU course, however, advances in surgical and anesthetic techniques have streamlined the intraoperative course, now being a “routine”, allowing modifications of the practice to reduce perioperative complications and costs. The MELD score established for organ distribution in the USA in 2002, as well as in most liver transplant centers and in Peru in 2008, as a disease severity score, with a greater acceptance of donors with expanded criteria and, the acuity of the receptors, more patients are admitted to the operating room from the ICU, where they have required support in the face of respiratory failure, hemodynamic instability or severity of portosystemic encephalopathy.
More than 20 years of experience have passed with favorable results, and with different types of medical- surgical complications. In this sense, the present study aims to present the results of our experience in the Intensive Care Unit since March 23, 2000 to October 31, 2020.
Management in the intensive care unit requires specialists in intensive medicine that provide evidence- based therapeutic interventions, providing support for multiple organs, with a holistic view of the patient. The intensivist with training in transplant complications management and immunosuppression is ideally trained in an international or national transplant center and accredited by government entities.
MATERIALS AND METHODS
A descriptive, retrospective, cross-sectional study was conducted that included 243 adult patients with orthotopic liver transplantation. The inclusion criteria were all patients over 18 years of age, liver transplants who were treated in the Intensive Care Unit in the immediate postoperative period, the exclusion criteria were those under 18 years of age, double transplants (liver - kidney), retransplants, SPLIT or domino transplants. The data were obtained from the medical records and the database of the Transplant Department at the Guillermo Almenara National Hospital.
The statistical analysis consists of the description of the different sociodemographic, clinical and surgical variables of the patients under study, mentioning the pre-transplant situation, intra- and post-operative variables in ICU and hospitalization. The Microsoft Office Excel and SPSS (version 25) programs were used.
RESULTS
During the study period, 243 patients were included out of a total of 302 transplants.
Pretransplant findings:
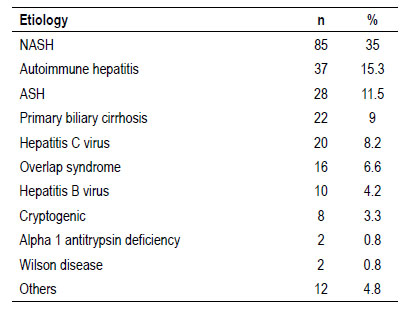
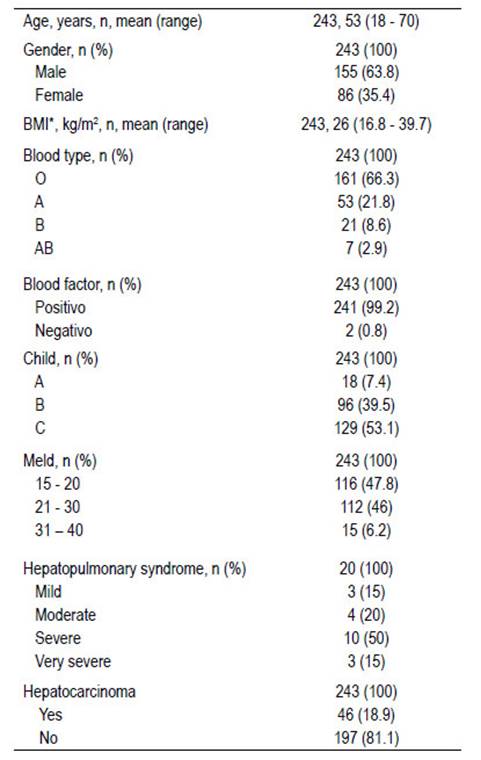
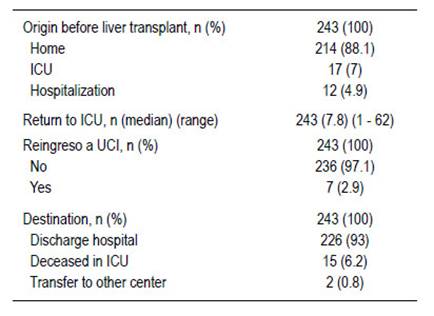
Sex and gender: average age: 49 years range: 18 to 70 years, gender: male (63.8%). Etiology: NASH (35%), autoimmune hepatitis (15.3%), ASH (11.5%), primary biliary cirrhosis (9%), viral hepatitis among others (Table 1), other etiologies in many fewer were alpha 1 antitrypsin deficiency, Caroli's disease, Wilson's disease, Budd Chiari syndrome, and polycystic hepato- renal disease among others. Severe hepatopulmonary syndrome predominated in 10 patients (50%), 197 (81.1%) patients had hepatocarcinoma, average BMI at 26 kg/m2, CHILD C (53.1%), MELD score: 15 - 20 points (47.5%). The patients origin: domicile in 214 (88.1%) and ICU: 17 (7%). Tables 1 and 2.
Operating room findings:
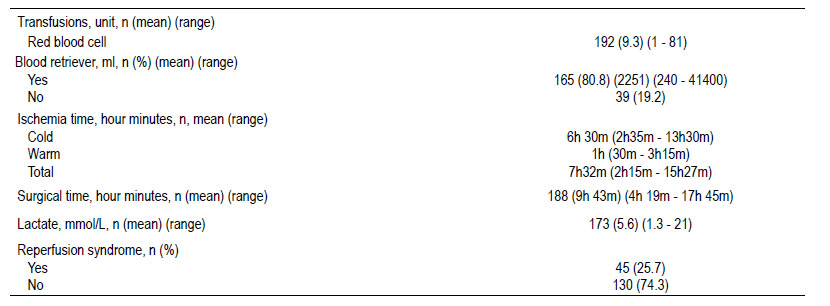
Ascites 4219 ml, intraoperative bleeding: mean 6393 cc. Red blood cell transfusion: average 9.3 units. Ranges: 1-81. Use of cell saver: 165 (80.8%) patients. Average 2251 cc. Cold ischemia time: average 6 hours 30 minutes. Range 2 hours 35 minutes - 13 hours 30 minutes. Average warm ischemia time: 1 hour. Ranges:
30 minutes - 3 hours 15 minutes. Ischemia time: 7 hours 32 minutes’ average. Surgical time: 9 hours 43 minutes. Intraoperative lactate: 5.6 mmol/L. Ranges: 1.3 - 21 mmol/L. Reperfusion syndrome 45 (25.7%) patients. Table 3.
Surgical complications:
Relaparotomy: 67 patients. Hemoperitoneum: 20
(29.9%) patients, diagnostic laparatomy: 10 (14.9%) patients, and hepatic artery thrombosis: 7 (10.4%).
Intensive Care Unit findings:
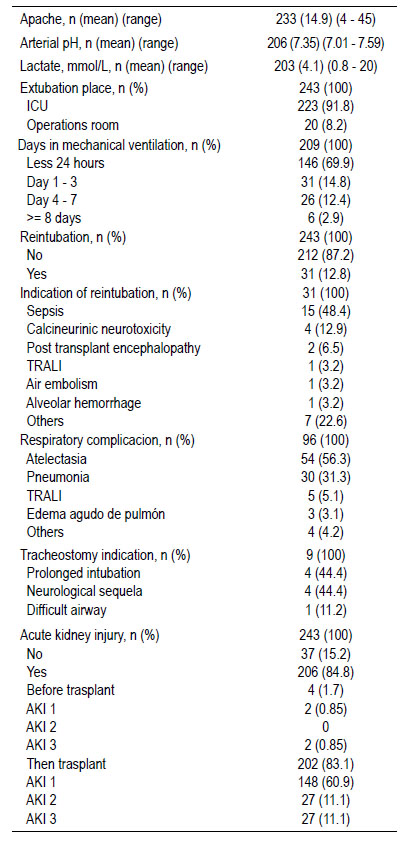
APACHE admission: 14.9 points (ranges: 4 - 25 points). ICU admission pH: 7.35 (ranges: 7.01 - 7.59) Lactate admission to ICU: 4.1 mmol / L (ranges: 0.8 - 20 mmol / L). ICU extubation: 223 (91.8%) patients and fast track (OR): 20 (8.2%). Mechanical ventilation time: < 24 hours: 146 (69.9%) patients; 1-3 days: 31 (14.8%); 4-7 days: 26 (12.4%). Maximum: 25 days. Average stay in ICU was 7.8 days, minimum 1 day and maximum: 62 days. Readmissions to ICU: 7 patients (2.9%). Tables 4 and 5.
ICU Complications:
Reintubation: 31 (12.8%) patients due to septic shock: 15 (48.4%) and calcineurin inhibitors related severe neurotoxicity: 4 (12.9%). Table 4.
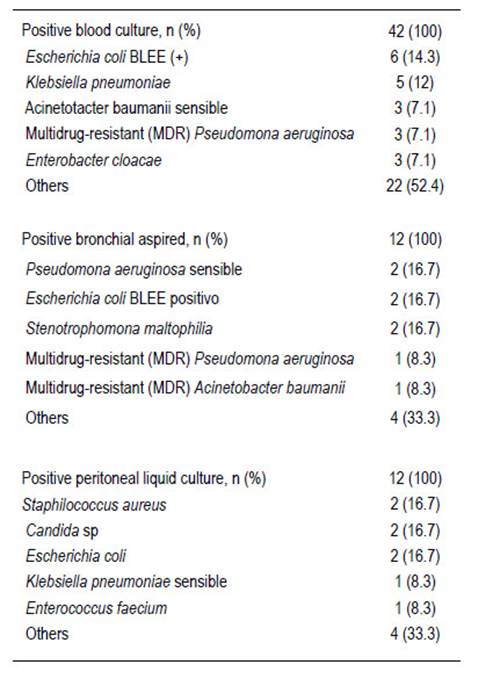
Respiratory complications: atelectasis: 54 (56.3%), pneumonia: 30 (31.3%), TRALI: 5 (5.1%), acute lung edema: 3 (3.1%). Tracheostomy: 9 patients (prolonged intubation: 4; 44.4%), neurological sequela: 4 (44.4%) and difficult airway: 1 (11.2%). Acute renal injury: 206 (84.8%) patients; preLTx: 4 (1.7%) and post transplantation in 202 (83.1%). AKI-1 post-transplant: 148 (60.9%), AKI-2: 27 (11.1%) and AKI-3: 27 (11.1%) with hemodialysis. Neurological complications: calcineurin neurotoxicity: 43 (47.8%) patients, post- transplant encephalopathy: 18 (20%) patients. Antibiotic prophylaxis: 82 monotherapy (39.2%), double therapy: 127 (60.8%). Antibiotic scheme: Ampicillin - Sulbactam: 88 (39.6%) patients, Piperacillin-Tazobactam: 65 (29.3%), Meropenem: 61 (27.5%). Culture results: Escherichia coli ESBL (+): 6 (14.3%) patients, Klebsiella pneumoniae 5 (12%) patients. Table 6.
Immunosuppression:
Immunosuppressive induction: Basiliximab: 109 (44.9%). Maintenance therapy: Tacrolimus 216 (88.9%) patients.
DISCUSSION
Liver transplantation is the standard treatment for end-stage liver disease, that affects all organs in different forms and intensity and, after an optimal postoperative period, multisystem functionality should be resolved. The optimal monitoring and management in the operating room and in the Intensive Care Unit is essential and transcendental since the use of marginal donors of our country is increasing, in addition to the multi-organ commitment of the recipient that is not reflected in the MELD score. An early evaluation and recognition of the different organ complications is essential in the ICU since it has an impact on the structure and functionality of the graft and, therefore, on the morbidity and mortality of the patient.
Although no single factor is responsible, advances in surgical and anesthetic techniques, a better understanding of liver physiology, and improved perioperative management have contributed 6. Most of the postoperative management problems after liver transplantation are unique and require a broader understanding of liver metabolism and the pathophysiology of liver disease 6.
The etiology of liver transplantation in our experience was predominantly NASH (35%), autoimmune hepatitis (15.3%) and ASH (11.5%), in comparison with other experiences 7, a North American study of 5 years where it shows that its most frequent incidence in recent years was ASH (40.3%), NASH (33.9%) in patients without hepatocarcinoma and that the most frequent incidence in patients with hepatocarcinoma was HCV infection (35.9%, although decreasing due to the new regimens of direct-acting antiviral agents), followed by NASH (34.7%). In this same study, the mean age was 56.8 years and the female sex represented 34.8%, in comparison with our study that the average age was 53 years and the female sex had a similar percentage of 35.4%. In a similar Brazilian study 8, the most frequent aetiology of transplantation was ASH (31%), HCV (20.2%), NASH (14%), in this same study CHILD - B was the most frequent with 44.2%, compared to ours, which was CHILD - C with 53.1%. Regarding the MELD on the waiting list, they had an average of 21.6 points and, in our study, it ranged between 15 - 20 points (47.8%). The incidence of hepatopulmonary syndrome was 8.23% in our entire series, a similar percentage to the study carried out in the same series but with a lower number of transplants 9, where the incidence was 9.45%. Severe hepatopulmonary syndrome was the most frequent in our study (50%) compared to another study where it was only 16.7% 10.
Regarding the intraoperative parameters, the mean blood pack transfusion was 9.3 units, compared to the mean of 8.1 blood pack units 11.
The average APACHE in our study was 14.9%, similar to other study 6, who had an average of 13.8%, which may or may not be associated with the mortality rate according to the studies reviewed.
In our study, 69.9% of the patients were extubated in the first 24 hours, compared to 75.5% in early extubation (12. According to other center 13, the average number of hours on mechanical ventilation was 22 hours and the percentage of patients without post- operative respiratory failure was 20% 13. In addition, 6% of the patients required mechanical ventilation equal to or greater than 8 days, a figure compared with ventilatory support between 7 - 30 days after transplantation, in 7% 14.
A round a quarter (25.7%) of the transplanted patients presented post reperfusion syndrome, a result consistent with other studies 15. This syndrome was defined as a decrease in mean arterial pressure greater than 30% of the value observed in the anhepatic phase, for more than 1 minute during the first 5 minutes after reperfusion of the graft 16, using the Piggy Back Technique, the factors associated with this syndrome are not entirely clear, but intraoperative hemodynamic changes influence the postoperative morbidity of liver transplantation 16,17.
Nosocomial pathogens include gram negative and gram positive bacteria, the intensity, exposure time and virulence of the pathogen affect mortality and morbidity 18. There are no recent data to know the incidence of colonization and infection by ESBL- producing gram-negative organisms. It seems likely that there is a significant variation worldwide in its prevalence, multidrug-resistant bacteria and Burkhodelia cepacia have been less studied and their incidence varies according to the geographical area 19. Given the potential for serious infection-related complications in this population, it is essential to identify patients at risk and provide appropriate treatment in a timely manner.
In a main center of France 20, found a two times higher risk of fungal infection in liver transplant recipients who had a MELD score between 20 and 30 and a four times higher risk in those with a MELD score > 30. Although the spectrum of Infection varies by region and between centers, infections caused by gram-negative bacteria are generally the most common, causing 50-70% of bacterial infections, although nearly a third of infections can be polymicrobial 21. Common organisms include Escherichia coli, various species of Pseudomonas, Klebsiella, Acinetobacter, and Enterobacter; as well as gram-positive organisms such as Staphylococcus aureus and Enterococcus species. Our results show a similar prevalence to previous reports. As with other high-risk populations, multidrug resistant (MDR) organisms are becoming more prevalent after liver transplantation with higher mortality than drug-susceptible infections. With targeted prevention, prophylaxis, and monitoring before and after transplantation, many infections can be prevented or identified early, allowing for the rapid initiation of appropriate therapy.
The length of stay in the ICU was 7.8 days in our study, compared with 8.8 days in other study 22, related to arterial lactate of 4.1 mmol/L. In our study lactate was 2.7 mmol/L related to bleeding in the operating room, in our study 6393 ml, compared with 4550 ml in the aforementioned study.
Our results show the experience of the most important liver transplant center in Peru. Many factors will determine the final outcome of a patient after a liver transplant, be it a short or long stay in the ICU, the need for intensive support in the pre-transplant, medical surgical complications, as well as the provision of high quality care in the ICU, a key element of the hospital infrastructure necessary to deliver excellent results.