INTRODUCTION
Acute cholecystitis is a frequent cause of abdominal pain and one of the most important causes of admission to emergency units globally. Stones are the leading cause of acute cholecystitis, and cholecystectomy is the first-line treatment for this entity for the majority of patients 1.
Occasionally, cholecystectomy is not possible because the patient is not suitable for surgery, and non-operative management should be performed 2.
In the group of non-operative management are the percutaneous transhepatic gallbladder drainage (PTGBD) and the endoscopic gallbladder drainage.
On the other hand, endoscopic techniques are subdivided into endoscopic transpapillary gallbladder drainage and ultrasound-guided transmural gallbladder drainage (EUS-GBD). Recent studies mention that EUS-GBD with lumen-apposing self-expandable metal stents (LAMS) should be preferred to endoscopic transpapillary gallbladder drainage 3, where it was found that technical and clinical success were higher with the transmural access and also appears to be safe and feasible than transpapillary technique 4-6.
In the present study, we decide to compare the efficacy and safety of PTGBD and EUS-GBD in the non-operative management of patients with acute cholecystitis.
METHODS
Literature search and data selection criteria
We conducted a systematic review in different databases, such as PubMed, Cochrane, Medline, and OVID Database. A search was made of all studies published up to August 2021. Only those studies that are in English- language were considered for the search. The next following entries were assessing using Boolean operators: “gallbladder drainage”, “endoscopic ultrasound”, “EUS guided gallbladder drainage”, “endoscopic ultrasound gallbladder drainage”, “ultrasound-guided transmural gallbladder drainage”, “percutaneous drainage”, “percutaneous transhepatic gallbladder drainage”, “cholecystitis”, “acute cholecystitis”, “calculous acute cholecystitis”, and “acalculous acute cholecystitis”.
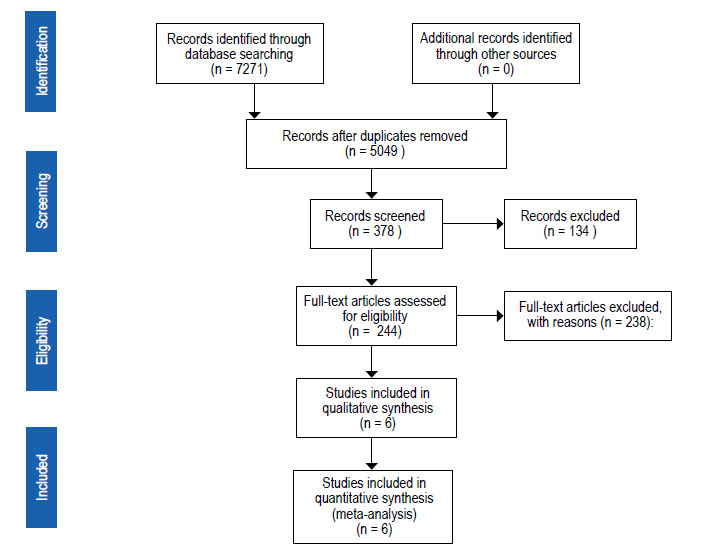
We excluded those publications that analyzed only the efficacy of endoscopic gallbladder drainage or the percutaneous transhepatic gallbladder drainage separately. Studies in which the techniques mentioned earlier were compared with transpapillary endoscopic drainage were not considered. Studies with other techniques for gallbladder drainage, review articles, other meta-analyses, case reports, duplicates, redundant data, book chapters, editorials, commentaries, abstracts, non-relevant publications, or incomplete analysis were excluded for the present pooled-data analysis (Figure 1). All reviewers fully agreed with the selection and analysis of the studies.
Statistic methods ana data analysis endpoints
The primary endpoints computed were technical success rate, clinical success rate, and adverse events (AEs) rate for EUS-gallbladder drainage and PTGBD. Technical success was defined as successful transgastric or transduodenal stent placement during the endoscopic procedure. On the other hand, clinical success was defined as significant improvement or relief of symptoms evidenced during follow-up after the gallbladder drainage. Adverse events were defined as complications related to the endoscopic procedure.
Data extraction
To confirm study eligibility, we reviewed the full texts of the six selected articles. To extract the data selected, we design a table for data extraction from each study. The main variables selected were: country, author, year of publication, study design, age and gender of patients, number of patients in each study, number of procedures where EUS-GBD was performed, number of procedures where PTGBD was performed; the technical and clinical success of each technique; and finally, the adverse events for each method and the follow-up time of the patients.
Risk of bias assessment
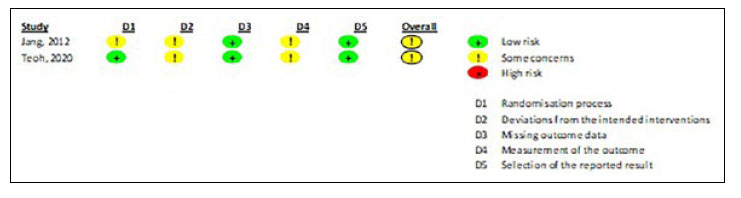
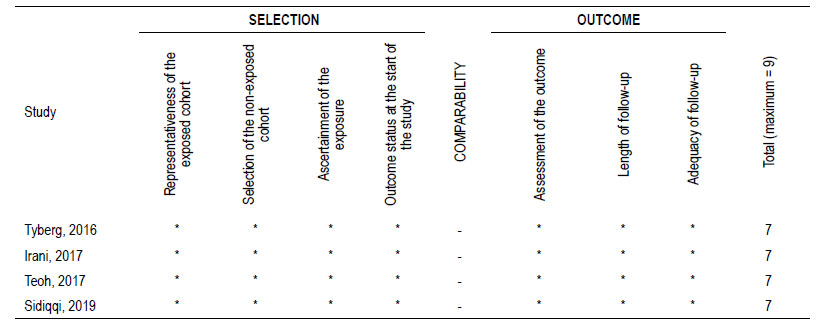
The risk of bias of randomized controlled trials (RCTs) was assessed using the Risk of Bias (RoB) 2.0 tool. Each RCT was classified as having a low risk of bias, some concerns, and a high risk of bias. Cohort studies were evaluated using the Newcastle-Ottawa Scale (NOS). Each study was scored as follows: low risk of bias (8-9 points), moderate risk of bias (5-7 points), and high risk of bias (0-4 points). (Figure 2 and Table 2)
Statistical data analysis
All meta-analyses were performed using an inverse- variance random-effects model. The Paule-Mandel method was used to estimate the between-study variance (Tau2). All outcomes were pooled using risk ratio (RR) with its 95% confidence interval (CI). Heterogeneity was assessed using the chi-squared test (threshold p<0.10) and the I2 statistic. Heterogeneity was defined as low if I2<30%, moderate if I2 is 30%- 60%, and high if I2>60%. Subgroup analyses were performed according to the study design (RCT versus cohort). The interaction test (threshold p<0.10) was used to evaluate the difference between subgroups. Publication bias was assessed only if ten or more studies were available. We used the meta-package from R 3.6.3 (www.r-project.com) for all meta-analyses. A two-tailed p<0.05 was considered statistically significant.
RESULTS
Characteristics of included studies
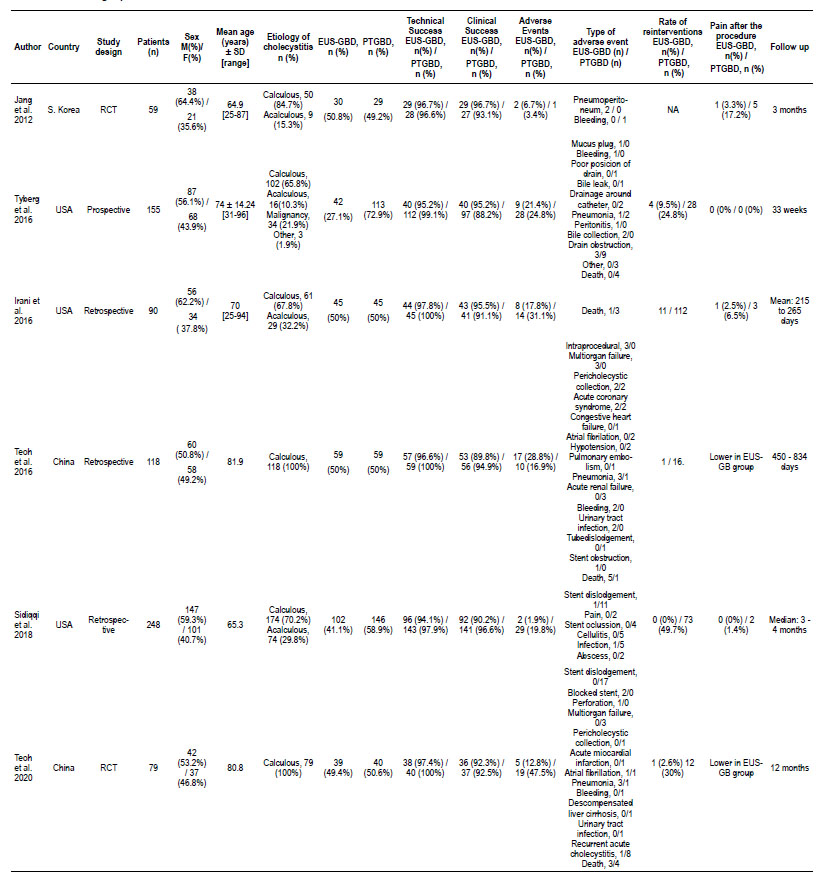
In Figure 1, we described the search and selection process in a flow diagram. The initial search yielded 7271 articles, of which six studies were selected and analyzed [7-12]. Of these six studies, two were randomized controlled trials (RCTs) (7, 12), the remaining four studies were retrospective 8-11. Three studies were conducted in the USA [8, 9, 11], two in China [10, 12], and one in South Korea [7]. Table 1 lists the features and distribution of the thirteen studies included.
Demographic features
All six studies included a total of 749 patients. The mean age in all six studies was 72.81 ±7.41 years; Of 749 patients, 57.4% were male (430 patients), and 42.6% were female (319 patients). Three hundred seventeen patients (42.3%) underwent EUS-GBD, and 432 (57.7%) underwent PTGBD.
Aetiology of cholecystitis
In five hundred and eighty-four of the 749 patients (77.9%), the aetiology of the cholecystitis was calculous and in 128 patients (17.1%) was acalculous. Only one study [8] considered 34 patients with malignant aetiology in its data (4.5%)
Technical success
In six studies (n=749), the use of EUS-GBD was associated with a lower technical success than PTGBD (RR, 0.97; 95% CI, 0.95-0.99; I2=0%).
Considering only RCTs, the use of EUS-GBD has similar technical success compared to PTGBD (RR, 0.98; 95% CI, 0.94-1.02; I2=0%). In contrast, considering only cohort studies, the use of EUS-GBD was associated with a lower technical success than PTGBD (RR, 0.97; 95% CI, 0.94-0.99; I2=0%). However, the interaction test (p=0.64) was not significant. (Figure 3)
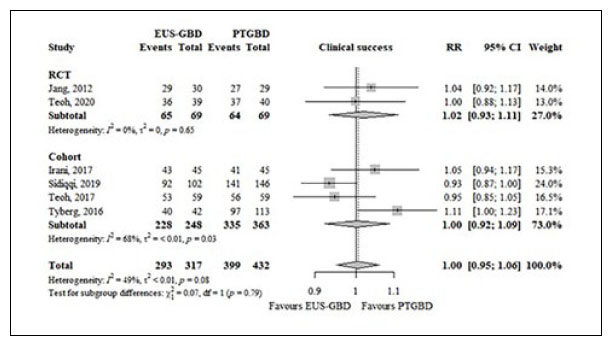
Clinical success
In six studies (n=749), the use of EUS-GBD has similiar clinical success compared to PTGBD (RR, 1.00; 95% CI, 0.95-1.06; I2=49%).
Considering only RCTs (RR, 1.02; 95% CI, 0.93-1.11; I2=0%) or cohort studies (RR, 1.00; 95% CI, 0.95-1.06; I2=68%), the use of EUS-GBD has similar clinical success compared to PTGBD. The interaction test (p=0.79) was no significant. (Figure 4)
Adverse events
The total adverse events are listed in Table 1. In six studies (n=749), the use of EUS-GBD has similar adverse events rate compared to PTGBD (RR, 0.58; 95% CI, 0.25-1.35; I2=74%).
Considering only RCTs (RR, 0.53; 95% CI, 0.08-3.29; I2=58%) or cohort studies (RR, 0.60; 95% CI, 0.19-1.84; I2=78%), the use of EUS-GBD has similar clinical success compared to PTGBD. The interaction test (p=0.91) was no significant. (Figure 5)
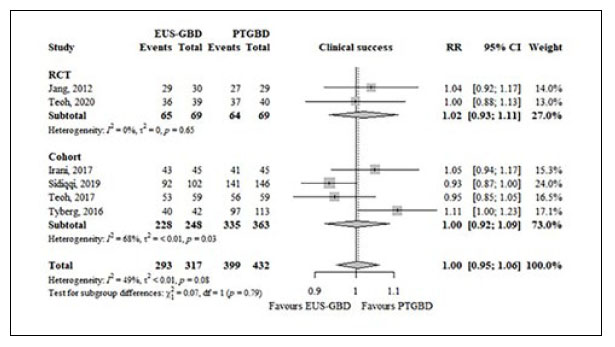
Figure 5 Forest plot showing the effect of EUS-GBD compared to PTGBD on adverse events. Abbreviations: EUS-GBD, ultrasound-guided transmural gallbladder drainage; PTGBD, percutaneous transhepatic gallbladder drainage; RR, risk ratio; CI, confidence interval.
Twenty-one deaths were reported in all six studies. The global mortality rate was 2.80%, without differences in both groups. The mortality rate in the group that underwent EUS-GBD was 2.84%, whereas in the groups that underwent PTGBD was 2.77%.
DISCUSSION
In some cases, acute cholecystitis cannot be treated with surgery 9-11, resulting in significant morbidity and mortality rates in high-risk patients 12-14. Currently, there are other methods to replace cholecystectomy. These forms to treat the non-tributary patients without surgery can be with endoscopic or percutaneous approach 2. PTGBD is a radiologic procedure with a 56% to 100% clinical response in different studies 15-16; however, this method is not free of complications, such as peritonitis, bleeding, and pneumothorax, bile leak, subcapsular hematoma, pain, and catheter migration 17. The adverse events of PTGBD are reported around 12% to 14% in some studies 18-21. Patients with coagulopathy and massive ascites can have some risk when they are undergoing PTGBD. It is the reason why endoscopic procedures can result in an excellent alternative to treat patients with acute cholecystitis with high surgical risk. The endoscopic approach for gallbladder drainage is possible with transmural access through EUS (transgastric or transduodenal access). A previous systematic review reported high success rates (up to 96%) with a low rate of adverse events (5.5%) 22.
Our meta-analysis showed that EUS-GBD has a significantly lower technical success rate than PTGBD (RR, 0.97; 95% CI, 0.95-0.99; I2=0%). However, when only RCTs were analyzed independently, this statistical difference disappeared. We should consider that the transmural approach requires adequate expertise and training. In addition, endoscopic access technically appears more complex than percutaneous access. EUS-GBD has a high technical success rate (95.9%); even though there is a statistical difference with the PTGBD technical success rate, we consider that this procedure is a valid method for treating patients with acute cholecystitis who can not be undergoing surgery.
The clinical success rate was similar in both groups (94.3% in the EUS-GBD groups and 92.4% in the PTGBD group). None of all six studies showed a statistical difference independently; however, the heterogeneity for this analysis was moderate (I2 = 49%). It is essential to highlight that the adverse events rate did not differ between the groups, 13.6% and 23.4% in the EUS-GBD group and PTGBD group, respectively (RR, 0.58; 95% CI, respectively 0.25-1.35; I2=74%).
When only RCTs were considered in the analysis, this trend continued. The type of adverse event was variable in the different studies. Tyberg et al. [8] showed that drain obstruction was the most frequent complication in the percutaneous approach. In contrast, the stent dislodgment was the most common complication in the study of Teoh et al. 12, reaching up to 17 patients. The global mortality rate was 2.8% and was similar between both groups. The mortality rate in the group that underwent EUS-GBD was 2.84%, whereas in the groups that underwent PTGBD was 2.77%. Only two of the six studies did not report deaths 7,11.
In our study, it was not possible to perform an analysis about postprocedure pain. Only three of the six studies 7,9,11 showed exact data, but the remaining three studies only report general data, being the postprocedure pain consistently lower In the EUS-GBD. The reinterventions rate was reported in five studies (8 - 12), which was higher in the PTGBD group. These are other good reasons to choose the endoscopic approach to perform a cholecystostomy in patients whose surgical treatment is not possible.
It is essential to mention that some studies comparing PTGBD with endoscopic techniques were excluded in our meta-analyses. For example. Kedia et al. 23 reported that the endoscopic approach was superior in terms of long-term efficacy and tolerability to PTGBD. This study was excluded because the endoscopic procedure was transpapillary mainly. The EUS-GBD only was performed in six patients, and the features and results in this small group were not detailed.
Our study has some limitations. We should recognize that the total of included studies was small. Six studies were included, and only two of them were RCTs. The remaining four studies were retrospective. On the other hand, we believe that this metanalysis has an advantage: the selection of the different studies is more strict, and the fact that only comparative studies are included help to reduce the heterogeneity and selection bias.
Despite the theoretical similarity between EUS-GBD o PTGBD in treating acute cholecystitis, we believe that more randomized controlled studies are needed to corroborate this data.
CONCLUSION
EUS-GBD and PTGBD were successful techniques for gallbladder drainage in patients with acute cholecystitis who are non-tributary for surgery. EUS-GBD has a similar clinical success rate and a similar adverse events rate to PTGBD. The high technical success and the low adverse events rate of the EUS approach to gallbladder make this technique an excellent alternative for patients with acute cholecystitis who cannot be undergoing surgery.
Author’s Contribution: Edson Guzman-Calderón: Is the corresponding author: conception and design, acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version to be published. Carlos Díaz: methodological and statistical analysis, interpretation of data. Alfonso Chacaltana, Ramiro Díaz, Ronald Arcana, and José Ramón Aparicio: analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version to be published.