INTRODUCCIÓN
Typhlitis, is also known as neutropenic enterocolitis, affects the cecum and distal ileum. It was frequently described in pediatric patients undergoing treatment for leukemia. Nonetheless, it can affect adult patients, regardless of the cause of the immunosuppression. This entity has been described in HIV infection, treatment for rheumatological diseases, neoplasms, organ transplants 1. The exact pathophysiology of the disease is not known, but it is suggested that it is the result of bacterial translocation due to a friable intestinal mucosa 2.
The incidence of the illness in our population is not known, however, a cohort study refers to a 3.5% incidence in severe neutropenic patients 3, although it can vary from 1.75 to 16.2% in the different series of the pediatric population 4.
Typhlitis can be found in any age group; however, the most frequently affected group is between 4 to 10 years old with a male/female ratio of 1.7/1. (5, 6)
Gastrointestinal bleeding associated with Neutropenic Enterocolitis is one of the most feared complications, with very few reports cited in the literature. 7-9.
We present the case of a patient with osteosarcoma who develops Neutropenic Enterocolitis and subsequently presenting a lower gastrointestinal bleeding responding to conservative management.
CASE REPORT
A 20-year-old male patient with a history of osteoblastic osteosarcoma located in the right proximal tibia, which was diagnosed 8 months prior to his hospital admission, underwent conservative surgery after the second cycle of neoadjuvant treatment. He received a scheme according to the EURAMOS 1 program (Methotrexate, Doxorubicin, Cisplatin).
When the patient was undergoing his fifth cycle of treatment (Cisplatin/Doxorubicin), he was evaluated in the emergency department with a 6-day history of nausea and vomiting, fever sensation and diarrhea (6 episodes a day on average). Two days before admission, he complained of diffuse abdominal pain (subjective intensity 9/10).
He was oriented in time, place and person, HR 122 x‘, BP 70/40mmhg. The abdomen was distended, bowel sounds were absent, with marked tenderness to palpation on lower quadrants predominantly in the right iliac fossa. The rest of the physical examination was unremarkable.
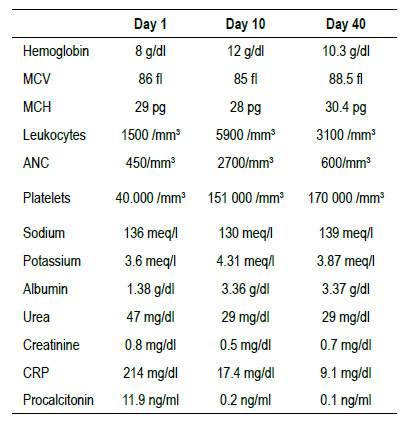
Laboratory tests showed moderate anemia with leukopenia and severe neutropenia, as well as thrombocytopenia, severe hypoalbuminemia, and mild hypokalemia. Blood cultures were negative, as were glutamate dehydrogenase and PCR tests for clostridium difficile (Table 1).
The abdominal CT scan showed edema of the walls of the ascending colon and cecum, with a cecal wall width of 8.24 mm, (Figure 1). There was also small bowel distension with edema, predominantly in the ileal region, and abundant peritoneal fluid. The cecal appendix had no alterations.

Figure 1 Computed tomography of the abdomen and pelvis with contrast showing the thickness of the cecum wall (8.24 mm). Distention of small bowel loops associated with wall edema, predominantly in the ileal region and presence of free fluid in the abdominal cavity.
The patient was initially treated with vasopressor support, potassium replacement, packed red blood cells and platelet transfusion, granulocyte colony- stimulating factor, bowel rest, and parenteral nutrition. Broad-spectrum antibiotic therapy was administered (Meropenem + Vancomycin + Metronidazole). Antifungal therapy with Voriconazole was added on the third day because of persisting fever.
The patient’s clinical course was favorable. From hospital day 7, he was hemodynamically stable, afebrile, and his abdomen was non tender and with normal bowel sounds. On day 10, oral tolerance with clear liquids was started.
On day 13 of hospitalization, the patient presented episodes of melena with a drop in hemoglobin. Because of the thrombocytopenia, endoscopic procedures were deferred, and a tagged red blood cell scintigraphy with 99 Tc was obtained (Figure 2), showing diffuse uptake in the left flank region, compatible with active bleeding. We opted for a conservative management approach with hydration and blood transfusions. On day 16, there were no new episodes of melena or a drop in hemoglobin.
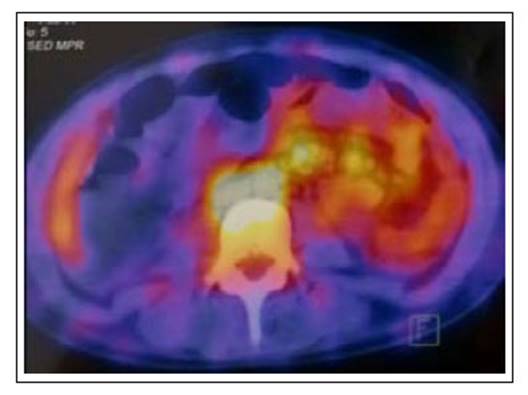
Figure 2 Tagged blood cell scintigraphy shows uptake of the radiotracer in thin intestinal loops of the left flank in relation to active digestive bleeding.
The patient evolved favorably, tolerated diet, remained afebrile and had no abdominal pain, being discharged on day 20.
The abdominal CAT scan performed one month later was completely normal (Figure 3).
DISCUSSION
The suspected diagnosis of typhlitis requires a correct anamnesis which includes the patient’s current medication, as well as important information including immunosuppression 10.
The clinical picture of neutropenic enterocolitis is that of an acute abdomen, with pain in the right lower quadrant of the abdomen in most cases, associated with an increase in body temperature, diarrhea -which may be bloody-, nausea, vomiting, bloating and signs of peritoneal irritation. Likewise, patients may experience hypotension, decreased bowel sounds, and sometimes palpable mass in the right iliac fossa 11.
Plain abdominal radiography can show dilatation of the small bowel loops, fluid in the ascending colon, pneumatosis, and dilatation of the cecum; however, these findings lack adequate sensitivity and specificity, limiting its use 12.
The ultrasound can show changes, such as thickening of the intestinal wall in combination with other findings like fluid accumulation, increased echogenicity of the mesenteric fat enlarged lymph nodes, and hyperemic changes 13.
In a series of cases assessing the ultrasound findings in 14 patients with Neutropenic Enterocolitis, it was found that 11 patients had ascites, in addition to the previously mentioned characteristics 14.
CT findings suggestive of typhlitis are mural concentric thickening of the cecum with extension to the ascending colon and ileum, peri colonic inflammation, adjacent fat stranding intestinal pneumatosis and ascites 15.
The findings of the anamnesis and physical examination should be supported with a CT with intravenous contrast, the imaging test of choice, which helps excluding other differential diagnoses, such as pseudomembranous colitis, inflammatory bowel disease, appendicitis, ischemic colitis, intestinal tuberculosis 12.
A case-control study proposed diagnostic criteria for the identification of patients with Neutropenic Enterocolitis, which have been met in this case report. Those are Neutropenia < 500/mm3, fever > 38 degrees, wall thickness (ultrasound or CT) more than 4 mm, and abdominal pain. 16
Patients with neutropenic enterocolitis can present different degrees of neutropenia. In the study by Bautista it was observed that 80% of cases of neutropenic enterocolitis presented severe neutropenia (Less than 500 mm3), 15% moderate neutropenia (Less than 1000 mm3) and the remaining 5% mild neutropenia (Less than 1500 mm3) 5. The changes in platelet count, electrolyte disorders, bilirubin, hemoglobin are nonspecific and do not contribute to the diagnosis; however, it is extremely important to correct these alterations 11.
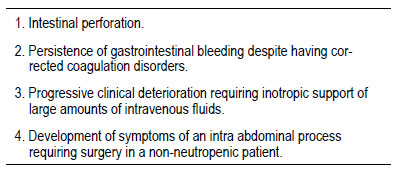
Intestinal perforation.
Persistence of gastrointestinal bleeding despite having cor- rected coagulation disorders.
Progressive clinical deterioration requiring inotropic support of large amounts of intravenous fluids.
Development of symptoms of an intra abdominal process requiring surgery in a non-neutropenic patient.
Sloas et al. observed that only 33% of the patients presented bacteremia. The pathogens isolated in the study were Escherichia coli, Klebsiella pneumoniae, Pseudomona aeruginosa, Enterobacter taylorae, Morganella morganii, and Streptococcus viridans 11.
The mainstay of treatment of this condition is supportive care, leaving the surgical option for severe complications such as intestinal perforation. The Shamberger criteria are useful to determine the need for surgical treatment 17. (Table 2)
Medical treatment includes hemodynamic stabilization of the patient, correction of fluid and electrolyte disorders, bowel rest, and broad-spectrum antibiotic therapy. Antibiotic therapy should include coverage for gram negative bacilli, gram positive cocci, anaerobes, since the infection is usually polymicrobial. Cover against fungi is suggested if there is no improvement 72 hours after starting treatment 18, which was the case of our patient.
Regarding the use of granulocyte colony stimulating factors (G-CFS), it is not routinely recommended in those patients with uncomplicated febrile neutropenia; however, it can be prescribed in patients who are at high risk for complications related to infection. These include patients with an absolute neutrophil count <100 / ml, uncontrolled primary disease, pneumonia, hypotension, multi-organ dysfunction, and fungal infection 19.
There are currently no clinical guidelines on the management of neutropenic enterocolitis, however bowel rest and total parenteral nutrition are recommended in most seriously ill 20.
Possible complications can be intestinal perforation, peritonitis, septic shock, abscess formation and even hypovolemic shock due to lower gastrointestinal bleeding 21.
In a case series from 1970 to 1987, 35 cases of Typhlitis were reported at Texas Children’s Hospital. Of these patients, 13 developed gastrointestinal bleeding, which was considered a complication with a poor prognosis 6.
Some patients responding to conservative management like ours in the setting of neutropenic colitis and gastrointestinal bleeding have been reported; However, if the bleeding persists, it is recommended to use interventional radiology techniques, as in the case published by Meyerovitz et al., in which they performed a successful embolization of the ileocolic artery 8. Lister et al reported a successful treatment with embolization of the superior mesenteric artery in a patient with typhlitis and cecal bleeding. 9
Shamberger criteria mentioned above include persistence of gastrointestinal bleeding refractory to correction of coagulation disorders. However, patients admitted to surgery have associated comorbidities that could increase the perioperative mortality rate 7, which can be up to 50%, especially when associated with intestinal perforation 20.
One study reported the relationship between the thickness of the intestinal wall and the mortality rate in patients with neutropenic enterocolitis, being 60 % in those with a thickness > 10 mm compared to 4.2 % in those with a thickness ≤ 10 mm 22.
CONCLUSION
Neutropenic enterocolitis or typhlitis should be suspected in all patients who develop neutropenia after chemotherapy and who present gastrointestinal symptoms such as nausea, vomiting, diarrhea, and severe abdominal pain. Undoubtedly the diagnosis is based on abdominal CAT scan. Early diagnosis and treatment help improve the prognosis of this severe complication.
Gastrointestinal bleeding is an expected complication in this setting, for which conservative management, which involves correction of coagulopathy, red blood cell transfusion, and volume repletion, may be the appropriate treatment in patients who do not have hemodynamic instability and manage to control bleeding. If gastrointestinal bleeding persists, interventional radiology embolization and surgery are alternatives for management.