INTRODUCCIÓN
Barrett's esophagus (BE) is characterized by the replacement of stratified squamous epithelium by columnar epithelium with the presence of intestinal metaplasia in the lower esophagus. BE can progress to dysplasia and is a known precursor of adenocarcinoma. Rarely, dysplasia and adenocarcinoma can be found with an extensive polypoid appearance in a context of BE, and most of these cases are diagnosed on advanced stages at presentation. For this reason, most of protruded lesions are managed surgically. We report a case of polypoid early neoplasia in BE esophagus, managed by endoscopic submucosal dissection (ESD).
CASE REPORT
A 71-year-old male, with history of chronic gastroesophageal reflux disease, was referred due to the presence of a large polypoid lesion in BE esophagus. An upper endoscopy was performed and revealed mucosal changes consistent with long-segment BE (C5M9 per Prague criteria) and a 25 mm pedunculated lesion (Figure 1A). Due to the presence of abundant fibrin on the surface of the lesion, it was not possible to determine the mucosal or vascular pattern. Endoscopic ultrasound (EUS) showed no lymph nodes invasion. After a multidisciplinary meeting and discussing with the patient the pros and cons of each of the therapeutic possibilities, it was decided to perform an endoscopic resection to allow accurate diagnostic staging. The polypoid lesion was resected en bloc by ESD, without complications (Figure 1B). Histological analysis revealed extensive polypoid high-grade dysplasia with a focus of intramucosal adenocarcinoma restricted to the lamina propria with free margins (Figure 2A and 2B). The resection was considered curative, and the patient was discharged for posterior radiofrequency ablation. No evidence of recurrence was observed in endoscopic controls.
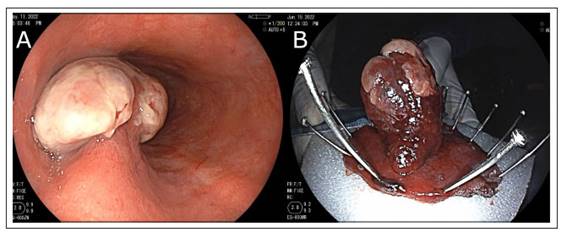
Fig. 1 (A) Barrett esophagus with an extensive polypoid lesion of 25 mm obstructing the lumen covered with fibrin. Due to the presence of abundant fibrin on the surface of the lesion, it was not possible to determine the mucosal or vascular pattern. (B) Resection of the lesion.
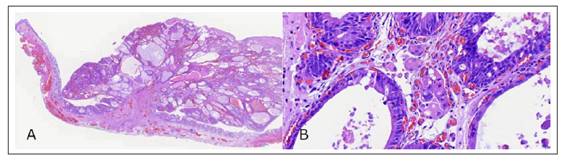
Fig. 2 Histological analysis. (A) Low-power view of the resected specimen shows a pediculated lesion over a mucosa of Barrett esophagus (hematoxylin & eosin stain). (B) High-power view reveals high-grade dysplasia with a focus of intramucosal adenocarcinoma restricted to the lamina propria (hematoxylin & eosin stain).
DISCUSSION
Recent advances in endoscopy have allowed to change the management of superficial adenocarcinoma in BE from major surgery to minimally invasive endoscopic resections. Predicting the risk of lymphatic invasion is essential when selecting candidate patients for endoscopic resection 1,2. T1a esophageal adenocarcinomas are associated with a better survival than advanced neoplasia, mainly due to the lower risk of lymph node involvement (<4% risk of nodal involvement 3 and current guidelines recommend endoscopic resection as the preferred treatment for early esophageal cancers 1,2.
Endoscopic options to predict the level of invasion include EUS and endoscopic resection. EUS is the preferred non-histologic method to assess depth of invasion, but is more appropriate for staging more advanced neoplasia than T1 disease, and endoscopic resection remains the most accurate tool for staging in early esophageal cancers4.
In addition to the level of invasion, there are other factors that influence the risk of lymph node involvement like tumor size, grade of differentiation, and presence of lymphovascular invasion5. These features must be considered when we choose between performing an endoscopic resection or surgery.
Several techniques were developed for endoscopic resection including endoscopic mucosa resection (EMR) and ESD. EMR is a simpler technique and allows resections of small lesions (1 - 2 cm)6). However, in case of larger lesions, ESD permits en bloc resection giving the opportunity of clear histological assessment of deep and circumferential margin(7). Despite the advantage of ESD, this technique requires a long learning curve to be safely performed and more specialized endoscopic tools than EMR.
Esophagectomy is a major surgery associated with high mortality8, therefore, in cases of intramucosal adenocarcinoma is advised to perform and endoscopic resection before proceeding directly to surgical resection9. Even in cases of T1b lesions, endoscopic resection can be curative if the risk of lymph node invasion is acceptably low. However, we will not always be able to have an exact prediction of the level of invasion, even performing an EUS.
It has been described that non-protruded lesions are more commonly found and that protruded appearance of the lesion is related to overstaging of superficial esophageal cancer4. The protruding lesion can obstruct the esophageal lumen and gives a more advanced image at the time of endoscopy. In addition, the size of the lesion will disturb adequate compression of the esophageal wall, preventing adequate penetration of the soundwave into deeper depth. Furthermore, protruded appearance has been shown to have a higher risk of submucosal invasion than the non-protruded appearance10.
In our case, our patients presented a lesion with a non-typical macroscopic subtype with a relatively extensive size that may suggest the presence of an advanced lesion. However, considering all the factors described, a clinical meeting was held, the risks were discussed with the patient and an endoscopic resection was chosen with diagnostic intention. The final diagnosis was an extensive polypoid high-grade dysplasia with a focus of intramucosal adenocarcinoma with a curative resection. Dysplasia in BE most commonly occurs over a flat lesion, but this case shows a rarely presentation of dysplasia and superficial adenocarcinoma as a polypoid lesion.
There is a certain correlation between the endoscopic macroscopic type and the level of invasion, but this risk is lower in the case of pedunculated lesions than in sessile subtype10. Despite having tools such as EUS and magnified endoscopy for correct preoperative staging, the development of new tools is required for an accurate diagnosis, and in cases in which there is no certainty of advanced lesion, a diagnostic endoscopic resection should be performed that will reveal the final histological staging.
In conclusion, the existence of a protruding lesion in the context of BE does not always indicate the presence of an advanced lesion and adequate staging should be performed, including a thorough endoscopic evaluation or EUS. However, on some cases, assessing the risks that may be associated with surgery, a diagnostic resection with curative potential should be performed, as in our patient.














